Table of Contents
About This Issue
Although infectious colitis in an immunocompetent child is often self-limited, complications of colitis can be serious, and early recognition can expedite critical medical interventions and surgical consultation. This issue provides a practical approach to the evaluation and management of adolescent colitis and associated acute complications in the emergency department. In this issue, you will learn:
Common causes of colitis in adolescents, including infectious colitis, inflammatory bowel disease, Clostridioides difficile infection, and sexually transmitted infectious proctitis
Etiologies of lower gastrointestinal bleeding in well-appearing and ill-appearing children
Key aspects of the history that must be obtained, including details regarding the onset and duration of symptoms, stool quality and quantity, the presence of extraintestinal symptoms, and a detailed sexual history
Recommendations for the physical examination including attention to vital signs, assessing for dehydration, abdominal examination, perianal examination, digital rectal examination, and evaluation for extraintestinal manifestations
Validated tools that can be helpful in determining the severity of acute exacerbations
Guidance for when diagnostic studies are indicated and which are recommended
Recommendations for treatment of infectious colitis, acute severe colitis, toxic megacolon, acute flares of inflammatory bowel disease, C difficile pseudomembranous colitis, and sexually transmitted infectious proctitis
Special considerations for patients with stercoral colitis and those with neutropenic enterocolitis
Guidance for disposition of patients with inflammatory bowel disease and those with undifferentiated colitis
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Infectious Colitis
- Inflammatory Bowel Disease
- Clostridioides difficile Infection
- Sexually Transmitted Infectious Proctitis
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Timing
- Stool Quality and Quantity
- Extraintestinal Symptoms
- Sexual History
- Additional Considerations
- Patients With Known Inflammatory Bowel Disease
- Physical Examination
- Diagnostic Studies
- Stool Studies
- Blood Work
- Sexually Transmitted Infection Studies
- Imaging Studies
- X-Ray
- Ultrasound
- Computed Tomography
- Treatment
- Infectious Colitis
- Acute Severe Colitis
- Toxic Megacolon
- Acute Flare of Inflammatory Bowel Disease
- Clostridioides difficile Pseudomembranous Colitis
- Sexually Transmitted Infectious Proctitis
- Special Populations
- Patients With Stercoral Colitis
- Patients With Neutropenic Enterocolitis
- Controversies and Cutting Edge
- Disposition
- Inflammatory Bowel Disease
- Mild to Moderate Flare
- Moderate to Severe Flare
- Undifferentiated Colitis
- Summary
- Risk Management Pitfalls in Emergency Department Management of Adolescent Patients with Colitis
- 5 Things That Will Change Your Practice
- Time- and Cost-Effective Strategies
- Case Conclusions
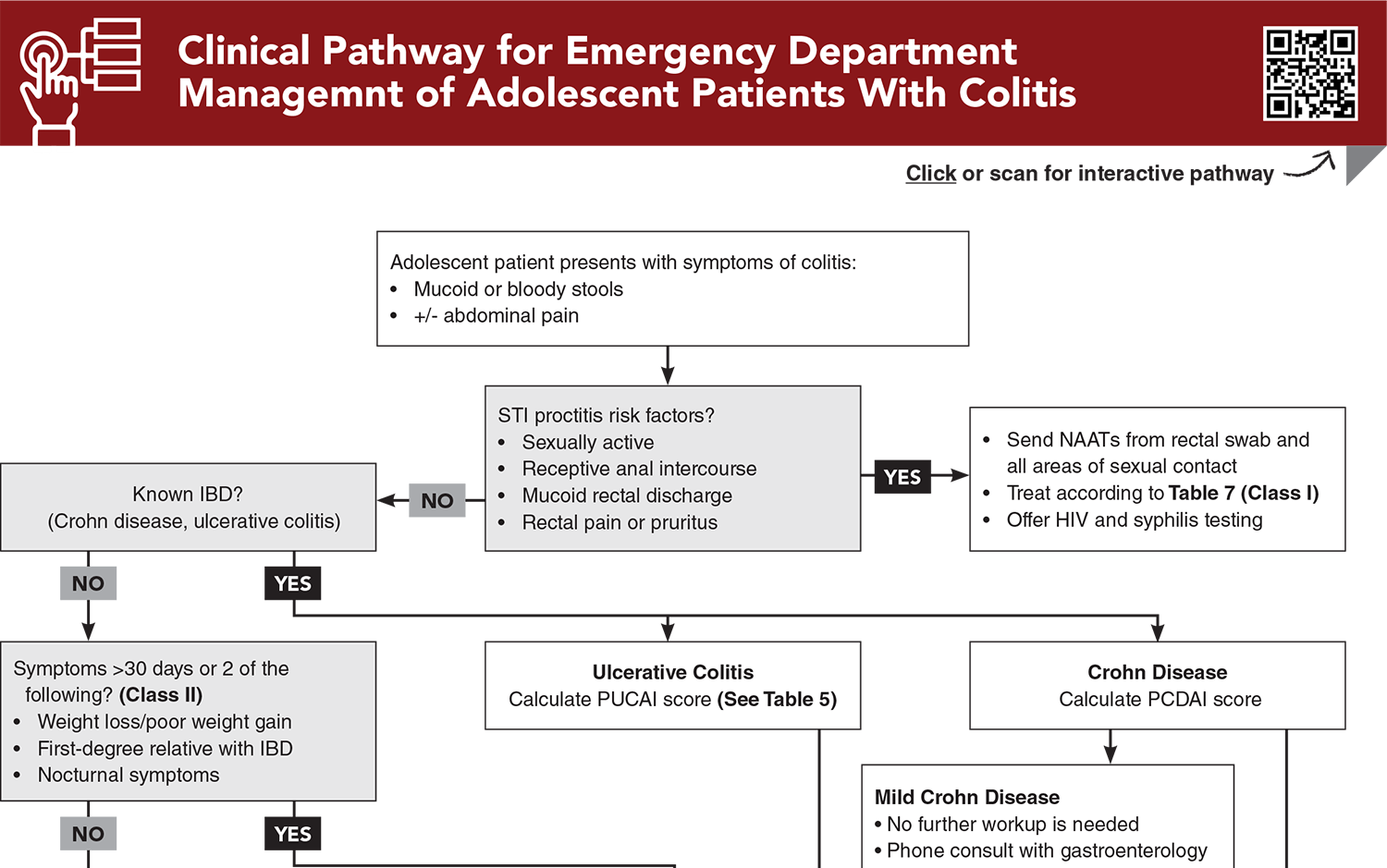
- Clinical Pathway for Emergency Department Management of Adolescent Patients With Colitis
