Table of Contents
About This Issue
ED patients who present with symptoms of alcohol withdrawal – or who develop it during an ED stay – require aggressive treatment and monitoring in order to prevent neuropsychiatric complications that can lead to death. This issue discusses the typical timing of symptoms of alcohol withdrawal syndrome (AWS) and how to begin individualized management, from symptom control to referral resources for alcohol use disorder. In this issue, you will learn:
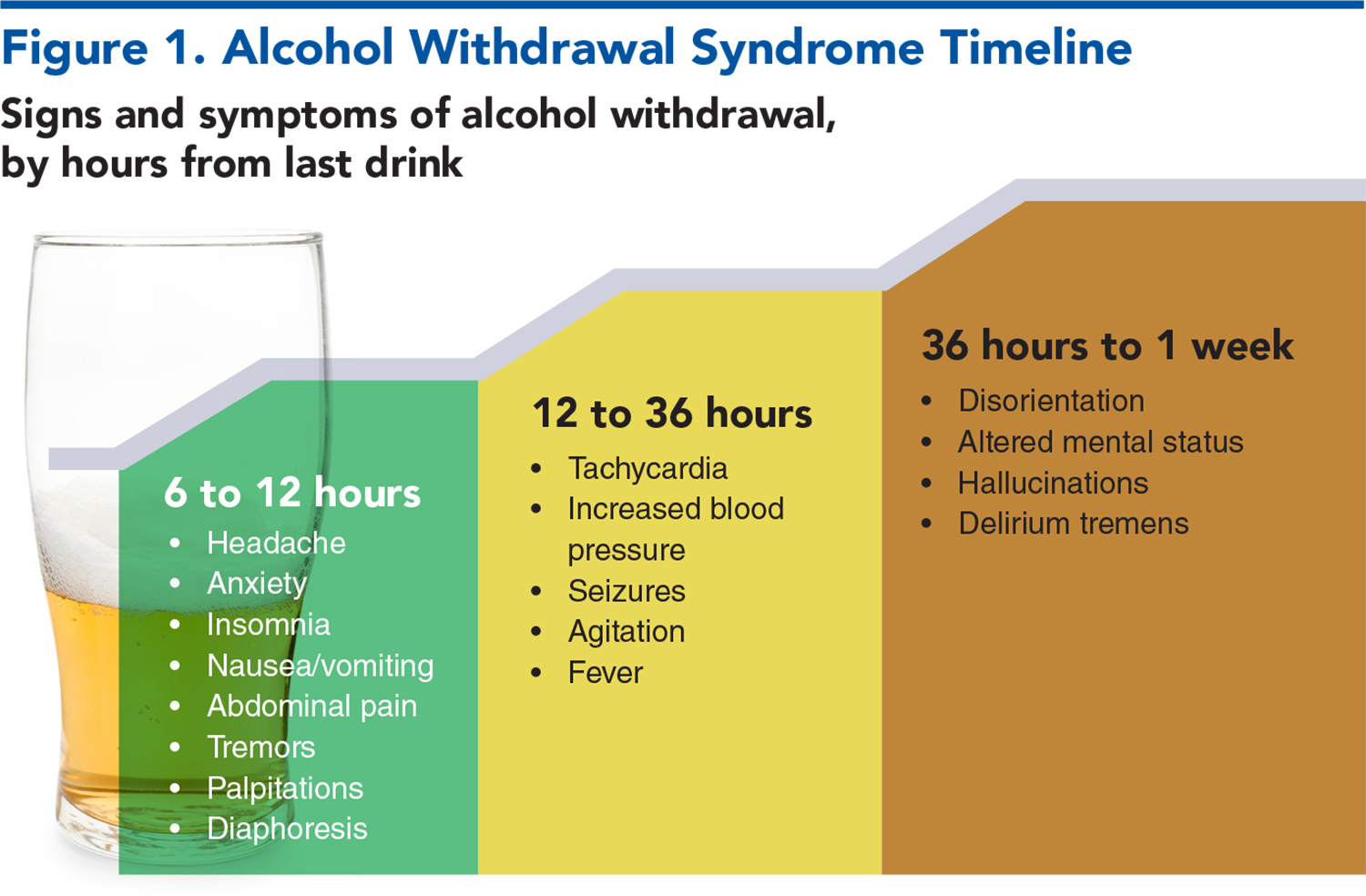
How the patient’s history of alcohol use, cessation, and previous alcohol withdrawal can help determine where they fall on the timeline of symptoms.
What the criteria and risk factors for complicated AWS are, and the medications that can blunt symptoms.
How to use scoring tools for AWS, including the CIWA-Ar, BAWS, and PAWSS.
Choosing the best benzodiazepine for symptom-triggered treatment: shorter time to onset versus longer half-life, and cautions for intubated patients and those with liver disease.
