Table of Contents
About This Issue
Gastrointestinal (GI) bleeding is common in pediatric patients. The main goal in managing pediatric GI bleeding in the emergency department is to identify and treat severe cases or those that may result in significant bleeding and deteriorate rapidly, while avoiding unnecessary workup and hospital admission for patients with minor or self-resolving conditions. This issue provides a comprehensive review of the causes of GI bleeding in children and offers management strategies for upper and lower GI bleeding. In this issue, you will learn:
Definitions associated with GI bleeding
Mimics of GI bleeding
Causes of upper and lower GI bleeding in pediatric patients
Critical elements of the history and physical examination that can help identify the potential source of bleeding
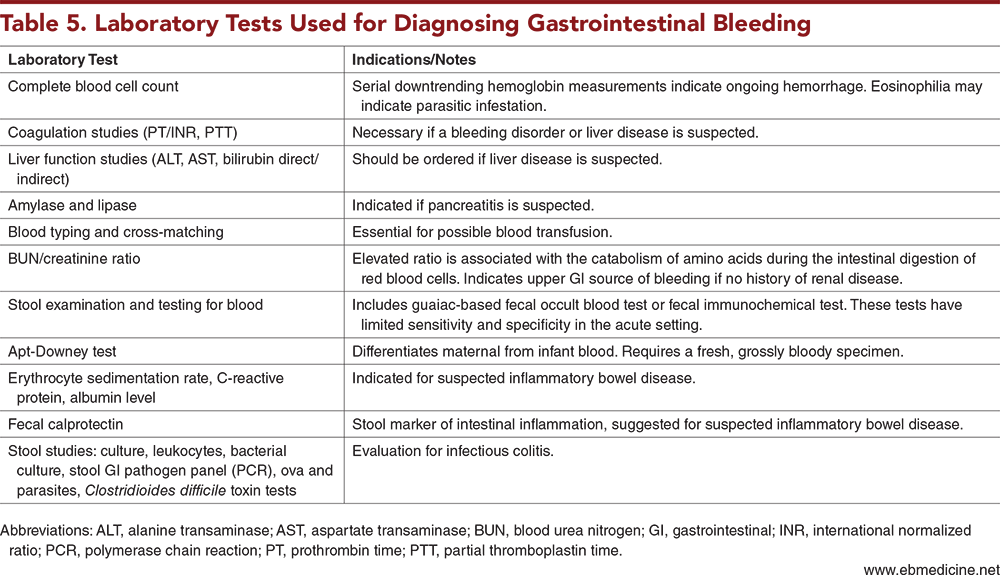
Laboratory tests that can be used for diagnosis of GI bleeding
Imaging studies for GI bleeding that can be useful in determining the etiology of bleeding
How to use the Sheffield scoring system to assess the likelihood of a child needing emergency endoscopy
Recommendations for managing hemodynamically unstable patients with GI bleeding
Options for pharmacologic treatment of upper GI bleeding
Detailed strategies for managing patients with esophageal varices, gastritis, peptic ulcer disease, necrotizing enterocolitis, food protein-induced allergic proctocolitis, intussusception, inflammatory bowel disease, and toxic megacolon
Recommendations for disposition of children with GI bleeding
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Upper Gastrointestinal Bleeding
- Lower Gastrointestinal Bleeding
- Specific Conditions in the Differential Diagnosis of Gastrointestinal Bleeding
- Esophageal Varices
- Peptic Ulcers
- Mallory-Weiss and Prolapse Gastropathy Syndrome
- Necrotizing Enterocolitis
- Malrotation With Midgut Volvulus
- Anal Fissures
- Food Protein-Induced Allergic Proctocolitis
- Intussusception
- Meckel Diverticulum
- Infectious Colitis
- Inflammatory Bowel Disease
- Toxic Megacolon
- Juvenile Polyps
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Laboratory Testing
- Imaging Studies
- Ultrasound
- Upper Gastrointestinal Series
- Meckel Scan
- Colonoscopy
- Endoscopy
