Table of Contents
About This Issue
Understanding the anatomy of the wrist and the mechanisms of injury and determining whether imaging is needed are crucial elements in providing optimal patient care. If a thorough history complemented by physical examination cannot rule out fracture or dislocation, appropriate imaging studies may offer valuable insights into accurate diagnosis and treatment planning. Meticulous clinical evaluation and a restrained approach to referral will ensure comprehensive management. In this issue, you will learn:
The anatomy of the wrist, mechanisms of injury, and common injuries;
Traumatic and nontraumatic causes of wrist pain and various types of fractures;
Historical questions to ask, physical examination techniques, and when to assess acute wrist injuries with diagnostic imaging; and
The disposition for wrist sprains and fractures, including those that require outpatient and emergent referral for further evaluation and treatment.
CODING & CHARTING: Determine what level of complication your patient’s wrist injury is to support proper coding and documentation, patient care, and reimbursement.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Anatomy
- Differential Diagnosis
- Urgent Care Evaluation
- History
- Physical Examination
- Inspection
- Palpation
- Range of Motion Testing
- Strength Testing
- Nerve Testing
- Ulnar Nerve
- Median Nerve
- Radial Nerve
- Suspected Carpal Tunnel Syndrome
- Diagnostic Studies
- Plain Radiographs
- Other Diagnostic Testing
- Diagnosis and Management of Common Wrist Injuries
- Fractures and Dislocations
- Sprains
- Overuse Injuries
- Carpal Tunnel Syndrome
- Arthritis
- Ganglion Cysts
- Treatment
- Reducing Inflammation
- Immobilization
- Wrist Braces
- Fiberglass Splinting
- Pain Management
- Special Treatment Considerations
- Carpal Tunnel Syndrome
- Distal Radius Fractures
- Special Populations
- Older Patients
- Medication Considerations in Older Adults
- Nonsteroidal Anti-inflammatory Drugs
- Opioids
- Athletes
- Controversies and Cutting Edge
- Four-dimensional Computed Tomography
- Increased Utilization of Magnetic Resonance Imaging Scans
- Telehealth Rehabilitation
- Disposition
- Summary
- Critical Appraisal of the Literature
- Case Conclusions
- Risk Management Pitfalls in the Evaluation and Management of Wrist Injuries in Urgent Care
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- KidBits: Urgent Care Management of Wrist Injuries in Pediatric Patients
- Etiology and Pathophysiology
- Evaluation and Treatment
- Disposition
- Nonaccidental Trauma
- References
- Coding & Charting: What You Need to Know
- Determining the Level of Service
- Problems Addressed
- Complexity of Data
- Risk of Patient Management
- Documentation Tips
- Coding Challenge: Managing Wrist Injuries in Urgent Care
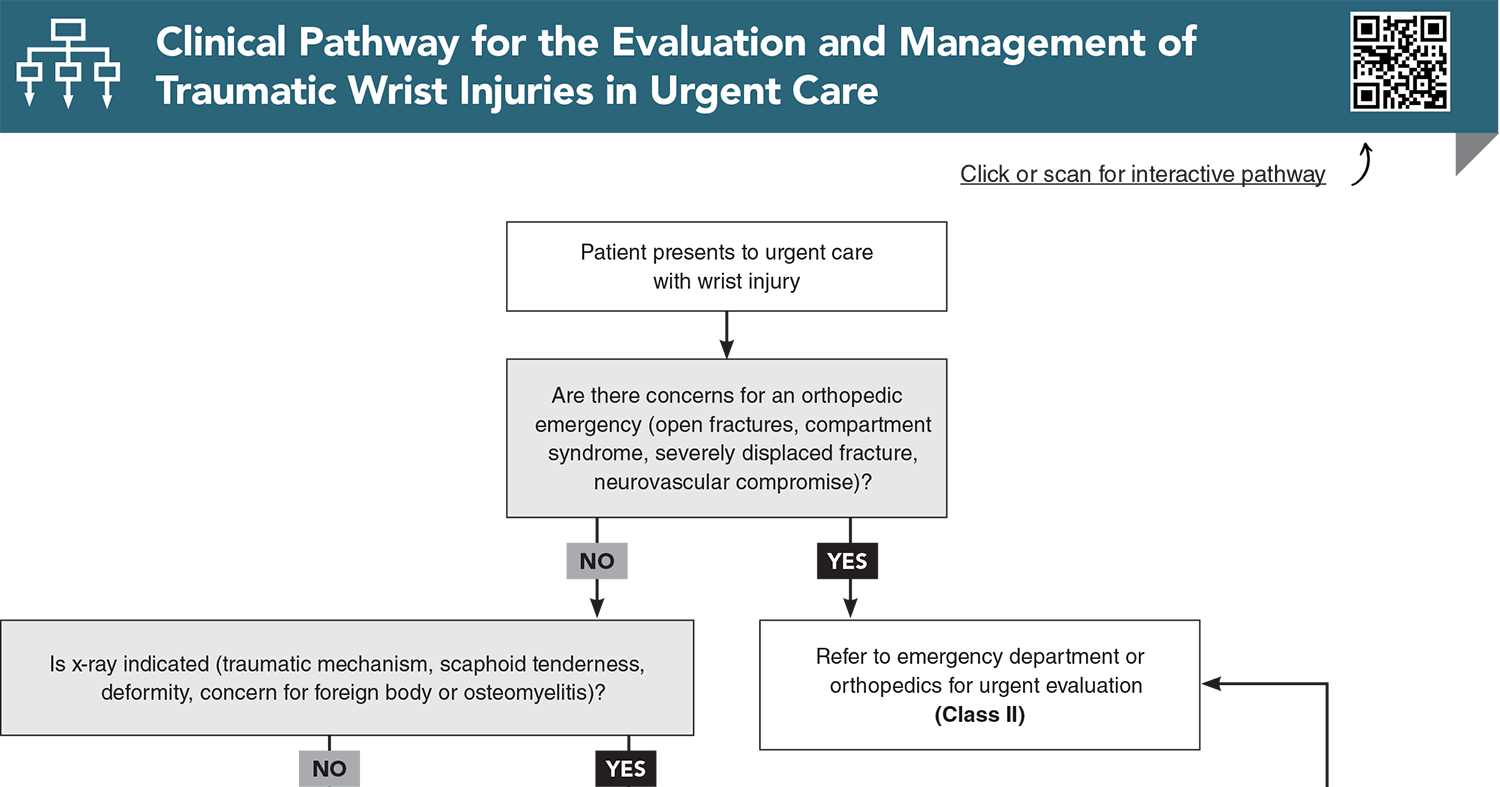
- Clinical Pathway for the Evaluation and Management of Traumatic Wrist Injuries in Urgent Care
- References
Abstract
Wrist injuries are commonly seen in urgent care and acute care settings. Failure to properly evaluate and manage wrist injuries can lead to missed diagnosis, delayed healing, and poorer patient outcomes. This review presents an overview of current best practices for the evaluation and management of wrist injuries in the urgent care setting. Commonly encountered wrist injuries are addressed and frequent diagnostic and management pitfalls are highlighted. Additionally, emerging technologies and imaging modalities that may influence and enhance future clinical practice are discussed.
