

A significant number of people who travel internationally each year will develop a travel-related illness while traveling or shortly after returning. Many illnesses acquired abroad can be identified and treatment initiated in the urgent care setting. This review provides evidence-based guidance for the diagnosis and treatment of the most common presenting symptoms in returning travelers, including fever, diarrhea, and rash. Geographic distributions, incubation periods of pathogens, and comparisons of the clinical and laboratory features of different etiologies are provided to aid in diagnosis, with an emphasis on critical diseases that must not be missed. Specific pharmacological interventions and other treatment strategies are also discussed.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
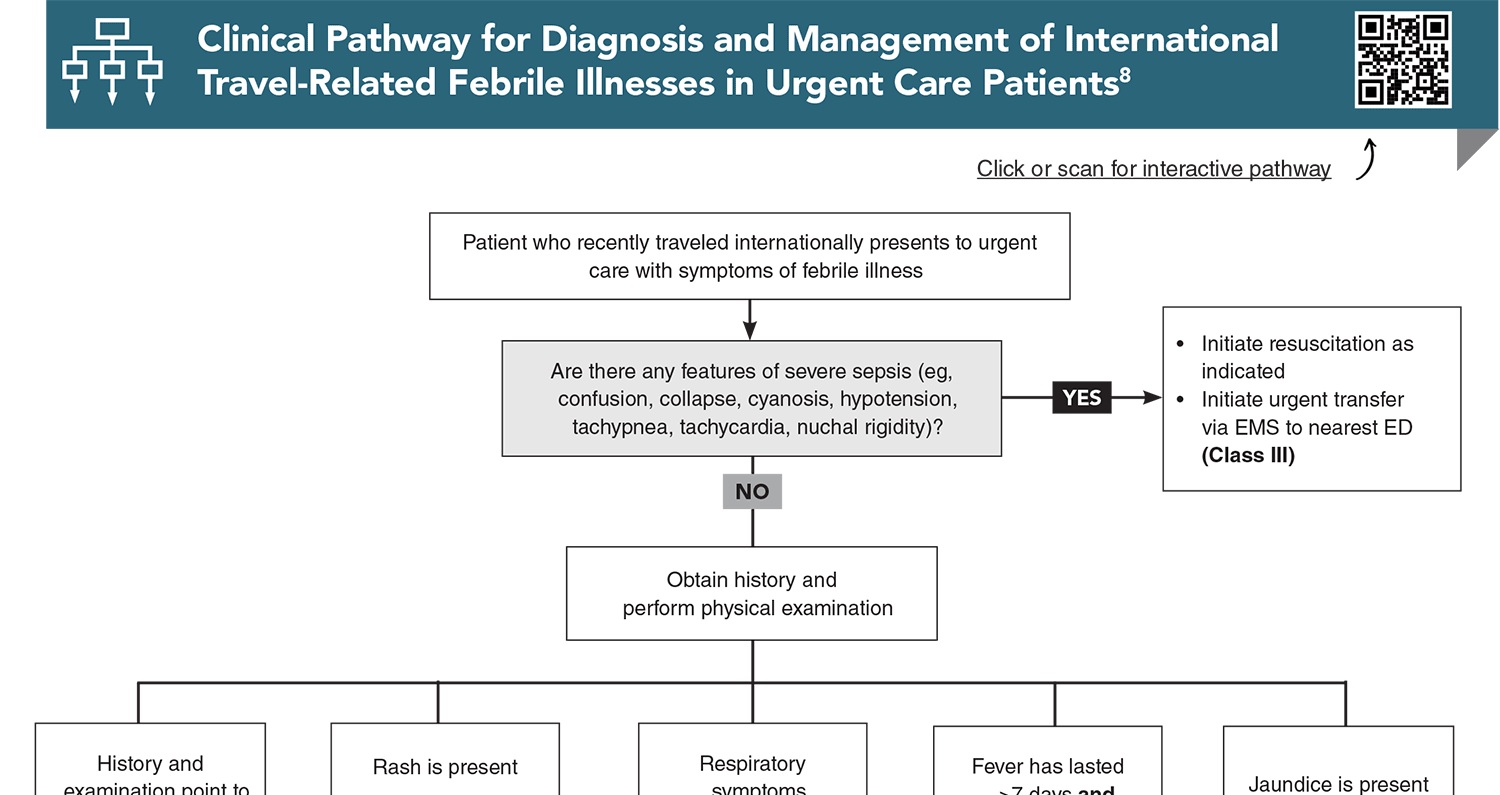
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
4. * Itzkowitz E, Alpert EA, Farojeh AZ, et al. Morbidity of returning travelers seen in community urgent care centers throughout Israel. Trop Med Infect Dis. 2023;8(6). (Prospective observational study; 1580 patients) DOI: 10.3390/tropicalmed8060319
9. * Camprubí-Ferrer D, Cobuccio L, Van Den Broucke S, et al. Causes of fever in returning travelers: a European multicenter prospective cohort study. J Travel Med. 2022;29(2):taac002. (Prospective multicenter cohort study; 765 patients) DOI: 10.1093/jtm/taac002
15. * Heather CS. Travellers’ diarrhoea. BMJ Clin Evid. 2015;2015:0901. (Systematic review; 24 studies) PMID: 25928418
20. * Thakker C, Warrell C, Barrett J, et al. UK guidelines for the investigation and management of eosinophilia in returning travellers and migrants. J Infect. 2025;90(2):106328. (Clinical practice guidelines) DOI: 10.1016/j.jinf.2024.106328
25. * Efstathiadou A, Tsourouktsoglou H, Shipman AR. Skin dermatoses in the returning traveller: a practical guide. Clin Exp Dermatol. 2024;49(11):1289-1300. (Review) DOI: 10.1093/ced/llae114
27. * Beny A, Paz A, Potasman I. Psychiatric problems in returning travelers: features and associations. J Travel Med. 2001;8(5):243-246. (Retrospective cohort study; 15 patients) DOI: 10.2310/7060.2001.24019
Subscribe to get the full list of 35 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: travel, travel-related disease, travel history, returning traveler, international traveler, geographic distribution, “exotic disease”, incubation, infectious agents, chemoprophylaxis, malaria, arbovirus, dengue, chikungunya, Zika, invasive protozoa, parasitic worms, helminths, hepatitis, cholera, dysentery, liver disease, visceral leishmaniasis, contact dermatitis, rash, fever, diarrhea, travelers’ diarrhea, fungal infection, acute respiratory infection, tuberculosis, pulmonary fungal disease, parasitic lung disease, COVID-19, pneumonia, influenza, Shigella, Vibrio, Salmonella, E coli, blood smear, febrile illness, Plasmodium falciparum, P ovale, P vivax, P malariae, P knowlesi, Cryptosporidium, Giardia, trichuriasis, ascariasis, biliary fluke infections, invasive amoebiasis, jetlag, psychosis, delusional parasitosis, schizophrenia, leprosy, rickettsioses, schistosomiasis, histoplasmosis, coccidioidomycosis, tuberculosis, Middle East Respiratory syndrome, enteric fever, viral hemorrhagic fever, strongyloidiasis, artemisinin-based combination therapy, Taenia, Ascaris, hookworm, bedbugs, ticks, mosquitoes, mites, myiasis, fleas, visceral larva migrans, chloroquine
Mark K. Huntington, MD, PhD, FAAFP
Hector M. Cabrera, MD, MPH; Jacqueline M. Vierheilig, MD
October 1, 2025