- Timing of Endoscopy
- Computed Tomography Angiography
- Radionuclide Imaging
- Treatment
- Management of Hemodynamically Unstable Patients
- Pharmacologic Options
- Acid Suppression
- Anticoagulation Reversal
- Management of Gastrointestinal Bleeding, Based on Underlying Cause
- Esophageal Varices
- Gastritis and Peptic Ulcer Disease
- Necrotizing Enterocolitis
- Food Protein-Induced Allergic Proctocolitis
- Intussusception
- Inflammatory Bowel Disease
- Toxic Megacolon
- Special Populations
- Children Receiving Chemotherapy
- Patients With Hirschsprung Disease
- Controversies and Cutting Edge
- Defining Severe Gastrointestinal Bleeding
- Nasogastric Tube Placement and Lavage
- Early Discharge Following Intussusception Reduction
- Fecal Occult Blood Testing
- Disposition
- Summary
- Time- and Cost-Effective Strategies
- Risk Management Pitfalls in Managing Pediatric Patients With Gastrointestinal Bleeding
- 5 Things That Will Change Your Practice
- Case Conclusions
- Clinical Pathways
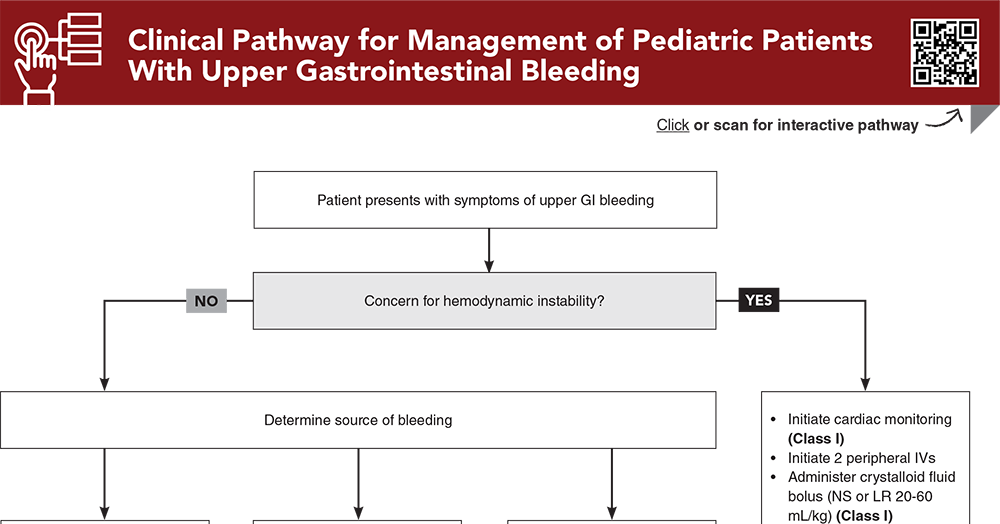
- Clinical Pathway for Management of Pediatric Patients With Upper Gastrointestinal Bleeding
- Clinical Pathway for Management of Pediatric Patients With Lower Gastrointestinal Bleeding
- Tables and Figures
- References
Abstract
Pediatric gastrointestinal (GI) bleeding ranges from mild and self-limited cases to severe episodes of hemorrhagic shock. A structured, age-specific approach is essential for the correct diagnostic workup and effective management. Collaboration with a multidisciplinary team, including pediatric surgery and gastroenterology specialists, may be necessary. The goal of managing pediatric patients with GI bleeding in the emergency department is to identify and treat severe cases, while avoiding unnecessary workup and admission for patients with mild or self-resolving cases. This issue provides a comprehensive review of the definitions, causes, and management strategies for upper and lower GI bleeding in children. It also highlights existing knowledge gaps and future research directions.
Case Presentations
- The boy’s parents report no vomiting or signs of pain. They brought a diaper with a large amount of bloody stool in it. They say the boy continues to tolerate his diet well.