Recommendations on the use of phenobarbital for AWS, with or without benzodiazepine.
The current evidence on the use of ketamine, gabapentin, acamprosate, magnesium, and antiseizure medications.
Discharge with detoxification referral, admission to inpatient treatment, or to ICU? How to track symptoms for the best outcome.
What emergency clinicians need to know about medications for AWS prevention, prophylaxis, and outpatient tapering, and whether treatment for alcohol use disorder should begin in the ED.
- About This Issue
- Acknowledgement
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Sobering Centers
- Emergency Department Evaluation
- History
- Physical Examination
- Scoring the Severity of Alcohol Withdrawal
- Complicated Alcohol Withdrawal
- Alcohol Withdrawal Hallucinosis
- Alcohol Withdrawal Seizures
- Delirium Tremens
- Diagnostic Studies
- Laboratory Studies
- Electrocardiogram
- Imaging Studies
- Treatment
- Treatment Strategies for Alcohol Withdrawal Syndrome
- Benzodiazepines
- Phenobarbital
- Adjunctive Therapy
- Prevention and Prophylaxis
- Special Populations
- The Complicated Withdrawal Patient
- The Intubated Patient
- The Patient With End-Stage Liver Disease
- The Pregnant Patient
- Controversies and Cutting Edge
- N-Methyl-D-Aspartate Receptor Antagonists
- Ketamine
- Acamprosate
- Magnesium
- Gabapentin
- Antiseizure Medications
- Dexmedetomidine
- Baclofen
- Disposition
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Patients With Alcohol Withdrawal Syndrome
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
- Clinical Pathway for Emergency Department Management of Alcohol Withdrawal Syndrome
- Tables and Figures
- References
Abstract
Alcohol withdrawal syndrome is a constellation of symptoms and signs resulting from the abrupt decrease or cessation of heavy alcohol use. Complications of alcohol withdrawal syndrome present significant dangers for patient morbidity and mortality, as well as burdens on emergency department resources. This review presents an overview of the pathophysiology of alcohol withdrawal syndrome and a systematic approach for management in the emergency department. Current evidence on treatment regimens and adjunctive therapies is reviewed, and recommendations for management of patients with alcohol use disorders are discussed.
Case Presentations
- He said he consumes about a fifth (750 mL) of whisky daily, and he says he has a history of alcohol withdrawal seizures. His last drink was about 24 hours ago.
- EMS checked his fingerstick blood glucose, which was normal, and administered 1 liter of IV 0.9% saline.
- His heart rate is 120 beats/min and his blood pressure is 163/92 mm Hg. He is oriented, but tremulous, anxious, and sweating.
- You consider your options to help control his symptoms quickly and prevent a repeat seizure...
- EMS transported him to the ED after reports of a man stumbling into the middle of traffic.
- You see a malnourished-looking man attempting to get out of the stretcher, swaying back and forth.
- His vital signs are unattainable, but he appears diaphoretic, altered, and his extremities are hot to the touch. He is moaning, “No, no, no,” and grasping at the air.
- You note in his records that he was seen for alcohol intoxication and a fall 4 days prior. His head and cervical spine CT scans were negative.
- You consider whether this patient has capacity, and what your best next steps would be...
- She says she normally imbibes 2 bottles of wine a day, and her last drink was about 12 hours ago.
- She has a history of withdrawal, but no hospitalizations for seizures or hallucinations.
- After 4 hours into your shift, the nurse informs you that the patient’s CIWA-Ar is 7, she is feeling anxious, and wishes to discuss detoxification options with you. To prepare for the discussion, you review the options for outpatient care resources you can offer, in order to prevent further withdrawal, and control her cravings...
