

Early recognition of stroke in young adults is crucial for effective treatment and mitigation of long-term impact on quality of life. This issue of Emergency Medicine Practice: Stroke EXTRA! offers a comprehensive, evidence-based review of stroke in young adults, including its distinct etiologies, diagnostic complexities, and tailored management approaches. Select case presentations highlight key considerations in evaluating and managing stroke in young adults, emphasizing the importance of timely recognition, rapid intervention, and long-term management.
A stroke code is called on her arrival to the ED. She was last known to be at her baseline about 5 hours prior to arrival. Her initial blood pressure is 176/94 mm Hg, and her serum glucose level is 102 mg/dL. On examination, she is in distress due to headache; on neurologic examination, she has mild weakness of the left lower face and weakness of the left arm. Her NIHSS score is 2. She has a history of polysubstance use. What are the most appropriate studies needed for this patient? Is she a candidate for any acute stroke intervention?
The patient reports that he awoke in the morning with pain in the left side of his neck and has had a progressive headache throughout the day. He recalls that he was lifting weights the night prior and had some mild left-sided neck pain during his workout, but it had resolved. He has no past medical history. On arrival to the ED, his blood pressure is 136/82 mm Hg. On neurologic examination, he has reduced sensation and weakness in the right arm and leg, and mild gait unsteadiness. Does this patient need emergent neuroimaging? If so, what studies should be ordered? Is he a candidate for any acute stroke intervention?
He said she was unable to locate the telephone, which was sitting on the table next to her, and when he noticed a left facial droop, he called 911. He reports that she seemed fine about 5 hours earlier. On arrival to the ED her blood pressure is 186/102 mm Hg. Her serum glucose level is 205 mg/dL. She has a history of hypertension, diabetes, and active smoking. On examination, she denies any deficits but is looking toward her right side and will not look to her left. She has a left-sided visual field deficit, lower facial droop, and is not moving her left arm. Her NIHSS score is 13. What imaging studies are needed emergently? Is this patient a candidate for any acute stroke intervention?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
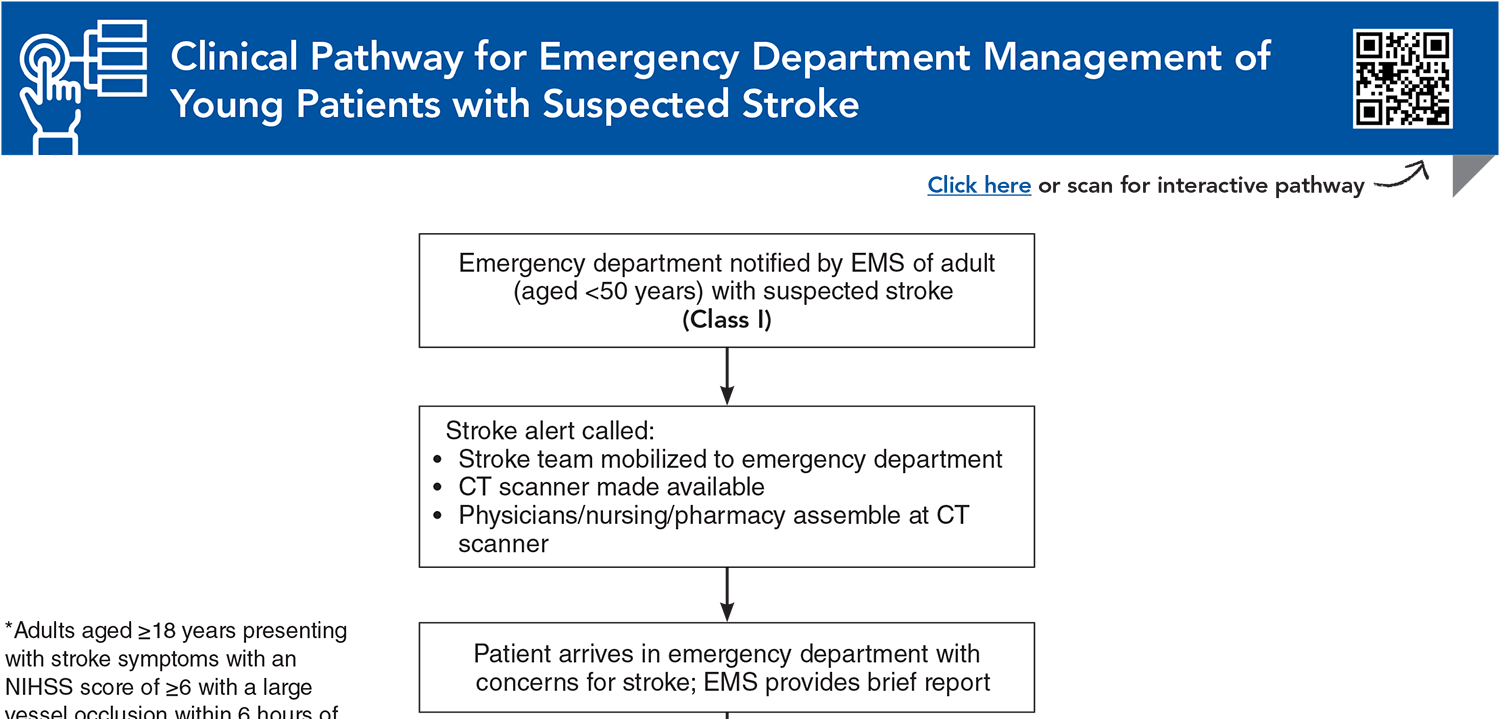
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
5. * Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic troke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. (Guidelines) DOI: 10.1161/STR.0000000000000211
6. * Putaala J. Ischemic stroke in young adults. Continuum (Minneap Minn). 2020;26(2):386-414. (Review article) DOI: 10.1212/CON.0000000000000833
7. * Mendelson SJ, Prabhakaran S. Diagnosis and management of transient ischemic attack and acute ischemic stroke: a review. JAMA. 2021;325(11):1088-1098. (Review article) DOI: 10.1001/jama.2020.26867
8. * George MG. Risk factors for ischemic stroke in younger adults: a focused update. Stroke. 2020;51(3):729-735. (Review article) DOI: 10.1161/STROKEAHA.119.024156
9. * Saini V, Guada L, Yavagal DR. Global epidemiology of stroke and access to acute ischemic stroke interventions. Neurology. 2021;97(20 Suppl 2):S6-S16. (Review article) DOI: 10.1212/WNL.0000000000012781
10. * Powers WJ. Acute ischemic stroke. N Engl J Med. 2020;383(3):252-260. (Review article) DOI: 10.1056/NEJMcp1917030
11. * Herpich F, Rincon F. Management of acute ischemic stroke. Crit Care Med. 2020;48(11):1654-1663. (Review article) DOI: 10.1056/NEJMcp1917030
92. * Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731. (Meta-analysis; 5 studies, 1287 patients) DOI: 10.1016/S0140-6736(16)00163-X
107. * CADISS trial investigators, Markus HS, Hayter E, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015;14(4):361-367. (Randomized controlled trial; 250 patients) DOI: 10.1016/S1474-4422(15)70018-9
112. * Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):e282-e361. (Guidelines) DOI: 10.1161/STR.0000000000000407
Subscribe to get the full list of 139 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: stroke, young adults, acute ischemic stroke, hemorrhagic stroke, cervical artery dissection, cardioembolic stroke, patent foramen ovale, hypercoagulable states, cerebral venous sinus thrombosis, stroke mimics, intravenous thrombolysis, mechanical thrombectomy, computed tomography, CT angiography, CT perfusion, magnetic resonance imaging, diffusion-weighted imaging, FLAIR, large vessel occlusion, hypertension, diabetes, dyslipidemia, substance use, migraine, vasculopathies, moyamoya disease, CADASIL, prehospital stroke care, rehabilitation
Karissa C. Arthur, MD; Taylor N. Haight, MD; Rohan Arora, MD, FAHA; Shraddha Mainali, MD
William A. Knight IV, MD, FNCS, FACEP; Camelia Valhuerdi Porto, MD
December 15, 2025
December 20, 2028 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Stroke credits, subject to your state and institutional approval.