Table of Contents
About This Issue
Understanding the anatomy of the elbow and the mechanisms of injury are crucial elements in providing optimal patient care. A thorough physical examination in combination with appropriate imaging studies can help the urgent care clinician distinguish between benign and limb-threatening etiologies. Appropriate management of elbow and forearm pain can help prevent future functional limitations. In this issue, you will learn:
The anatomy of the elbow, mechanisms of injury, and common presentations;
Traumatic and nontraumatic causes of elbow and forearm pain, including various types of overuse and chronic conditions, fractures, dislocation, septic joints, and other serious presentations;
The disposition for chronic causes of pain, dislocation, and fracture, including those that require outpatient referral for further evaluation and treatment.
CODING & CHARTING: Accurate coding and detailed documentation of elbow and forearm pain in the urgent care setting are essential for ensuring quality patient care and proper reimbursement. Learn more in our monthly coding column.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Anatomy
- Differential Diagnosis
- Urgent Care Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Imaging
- Laboratory Studies
- Arthrocentesis of the Radiohumeral Joint
- Treatment
- Osteoarthritis
- Rheumatoid Arthritis
- Lateral Epicondylitis
- Medial Epicondylitis
- Ulnar Neuropathy
- Distal Bicep and Tricep Tendinopathies
- Olecranon Bursitis (Nonseptic)
- Radial Head Fractures
- Proximal Ulnar Fractures
- Distal Humerus Fractures
- Olecranon Fractures
- Coronoid Process Fractures
- Elbow Dislocation
- Septic Bursitis
- Septic Arthritis
- Compartment Syndrome
- Special Populations
- Older Adult Patients
- Controversies and Cutting Edge
- Kinesiology Tape
- Platelet-rich Plasma
- Disposition
- Summary
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls in the Urgent Care Management of Elbow and Forearm Pain
- Time- and Cost-Effective Strategies
- Critical Appraisal of the Literature
- Case Conclusions
- Coding & Charting: What You Need to Know
- Determining the Level of Service
- Problems Addressed
- Complexity of Data
- Risk of Patient Management
- Documentation Tips
- Coding Challenge: Elbow and Forearm Pain in Urgent Care
- Clinical Pathways
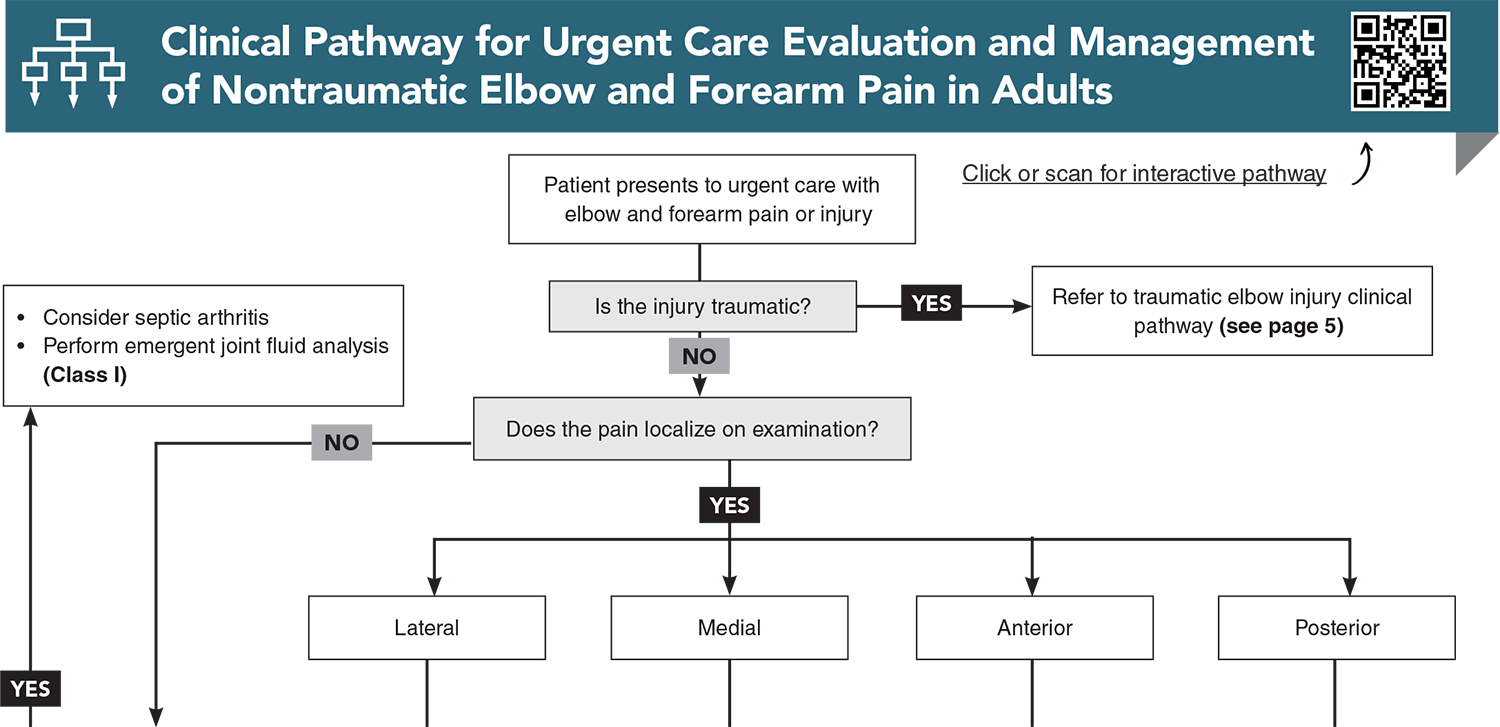
- Clinical Pathway for Urgent Care Evaluation and Management of Nontraumatic Elbow and Forearm Pain in Adults
- Clinical Pathway for the Urgent Care Management of Traumatic Elbow and Forearm Pain in Adults
- References
Abstract
Elbow and forearm pain can be caused by a variety of acute and chronic conditions, which often include a component of trauma or overuse. Key elements of the history and physical examination will guide decision making for a diagnostic workup, especially with consideration of rare but limb-threatening conditions. Many initial treatment plans for common causes of elbow and forearm pain center on conservative therapies, but specialist follow-up or urgent referral may be indicated. This article reviews common and “can’t miss” causes of elbow and forearm pain and their appropriate management and disposition. Evidence-based recommendations are presented, along with cutting edge therapies and considerations for older adults.