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
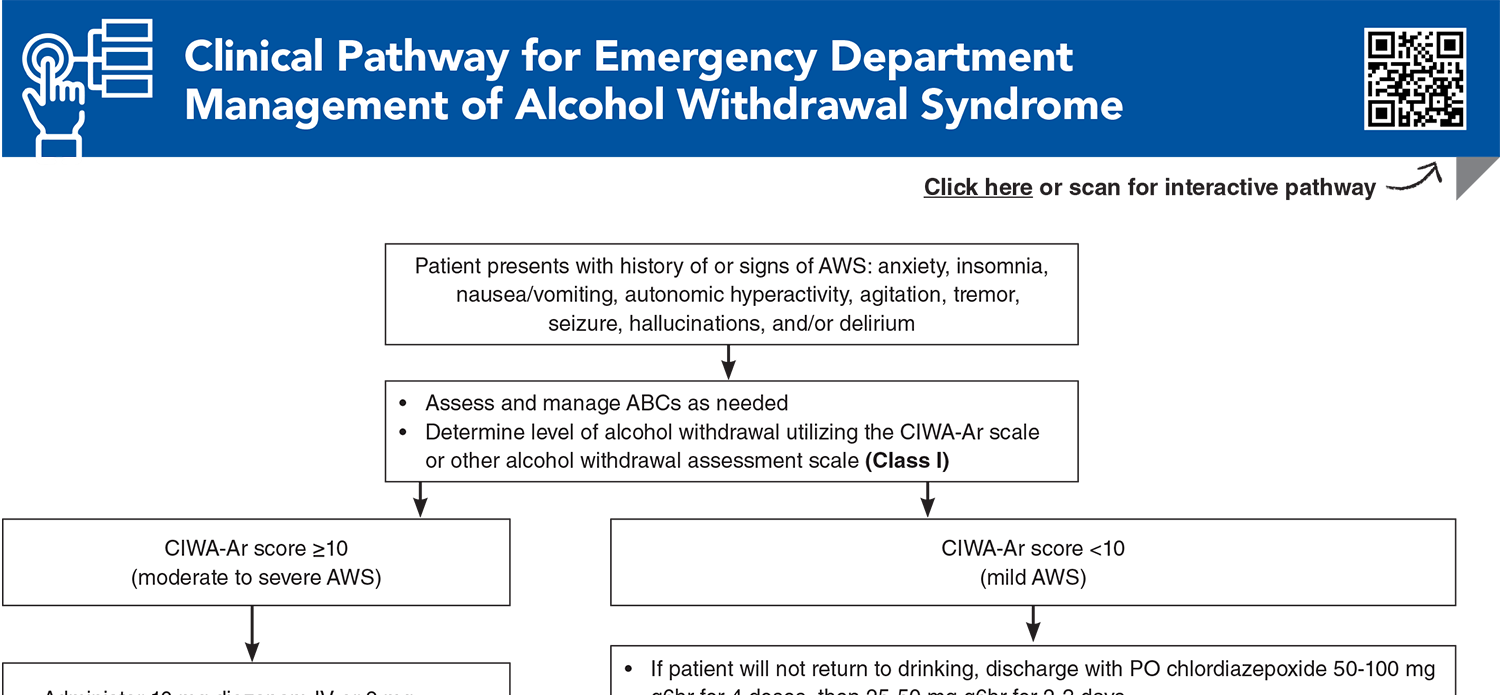
Clinical Pathway for Emergency Department Management of Alcohol Withdrawal Syndrome
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Strayer RJ, Friedman BW, Haroz R, et al. Emergency department management of patients with alcohol intoxication, alcohol withdrawal, and alcohol use disorder: a white paper prepared for the American Academy of Emergency Medicine. J Emerg Med. 2023;64(4):517-540. (White paper/clinical guidelines) DOI: 10.1016/j.jemermed.2023.01.010
4. * Kast KA, Sidelnik SA, Nejad SH, et al. Management of alcohol withdrawal syndromes in general hospital settings. BMJ. 2025;388:e080461. (Review) DOI: 10.1136/bmj-2024-080461
7. * The ASAM clinical practice guideline on alcohol withdrawal management. J Addict Med. 2020;14(3S Suppl 1):1-72. (Clinical practice guidelines) DOI: 10.1097/ADM.0000000000000668
8. * Borgundvaag B, Bellolio F, Miles I, et al. Guidelines for reasonable and appropriate care in the emergency department (GRACE-4): alcohol use disorder and cannabinoid hyperemesis syndrome management in the emergency department. Acad Emerg Med. 2024;31(5):425-455. (Clinical practice guidelines) DOI: 10.1111/acem.14911
71. * Pourmand A, AlRemeithi R, Kartiko S, et al. Evaluation of phenobarbital based approach in treating patient with alcohol withdrawal syndrome: a systematic review and meta-analysis. Am J Emerg Med. 2023;69:65-75. (Systematic review and meta-analysis; 12 articles, 1934 patients) DOI: 10.1016/j.ajem.2023.04.002
85. * Wolf C, Curry A, Nacht J, et al. Management of alcohol withdrawal in the emergency department: current perspectives. Open Access Emerg Med. 2020;12:53-65. (Review) DOI: 10.2147/OAEM.S235288
106. *McPheeters M, O’Connor EA, Riley S, et al. Pharmacotherapy for alcohol use disorder: a systematic review and meta-analysis. JAMA. 2023;330(17):1653-1665. (Systematic review and meta-analysis; 118 articles; 20,976 patients) DOI: 10.1001/jama.2023.19761
Subscribe to get the full list of 123 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: ethanol, tachycardia, withdrawal, hypertension, tremor, diaphoresis, benzodiazepine, CIWA-Ar, hallucinosis, seizure, delirium, kindling, phenobarbital, ketamine, gabapentin, anti-craving