

Shoulder pain is a frequent complaint in urgent care patients. Complaints may be related acutely (due to injury) or chronically (due to overuse). Correct diagnosis of an acute injury is essential to preventing chronic pain, disability, and life- and limb-threatening complications. This review presents a systematic approach to managing shoulder pain in the urgent care setting by providing a framework for classification using mechanism of action and clinical presentation. Appropriate imaging studies and treatment are discussed, along with the indications for immobilization and outpatient referral, versus emergency department evaluation for more serious injuries that need emergent, definitive care.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
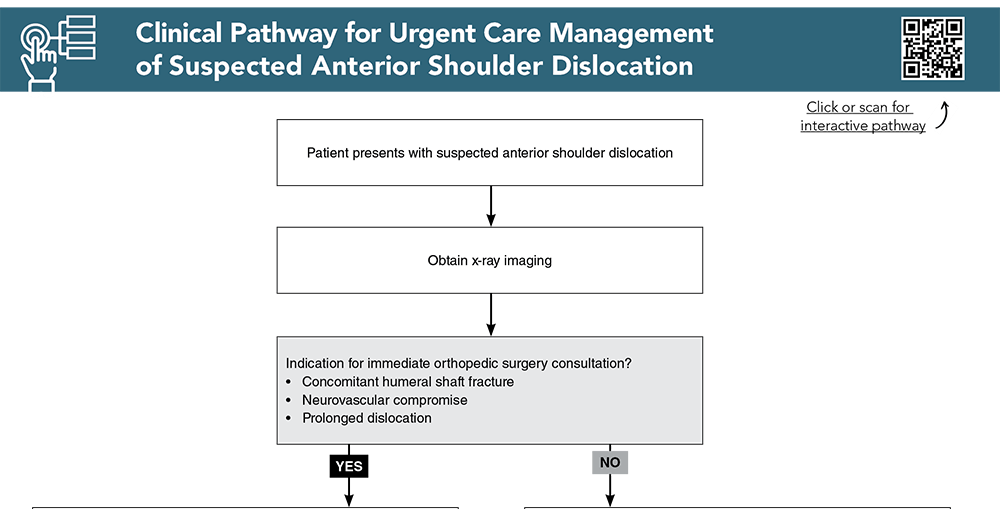
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
5. * Ponce BA, Kundukulam JA, Pflugner R, et al. Sternoclavicular joint surgery: how far does danger lurk below? J Shoulder Elbow Surg. 2013;22(7):993-999. (Prospective cohort; 49 patients) DOI: 10.1016/j.jse.2012.10.037
11. * Slaven EJ, Mathers J. Differential diagnosis of shoulder and cervical pain: a case report. J Man Manip Ther. 2010;18(4):191-196. (Case report) DOI: 10.1179/106698110X12804993426884
23. * Rouleau DM, Hebert-Davies J, Robinson CM. Acute traumatic posterior shoulder dislocation. J Am Acad Orthop Surg. 2014;22(3):145-152. (Review article)
26. * Cadogan A, Mohammed KD. Shoulder pain in primary care: frozen shoulder. J Prim Health Care. 2016;8(1):44. (Observational study; 80 patients)
29. * Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46(14):964-978. (Systematic review; 32 studies, 7693 patients)
Reid D, Chue WL. Endovascular management of an axillary arterial injury post shoulder dislocation. Emerg Med Australas. 2009;21(6):515-517. (Case report)
44. * Stephens NG, Morgan AS, Corvo P, et al. Significance of scapular fracture in the blunt-trauma patient? Ann Emerg Med. 1995;26(4):439-442. (Retrospective review; 173 patients)
45. Neer CS. Displaced proximal humeral fractures: part II. Treatment of three-part and four-part displacement. J Bone Joint Surg. 1970;52(6):1090-1103. (Observational study; 117 patients) PMID: 5455340
53. * Lenza M, Belloti JC, Andriolo RB, et al. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev. 2014(5):CD007121. (Systematic review; 3 trials, 354 patients) DOI: 10.1002/14651858.CD007121.pub3
65. * Deren ME, Behrens SB, Vopat BG, et al. Posterior sternoclavicular dislocations: a brief review and technique for closed management of a rare but serious injury. Orthop Rev (Pavia). 2014;6(1):5245. (Review article)
94. * Ziradkar R, Best TM, Quintero D, et al. Nonsteroidal anti-inflammatory and corticosteroid injections for shoulder impingement syndrome: a systematic review and meta-analysis. Sports Health. 2023;15(4):579-591. (Systematic review and meta-analysis; 10 studies)
Subscribe to get the full list of 110 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: shoulder, injury, fracture, dislocation, overuse syndrome, clavicle, scapula, humerus, joint, glenohumeral, acromioclavicular, sternoclavicular, subacromial bursitis, reduction, rotator cuff, frozen shoulder, adhesive capsulitis, bicep tendonitis, ligament, Neer classification, Rockwood classification, Bankart, Hill-Sachs, luxatio erecta, traction, FARES, Kocher, Davos, intra-articular
Mary Velagapudi, DO; Michelle Wilson, MD; Hope Ring, MD, FACEP
Chrysa Charno, PA-C, MBA, FCUCM; Dina Elnaggar, MD, MS, CAQSM; Michael P. M. Pond, MD
July 1, 2024
July 1, 2027 CME Information
4 AMA PRA Category 1 Credits™. 4 AOA Category 2-B Credits. 4 AAFP Prescribed Credits Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Trauma CME credits.