

Drugs of addiction have been associated with an increased risk of both hemorrhagic and ischemic stroke. While the mechanisms that increase stroke risk are well recognized for the most commonly used substances, there is limited evidence to guide the management and treatment of stroke in the setting of concurrent substance use disorder. This review presents a comprehensive approach to evaluation and management of stroke in patients with substance use disorders. Identification of concurrent drug intoxication and guidelines for drug screening in stroke patients are discussed, along with standardized treatment strategies to improve care and outcomes in these patients.
The patient is extremely agitated on arrival, requiring multiple officers to restrain him, so he is placed in 4-point restraints. He is sedated for safety and to facilitate clinical evaluation. Once he is calmer, you obtain vital signs and note that he is tachycardic and hypertensive, with a heart rate of 130 beats/min and blood pressure of 230/120 mm Hg. You also note that he does not seem to be moving his left side well and has facial droop. You are concerned for possible stroke. What diagnostic challenges do you anticipate? How may treatment options be limited in this patient?
The patient is anxious and tremulous and informs you she has been incarcerated for 48 hours. Her initial vital signs are significant for heart rate of 120 beats/min and blood pressure of 200/120 mm Hg. Given her restlessness and anxiety, she is unable to provide a reliable history. You note that the patient has equal pupils, left-sided facial droop and left upper-extremity weakness. You order a STAT CT of the head, which shows a right basal ganglia hemorrhage with mild right-to-left shift. How can treatment for hemorrhagic stroke be affected in this patient? What interventions should be considered to improve this patient’s management?
The EMS report states that the patient was last seen well at 11:00 PM when she went to bed after consuming 5 or 6 alcoholic mixed drinks. She was noted by EMS to have mild hypotension, with blood pressure of 89/60 mm Hg. Her point-of-care glucose level was 75 on EMS arrival. She received 1 L of IV saline during transport in addition to IV glucose and thiamine. In the ED, the patient is more responsive and answering simple questions. The initial examination is remarkable for bilateral nystagmus, dysarthria, and mild truncal ataxia. Her vital signs are: temperature, 36.0°C; heart rate 90 beats/min; blood pressure, 100/70 mm Hg; and oxygen saturation, 95%. Her lab test results are remarkable for an ethanol level of 0.205 g/dL. A head CT shows no evidence of obvious ischemic stroke or hemorrhage. Her symptoms are attributed to alcohol intoxication, and she remains in the ED for IV fluids and monitoring. Two hours later, the patient complains of diplopia and dysphagia despite improving alertness. A stroke alert is activated and she undergoes CTA of the head and neck, which shows occlusion of the basilar artery. Does alcohol intoxication affect this patient’s candidacy for mechanical thrombectomy?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
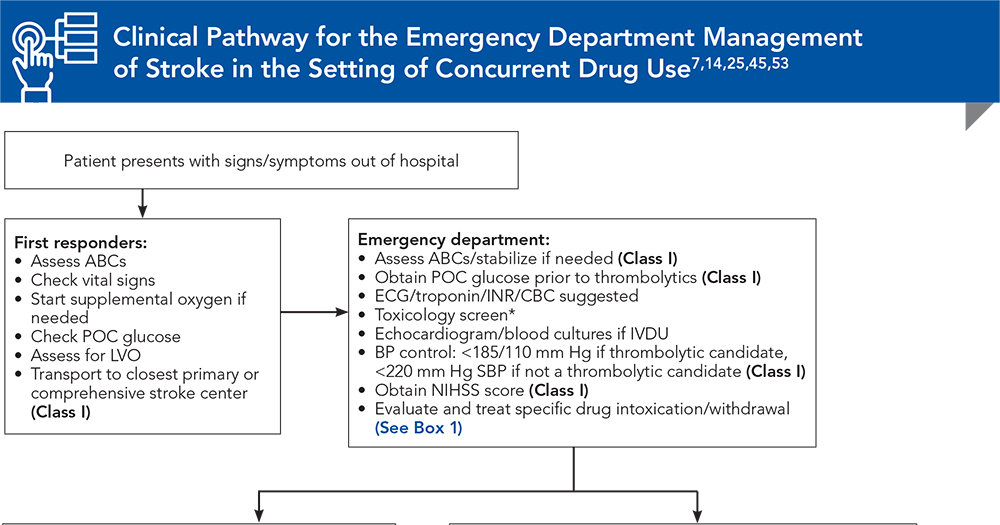
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.

Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
7. * Fonseca AC, Ferro JM. Drug abuse and stroke. Curr Neurol Neurosci Rep. 2013;13(2):325. (Review) DOI: 10.1007/s11910-012-0325-0
14. * Tsatsakis A, Docea AO, Calina D, et al. A mechanistic and pathophysiological approach for stroke associated with drugs of abuse. J Clin Med. 2019;8(9):1295. (Review) DOI: 10.3390/jcm8091295
25. * Middlekauff HR, Cooper ZD, Strauss SB. Drugs of misuse: focus on vascular dysfunction. Can J Cardiol. 2022;38(9):1364-1377. (Review) DOI: 10.1016/j.cjca.2022.04.011
45. * Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):E344-E418. (Clinical guidelines) DOI: 10.1161/STR.0000000000000211
53. * Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):E282-E361. (Clinical guideline) DOI: 10.1161/STR.0000000000000407
Subscribe to get the full list of 72 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: stroke, drugs addicton, substance use, substance use disorder, SUD, drug intoxication, stroke mimics, ischemic stroke, hemorrhagic stroke, cocaine, cannabinoids, amphetamines, MDMA, meth, ecstasy, molly, opioids, cerebral vasculitis, acute severe hypertension, toxicology screening, toxidromes, alcohol use disorder, AUD, alcohol withdrawal, Wernicke syndrome, thiamine deficiency, endocarditis
Abigail La Nou, MD; Smitesh Padte, MBBS; Mustafa Sajjad Cheema, MBBS; Sindhura Tadisetty, MBBS; Rahul Kashyap, MD, MBA
Mandy Hatfield, MD; Fajun Wang, MD
September 15, 2024
September 15, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Stroke credits, 2 Substance Use credits, and 1 Controlled Substances credit, subject to your state and institutional approval.