Case Presentations
- The pain has been gradually worsening over several days and is worse with movement. There is no history of injury.
- The patient has hypertension, type 2 diabetes mellitus, and a history of kidney stones. His other vital signs are normal.
- On physical examination, there is swelling over the lateral aspect of the elbow. Pain is exacerbated by extension of the forearm. There are no overlying skin changes.
- The patient asks you, “Why is my arm so sore? What can I do for the pain?”
- The patient fell while horseback riding a few hours ago. She is otherwise healthy and is accompanied by her father.
- She reports that she tried to brace herself as she fell but landed on her left side. She says she felt left elbow pain immediately after the fall but denies any other injuries.
- Her vital signs are normal. She is holding the left arm in a flexed position and is guarding against examination.
- The patient’s father asks if her arm is broken.
- The patient reports that she noticed the back of her elbow was swelling over the past day. It is occasionally sore with movement.
- She says she bumped her elbow while exercising a few days ago but did not notice any bruising or swelling at that time. She is otherwise healthy.
- She is afebrile and her vital signs are normal vital.
- On physical examination, there is swelling over the posterior elbow, without erythema or warmth. There is minimal tenderness over the olecranon.
- The patient asks you, “Why is my elbow suddenly swollen?”
- She says she tripped while taking the trash outside. She was able to brace her fall and did not hit her head. She has had right elbow pain since the fall and is reluctant to move her arm.
- Her medical history includes iron deficiency anemia and hypertension. She has normal vital signs.
- On physical examination, there are no overlying skin changes. The inferior aspect of the elbow is tender to palpation.
- There is an audible click as you manipulate the arm from pronated to supinated position.
- The patient asks about the sound when she moves her arm and whether you think something is broken.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Managing Patients Presenting with Acute Diarrhea in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Chin TY, Chou H, Peh WCG. The acutely injured elbow. Radiol Clin North Am. 2019;57(5):911-930. (Review) DOI: 10.1016/j.rcl.2019.03.006
4. * Kheterpal AB, Bredella MA. Overuse injuries of the elbow. Radiol Clin North Am. 2019;57(5):931-942. (Review) DOI: 10.1016/j.rcl.2019.03.005
5. * Hanlon DP, Mavrophilipos V. The emergent evaluation and treatment of elbow and forearm injuries. Emerg Med Clin North Am. 2020;38(1):81-102. (Review) DOI: 10.1016/j.emc.2019.09.005
8. * Kane SF, Lynch JH, Taylor JC. Evaluation of elbow pain in adults. Am Fam Physician. 2014;89(8):649-657. (Review)
20. * Marigi EM, Dancy M, Alexander A, et al. Lateral epicondylitis: critical analysis review of current nonoperative treatments. JBJS Rev. 2023;11(2). (Review) DOI: 10.2106/JBJS.RVW.22.00170
Subscribe to get the full list of 43 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: elbow, humerus, ulna, radius, lateral collateral ligament, ulnar collateral ligament, common extensor tendon, fat pad, overuse injury, bursitis, septic bursitis, septic arthritis, biceps tendinopathy, triceps tendinopathy, radial head fracture, ulnar fracture, coronoid process fracture, olecranon fracture, elbow dislocation, rheumatoid arthritis, osteoarthritis, lateral epicondylitis, medial epicondylitis, ulnar neuropathy, cubital tunnel syndrome, olecranon bursitis, compartment syndrome, arthrocentesis, intra-articular fracture, long arm splint, splinting, inflammation, kinesiology tape, platelet-rich plasma