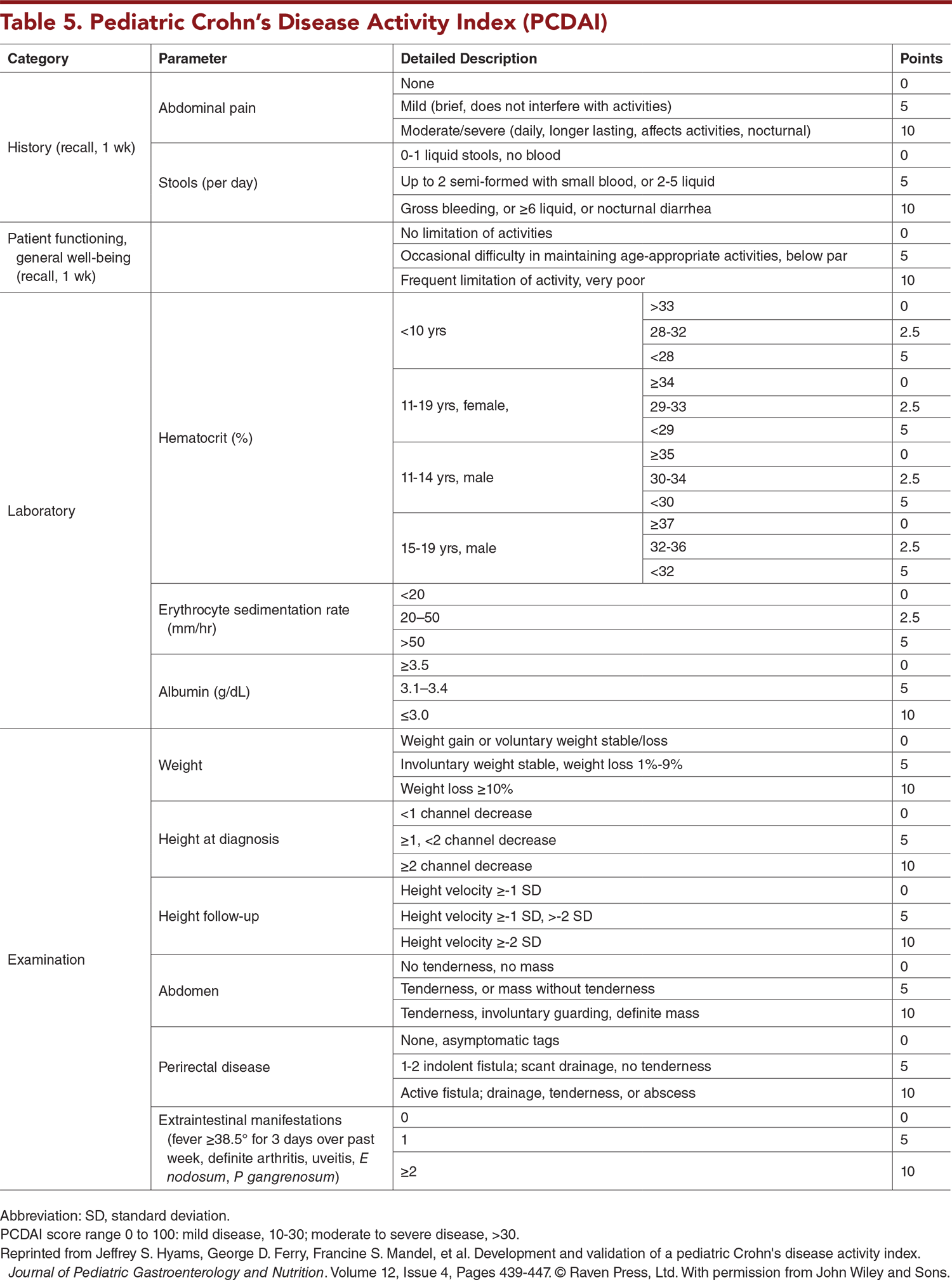
- Tables
- References
Abstract
Colitis presents as an inflammatory diarrhea that is often accompanied by abdominal pain. The differential diagnosis of colitis is broad and depends on the presenting symptoms and age of the patient. Although infectious colitis in an immunocompetent child is often self-limited, complications of colitis can be serious, and early recognition can expedite critical medical interventions and surgical consultation. This issue provides an evidence-based approach to the evaluation and management of colitis and associated acute complications in adolescent patients in the emergency department.
Case Presentations
- The boy says his symptoms began approximately 2 weeks prior to presentation and have worsened over the past 2 to 3 days. He states that he is passing several loose, bloody stools per day and that bowel movements are very painful. Over the past 24 hours he has developed tactile fever and chills. He denies vomiting. He reports that he has had a loss of appetite and an unintentional 10-pound weight loss over the past “couple of months.”
- On examination, he is febrile, mildly tachycardic, and appears ill. His vital signs are: temperature, 38.3°C; heart rate, 118 beats/min; blood pressure, 125/70 mm Hg; respiratory rate, 16 breaths/min; and oxygen saturation, 98% on room air. He is diffusely tender to palpation, especially in the left lower quadrant; he guards his abdomen.
- What additional history can help in determining the cause of this patient’s symptoms?
