Table of Contents
About This Issue
When a patient presents to the ED exhibiting symptoms of sympathomimetic toxidrome, including agitation, prompt management will not only treat the patient’s dangerous complications, but can assist in ED management of patients who can be resource-intensive. In this issue you will learn:
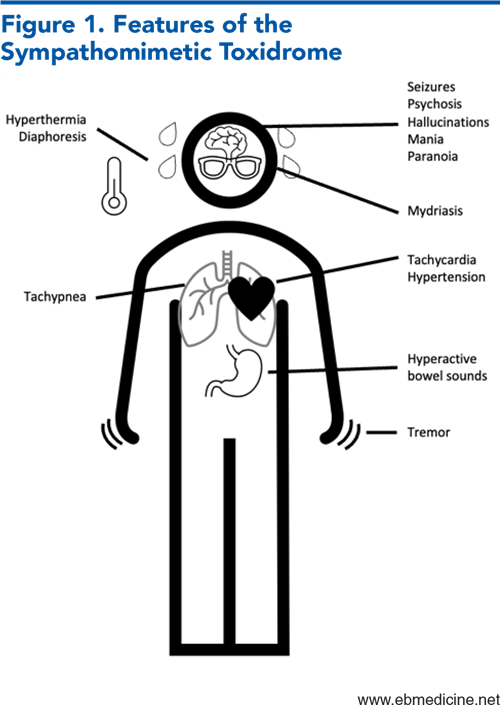
The symptoms of the sympathomimetic toxidrome, and how to distinguish it from other toxidromes.
How to manage the most dangerous complications of methamphetamine toxicity: rhabdomyolysis, acute kidney injury, and cardiovascular/cerebrovascular complications.
The symptoms of methamphetamine withdrawal and how to distinguish it from withdrawal from other substances.
Why hyperthermia is an urgent concern in these patients, and how to best treat it.
Benzodiazepines and antipsychotics: when to use each (or both).
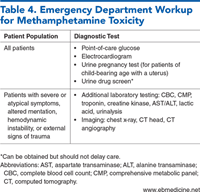
The must-do laboratory tests for all patients and the symptoms that call for further testing.
Whether to use antihypertensives.
The circumstances when toxicology screening should be performed.
-
About This Issue
-
Abstract
-
Case Presentations
-
Introduction
-
Critical Appraisal of the Literature
-
Etiology And Pathophysiology
-
Dangerous Complications of Methamphetamine Use
-
Rhabdomyolysis and Acute Kidney Injury
-
Cardiovascular and Cerebrovascular Complications
-
Methamphetamine Withdrawal
-
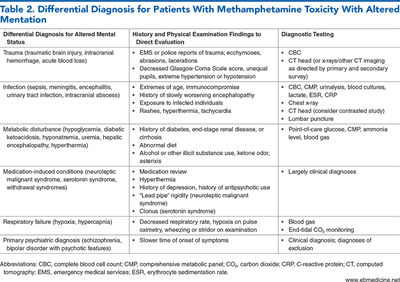
Differential Diagnosis
-
Prehospital Care
-
Medications
-
Restraints
-
Gathering On-Scene Information
-
Emergency Department Evaluation
-
History
-
Physical Examination
-
Diagnostic Studies
-
Electrocardiogram
-
Urine Drug Screen
-
Additional Laboratory Studies
-
Imaging Studies
-
Treatment
-
Treatment of Acute Agitation and Psychosis
-
Benzodiazepines and Antipsychotic Agents
-
Adjunct Medications
-
Airway Manaagement
-
Treatment of Vital Sign Abnormalities
-
Antihypertensives
-
Antipyretics
-
Treatment of Withdrawal
-
Special Populations
-
Elderly Patients
-
Pediatric Patients
-
Pregnant Patients
-
Controversies and Cutting Edge
-
Disposition
-
5 Things That Will Change Your Practice
-
Risk Management Pitfalls for Emergency Department Patients With Methamphetamine Intoxication
-
Summary
-
Time- and Cost-Effective Strategies
-
Case Conclusions
-
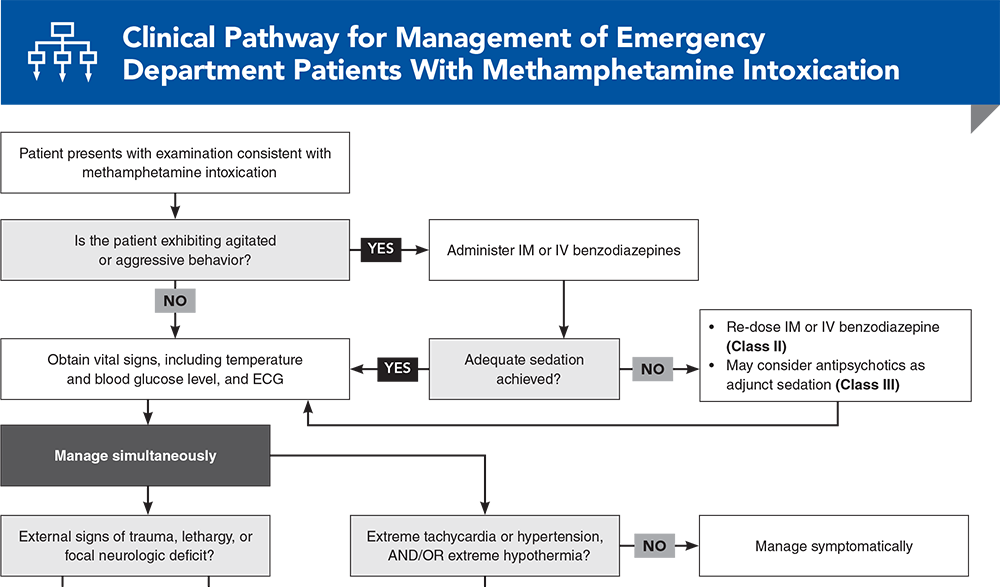
Clinical Pathway for Management of Emergency Department Patients With Methamphetamine Intoxication
-
Tables and Figures
-
References
Abstract
Management of patients who are acutely intoxicated with methamphetamine (a member of the substituted amphetamine class of drugs) can be resource-intensive for most emergency departments. Clinical presentations of the methamphetamine sympathomimetic toxidrome range from mild agitation to rhabdomyolysis, acute kidney injury, seizures, and intracranial hemorrhage. High-quality evidence on how to best manage these patients is lacking, and most research focuses on symptomatic interventions to control patients‘ agitation and hemodynamics. This review analyzes the best available evidence on the diagnosis and management of emergency department patients with substituted amphetamine toxicity and offers best-practice recommendations on treatment and disposition.