Case Presentations
- She states that she tripped over the sidewalk and landed on her hand. She did not sustain any other injuries.
- She reports no numbness or tingling in the hand, fingers, or wrist.
- She has applied ice to the injury. She is right-handed and denies any previous wrist injuries or surgeries.
- The patient expresses concern that the wrist is broken...
- He states the injury happened 3 hours ago. He was batting and got struck in the back of the hand by a baseball.
- The patient is right-handed.
- He denies any numbness or tingling in the hand or fingers.
- He is hoping to play in the college state championship next week and asks you if that will be possible...
- She injured it yesterday but was able to finish the competition. Today the pain is more constant.
- She is right-handed.
- She reports no previous injuries or surgery to the area, and she has no numbness or tingling in her hands or fingers.
- Today she is wearing a brace to help with the pain.
- She wonders when her wrist will get better and how she can accelerate the healing process...
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for the Evaluation and Management of Traumatic Wrist Injuries in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908. (Retrospective study; 1,465,874 cases) DOI: 10.1053/jhsu.2001.26322
4. * Simpson AM, Donato DP, Veith J, et al. Hand and wrist injuries among collegiate athletes: the role of sex and competition on injury rates and severity. Orthop J Sports Med. 2020;8(12):2325967120964622. (Descriptive epidemiology study) DOI: 10.1177/2325967120964622
6. * May Jr DD, Varacallo MA. Wrist sprain. StatPearls. Treasure Island (FL); 2024. (Review)
11. * Duckworth AD, Jenkins PJ, Aitken SA, et al. Scaphoid fracture epidemiology. J Trauma Acute Care Surg. 2012;72(2):E41-E45. (Epidemiological study; 151 fractures) DOI: 10.1097/ta.0b013e31822458e8
18. * Gallant GG, Tulipan JE, Rivlin M, et al. Baseball injuries of the hand and wrist. J Am Acad Orthop Surg. 2021;29(15):648-658. (Review) DOI: 10.5435/JAAOS-D-20-00101
19. * Pena J. Lunate dislocation. JETem. 2017;2(1). Accessed May 21, 2025. (Research notes)
27. * Howell DM, Bechmann S, Underwood PJ. Wrist splint. StatPearls. Treasure Island (FL); 2024. (Review)
Subscribe to get the full list of 43 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: distal ulna, radius, metacarpal bones, scaphoid, wrist fracture, anatomical snuffbox, trapezium, FOOSH, Froment Sign, ulnar nerve, Egawa test, Tinel sign, Phalen sign, x-rays, wrist dislocation, wrist sprain, overuse injury, contusion, compartment syndrome, arthritis, distal radius fracture, lunate dislocation, spilled teacup sign, scaphoid-lunate dissociation, Terry Thomas sign, scaphoid bone fracture, splint, brace, sugar tong splint, thumb spica splint, volar wrist splint, hamate bone, carpal bone, lunate bone, carpal tunnel syndrome, ganglion cyst, OLDCARTS, RICE, nonsteroidal anti-inflammatory drugs, Beers Criteria, Amsterdam wrist imaging rules, nonaccidental trauma