- The boy’s mother states that it is not unusual for her son to complain of abdominal pain, but that it appears that the pain has been more severe over the past 2 days, and he has been unable to attend school. She reports that he normally has hard and infrequent stools, but that for the past week, he has been having loose and watery stools with occasional soiling of his underwear. She denies recent fever or vomiting. She has noted decreased appetite. There are no known sick contacts.
- On examination, the child is afebrile and nontoxic but appears uncomfortable. His vital signs are: temperature, 36.7°C; heart rate, 95 beats/min; blood pressure, 130/75 mm Hg; respiratory rate, 22 breaths/min; and oxygen saturation, 99% on room air. His abdomen is somewhat firm, mildly distended, and diffusely tender to touch.
- What conditions are on your differential for this patient?
- The patient has a history of a cholecystectomy 4 months prior to presentation but has no other significant past medical history. The teenager reports that she has had almost daily lower abdominal pain for the past 4 weeks. She also reports up to 10 loose stools per day that contain bright red blood.
- On examination, she is somewhat ill but nontoxic-appearing. She is afebrile and has normal vital signs. Her abdomen is soft and nondistended, tender to bilateral lower quadrants, with positive bowel sounds and no rebound or guarding.
- What workup is warranted for this patient?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Adolescent Patients With Colitis
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
4. * Turner D, Ruemmele FM, Orlanski-Meyer E, et al. Management of paediatric ulcerative colitis, part 2: acute severe colitis-an evidence-based consensus guideline from the European Crohn’s and Colitis Organization and the European Society of Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2018;67(2):292-310. (Guidelines) DOI: 10.1097/MPG.0000000000002036
6. * Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017;65(12):1963-1973. (Guidelines) DOI: 10.1093/cid/cix959
21. * Strobel TM, Desai NA, Arrington-Sanders R. Acute infectious proctitis in adolescents. Pediatr Rev. 2023;44(9):491-497. (Review) DOI: 10.1542/pir.2022-005862
36. * Picoraro JA, Moore H, LeLeiko NS. Inflammatory bowel disease: an update. Pediatr Rev. 2023;44(3):139-152. (Review) DOI: 10.1542/pir.2022-005750
47. * Holtman GA, Lisman-van Leeuwen Y, Day AS, et al. Use of laboratory markers in addition to symptoms for diagnosis of inflammatory bowel disease in children: a meta-analysis of individual patient data. JAMA Pediatr. 2017;171(10):984-991. (Meta-analysis; 8 studies, 1120 patients) DOI: 10.1001/jamapediatrics.2017.1736
62. * Peuchant O, Lhomme E, Martinet P, et al. Doxycycline versus azithromycin for the treatment of anorectal Chlamydia trachomatis infection in women concurrent with vaginal infection (CHLAZIDOXY study): a multicentre, open-label, randomised, controlled, superiority trial. Lancet Infect Dis. 2022;22(8):1221-1230. (Randomized controlled trial; 460 patients) DOI: 10.1016/S1473-3099(22)00148-7
63. * Dombrowski JC, Wierzbicki MR, Newman LM, et al. Doxycycline versus azithromycin for the treatment of rectal chlamydia in men who have sex with men: a randomized controlled trial. Clin Infect Dis. 2021;73(5):824-831. (Randomized controlled trial; 133 patients) DOI: 10.1093/cid/ciab153
Subscribe to get the full list of 70 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: adolescent, colitis, infectious colitis, ulcerative colitis, acute severe colitis, toxic megacolon, inflammation of the colon, inflammatory bowel disease, IBD, Crohn disease, pseudomembranous colitis, Clostridioides difficile, C difficile, enterocolitis, proctocolitis, proctitis, sexually transmitted infection, STI, sexually transmitted infectious proctitis, inflammatory diarrhea, bloody diarrhea, bloody stool, hematochezia, mucoid stools, abdominal pain, dehydration, extraintestinal symptoms, Pediatric Ulcerative Colitis Activity Index, PUCAI, Pediatric Crohn’s Disease Activity Index, PCDAI, stool studies, calprotectin, stercoral colitis, neutropenic enterocolitis