Table of Contents
About This Issue
Emergency clinicians must have a high index of suspicion for cerebrovascular injury in pregnant and postpartum patients who present with any stroke-like symptoms. While data on managing stroke in this demographic are limited, in general, the ED approach to maternal stroke closely follows established protocols for nonpregnant patients. In this issue, you will learn:
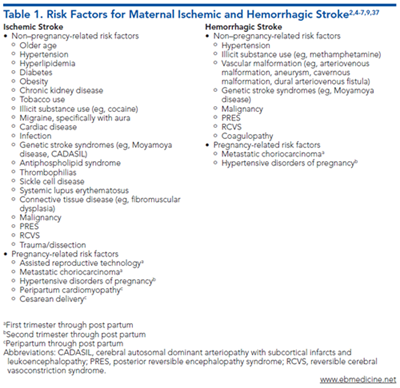
The specific pregnancy- and non-pregnancy-related risk factors for maternal ischemic and hemorrhagic stroke.
Differential diagnoses and mimics of stroke in pregnant and postpartum patients.
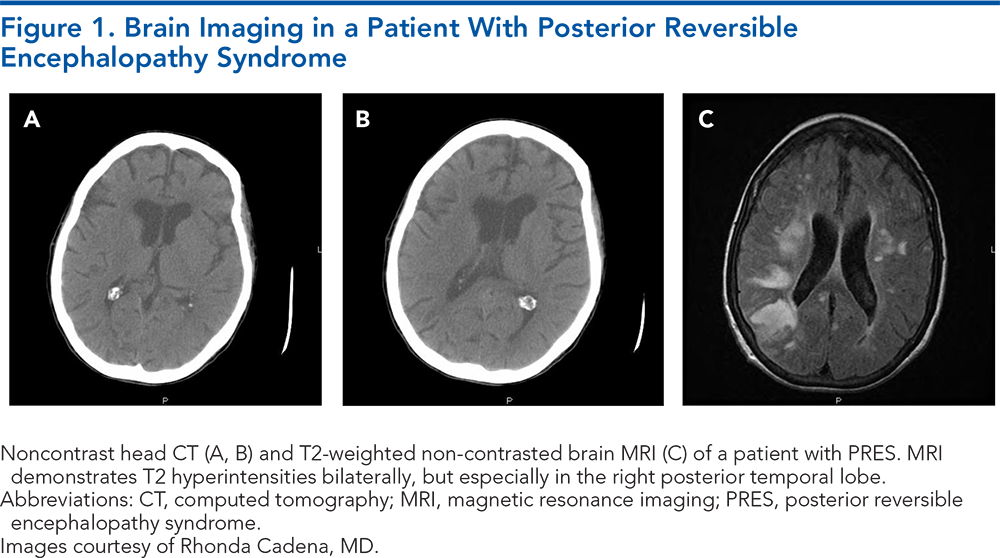
The utility of various imaging modalities in the assessment of maternal stroke, including CT, CTA, CTP, CTV, and MRI.
The latest recommendations for medical management of hypertension in pregnant patients.
ED management recommendations for acute ischemic stroke, large vessel occlusion, cerebral venous sinus thrombosis, intracerebral hemorrhage, arteriovenous malformation, and aneurysm rupture in pregnant and postpartum patients.
The available evidence regarding the use of IV thrombolytics and mechanical thrombectomy in pregnancy.
-
About This Issue
-
Abstract
-
Case Presentations
-
Introduction
-
Critical Appraisal of the Literature
-
Etiology, Pathophysiology, and Risk Factors
-
Etiology
-
Pathophysiology
-
Risk Factors
-
Non–Pregnancy-Related Risk Factors
-
Pregnancy-Related Risk Factors
-
Differential Diagnosis
-
Prehospital Care
-
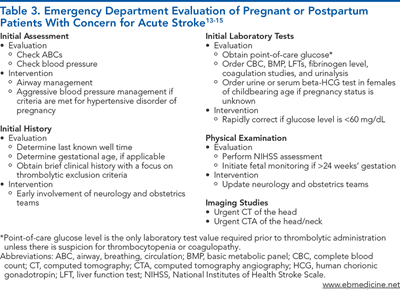
Emergency Department Evaluation
-
Initial Assessment
-
History
-
Physical Examination
-
Diagnostic Studies
-
Laboratory Testing
-
Imaging Studies
-
Emergency Department Management
-
Blood Pressure Management
-
Intravenous Thrombolytics for Acute Ischemic Stroke
-
Mechanical Thrombectomy for Acute Ischemic Stroke With Large Vessel Occlusion
-
Management of Cerebral Venous Sinus Thrombosis
-
Management of Intracerebral Hemorrhage
-
Arteriovenous Malformation and Aneurysm Rupture
-
Disposition
-
Summary
-
Risk Management Pitfalls to Avoid in the Emergency Department Management of Stroke in Pregnant and Postpartum Patients
-
Case Conclusions
-
Clinical Pathway for Stroke Management in Pregnant and Postpartum Patients
-
Tables and Figures
-
References
Abstract
Maternal stroke contributes to a significant burden of disease in the pregnant and postpartum patient populations, with an incidence nearly 3-fold that of comparable nonpregnant cohorts. Emergency clinicians must maintain a high index of suspicion for cerebrovascular injury in these patients, as rapid diagnosis and emergent management can prevent devastating neurological outcomes. Data on management of cerebrovascular injury in pregnant and postpartum patients are limited, but management of maternal stroke in the emergency department aligns closely with protocols established for nonpregnant patients. This issue discusses the risk factors associated with maternal stroke, and reviews the available evidence for emergency department management of maternal stroke, including thrombolytic and interventional therapies.