- On examination, the boy has no fever, his heart rate is 130 beats/min, and his blood pressure is 95/50 mm Hg. His abdomen is soft and nontender, with no palpable masses, and his external perianal examination is normal.
- Considering the patient’s clinical presentation, which diagnostic and management steps would be most appropriate to prioritize?
- The parents report that the infant is exclusively breastfed. She had 3 to 4 episodes of red blood-tinged stool, with no changes in consistency. There is no evidence of vomiting or pain.
- Upon arrival at the ED, the infant appears well and is not in distress. She has a normal physical examination and vital signs, including a heart rate of 120 beats/min.
- Despite the infant’s reassuring appearance, you are considering whether to initiate further evaluation. What tests should you order? What is your differential diagnosis?
- The boy’s mother urgently brought him to the ED. He has no fever or diarrhea but has had a poor appetite for the last 2 days and has recently appeared more pale. She reports no similar episodes in the past.
- Upon arrival, the patient appears tired, is tachycardic with a heart rate in the 160s, has weak peripheral pulses, and a blood pressure of 70/35 mm Hg. His examination is notable for pallor, scleral icterus, and a palpable spleen below the costal margin. His abdomen is soft and nontender.
- Given the history of the Kasai procedure, how does this influence your initial differential diagnosis? What are the most critical steps in the workup and resuscitation of this patient?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Pediatric Patients With Upper Gastrointestinal Bleeding
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
5. * Baker RD, Baker SS. Gastrointestinal bleeds. Pediatr Rev. 2021;42(10):546-557. (Review) DOI: 10.1542/pir.2020-000554
8. * Romano C, Oliva S, Martellossi S, et al. Pediatric gastrointestinal bleeding: perspectives from the Italian Society of Pediatric Gastroenterology. World J Gastroenterol. 2017;23(8):1328-1337. (Review) DOI: 10.3748/wjg.v23.i8.1328
16. * Thomson MA, Leton N, Belsha D. Acute upper gastrointestinal bleeding in childhood: development of the Sheffield scoring system to predict need for endoscopic therapy. J Pediatr Gastroenterol Nutr. 2015;60(5):632-636. (Retrospective study; 69 patients) DOI: 10.1097/mpg.0000000000000680
19. * Novak I, Bass LM. Gastrointestinal bleeding in children: current management, controversies, and advances. Gastrointest Endosc Clin N Am. 2023;33(2):401-421. (Review) DOI: 10.1016/j.giec.2022.11.003
86. * Colle I, Wilmer A, Le Moine O, et al. Upper gastrointestinal tract bleeding management: Belgian guidelines for adults and children. Acta Gastroenterol Belg. 2011;74(1):45-66. (Guideline)
119. *Freedman SB, Stewart C, Rumantir M, et al. Predictors of clinically significant upper gastrointestinal hemorrhage among children with hematemesis. J Pediatr Gastroenterol Nutr. 2012;54(6):737-743. (Retrospective cohort study; 613 patients) DOI: 10.1097/MPG.0b013e3182417a47
Subscribe to get the full list of 123 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: gastrointestinal bleeding, GI bleeding, pediatric gastrointestinal disorders, acute gastrointestinal bleeding, emergency management of gastrointestinal bleeding, gastrointestinal bleeding diagnostics, gastrointestinal bleeding mimics, upper gastrointestinal bleeding, lower gastrointestinal bleeding, hematemesis, melena, hematochezia, peptic ulcers, gastritis, esophageal varices, variceal bleeding, Meckel diverticulum, intussusception, peptic ulcer disease, inflammatory bowel disease, allergic proctocolitis, therapeutic endoscopy, fictitious bleeding, Mallory-Weiss tear, enterocolitis, angiodysplasia, hemolytic uremic syndrome, necrotizing enterocolitis, malrotation with midgut volvus, anal fissures, prolapse gastropathy, infectious colitis, toxic megacolon, juvenile polyps, Sheffield scoring system, transjugular intrahepatic portosystemic shunt, Sengstaken-Blakemore tube, Hirschsprung disease, fecal occult blood testing