Case Presentations
-
When you approach the patient, you find an 18-year-old woman who gives you her name but does not respond appropriately to orienting questions. She is cooperative at first, but then starts to become increasingly agitated when you try to obtain further history.
-
Her vital signs are: temperature, 37°C; blood pressure, 170/99 mm Hg; heart rate, 120 beats/min; and respiratory rate, 16 breaths/min. She is diaphoretic, but neurologically intact and without any evidence of trauma.
-
She becomes uncooperative and starts to threaten the staff. Your attempts at de-escalation with redirection and relocation fail, and you wonder what the best pharmacologic intervention would be...
-
He admits to taking an “upper,” but says that he is unsure of the specific substance.
-
His vital signs are: temperature, 36.6°C; blood pressure, 170/110 mm Hg; heart rate, 115 beats/min; and respiratory rate, 14 breaths/min. His electrocardiogram is negative for ischemic changes.
-
He denies any cardiac history or risk factors for pulmonary embolism. You wonder whether this young man needs to have a cardiac workup . . .
-
The EMTs report that the patient is otherwise healthy and had a witnessed seizure in front of family. Her family denies any prior history of seizure.
-
Upon arrival, the patient is disoriented and unable to provide further history. Her vital signs are: temperature, 37.1°C; blood pressure, 190/120 mm Hg; heart rate, 116 beats/min; and respiratory rate, 12 breaths/min.
-
You wonder whether her depressed consciousness is due to the seizure or if something else could be going on . . .
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Emergency Department Patients With Methamphetamine Intoxication
Subscribe to access the complete flowchart to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
4. * Schep LJ, Slaughter RJ, Beasley DM. The clinical toxicology of metamfetamine. Clin Toxicol (Phila). 2010;48(7):675-694. (Review) DOI: 10.3109/15563650.2010.516752
7. * Prosser JM, Nelson LS. The toxicology of bath salts: a review of synthetic cathinones. J Med Toxicol. 2012;8(1):33-42. (Review) DOI: 10.1007/s13181-011-0193-z
24. * Richards JR, Hawkins JA, Acevedo EW, et al. The care of patients using methamphetamine in the emergency department: perception of nurses, residents, and faculty. Subst Abus. 2019;40(1):95-101. (Survey) DOI: 10.1080/08897077.2018.1449170
26. * Banks ML, Worst TJ, Rusyniak DE, et al. Synthetic cathinones (“bath salts”). J Emerg Med. 2014;46(5):632-642. (Review) DOI: 10.1016/j.jemermed.2013.11.104
Subscribe to get the full list of 43 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: methamphetamine, substituted amphetamine, cathinone, sympathomimetic, tachycardia, hyperthermia, diaphoresis, seizure, agitation, psychosis, rhabdomyolysis, acute kidney injury, benzodiazepine, antipsychotic, myoclonus