Case Presentations
-
She is G2P1. She is accompanied by her mother, who reports that 2 hours ago, the patient suddenly became unable to speak in the middle of a conversation. There was also an observed right facial droop and difficulty moving her right arm.
-
The patient's mother says that her daughter is otherwise healthy, does not take any medications, and has had an unremarkable pregnancy thus far.
-
You call a code stroke and immediately check the patient's blood pressure, which is 128/85 mm Hg. On exam, she has notable aphasia, right facial droop, and right arm flaccidity, with a total NIHSS score of 25.
-
What emergent labs should you order for this patient? What imaging is indicated? Is this patient a candidate for any interventions?
-
She is G1P1 and had a healthy pregnancy and delivery.
-
She says she frequently experiences migraines, but this headache “feels different.” In contrast to her typical migraine, this new headache involves the whole head and is worse when she is lying down.
-
What are the “can’t-miss” diagnoses in a postpartum patient who presents to the ED with a new headache? Should this patient undergo any imaging? If so, how urgently?
-
Bystanders at a community picnic say the woman initially appeared well but suddenly complained of a severe headache and fell to the ground. When EMS arrived at the scene, the patient was unresponsive. Her blood pressure was 160/95 mm Hg and GCS score was 8. She was intubated in the field.
-
A code stroke is activated upon her arrival in the ED, where her repeat blood pressure is 155/87 mm Hg. She is on minimal sedation but does not follow commands or meaningfully track.
-
She is G3P2 and has no other past medical history. On exam, both pupils are dilated and sluggishly reactive, and she has no movement in the left arm or left leg, while she withdraws her right upper and lower extremities to noxious stimuli. You estimate her NIHSS score at 24. Her blood glucose level is 110 mg/dL.
-
What is the best approach for the management of this patient’s blood pressure?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
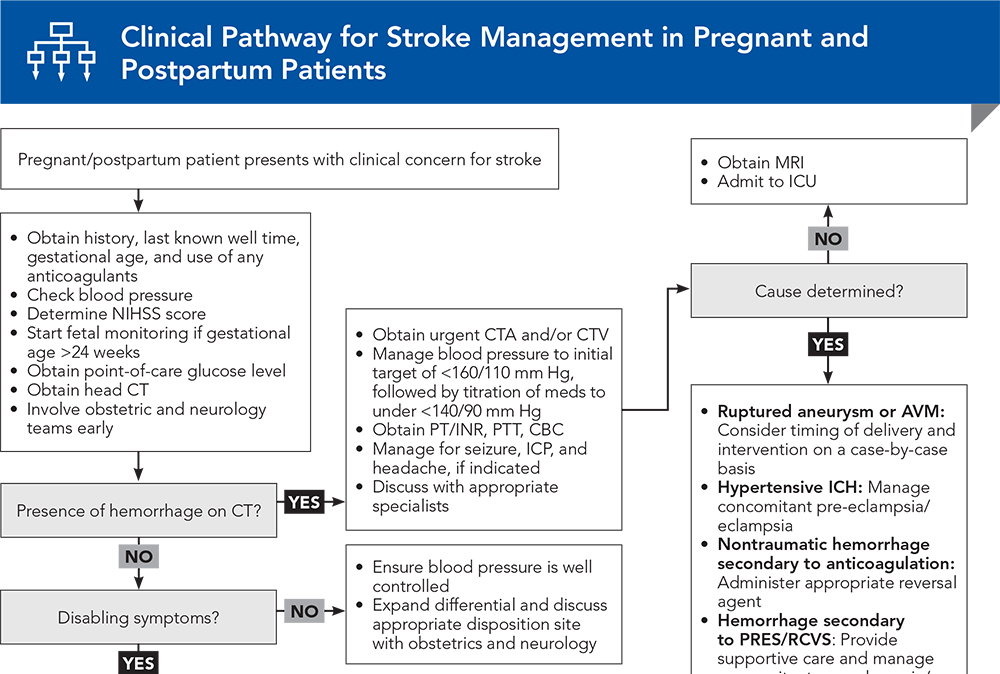
Clinical Pathway for Stroke Management in Pregnant and Postpartum Patients
Subscribe to access the complete flowchart to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
13. * Ladhani NNN, Swartz RH, Foley N, et al. Canadian stroke best practice consensus statement: acute stroke management during pregnancy. Int J Stroke. 2018;13(7):743-758. (Guidelines) DOI: 10.1177/1747493018786617
15. * Kremer C, Gdovinova Z, Bejot Y, et al. European Stroke Organisation guidelines on stroke in women: management of menopause, pregnancy and postpartum. Eur Stroke J. 2022;7(2):I-XIX. (Guidelines) DOI: 10.1177/23969873221078696
16. * Gestational hypertension and preeclampsia: ACOG practice bulletin, number 222. Obstet Gynecol. 2020;135(6):1492-1495. (Guidelines) DOI: 10.1097/AOG.0000000000003892
37. * Miller EC. Maternal stroke associated with pregnancy. Continuum (Minneap Minn). 2022;28(1):93-121. (Review) DOI: 10.1212/CON.0000000000001078
Subscribe to get the full list of 98 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: maternal stroke, stroke in pregnancy, postpartum stroke, HELLP, pre-eclampsia, eclampsia, hypertension, intracerebral hemorrhage, cerebral venous sinus thrombosis, posterior reversible encephalopathy syndrome, reversible cerebral vasoconstrictive syndrome, large vessel occlusion, arteriovenous malformation, aneurysm, antihypertensive, thrombectomy, thrombolysis, AVM, CVST, PRES, RCVS, ICH, SAH, LVO, NIHSS