

The prevalence of elder abuse and neglect is trending upward among American seniors, but physician reports of suspected maltreatment are not keeping pace. The most important step in management of elder abuse and neglect is making the diagnosis and reporting the suspicions to Adult Protective Services. This review presents a systematic approach for emergency department diagnosis of elder abuse and neglect, including a thorough history and physical examination combined with the use of standardized validated screening tools. To better assess and treat victims of suspected abuse, physicians can also employ a multidisciplinary team or recruit available resources in the hospital and the community, such as case managers, social workers, and primary care providers to create safety plans for at-risk elders.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
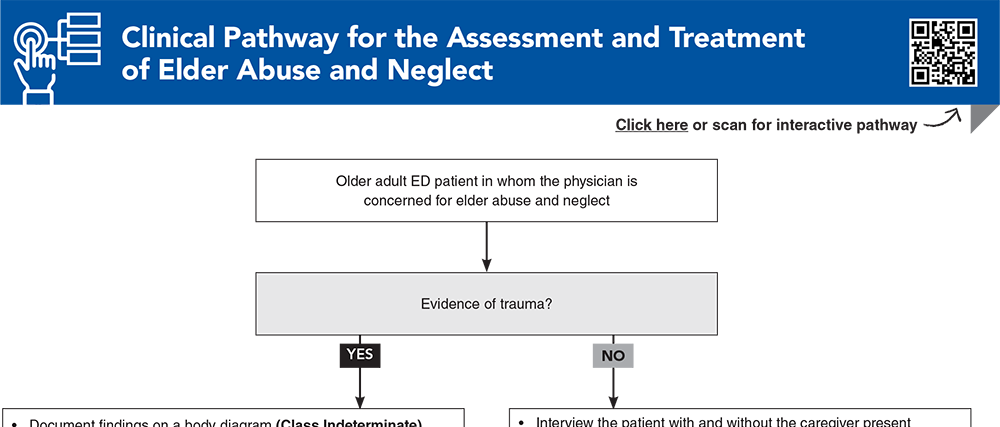
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.

Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
2. * Makaroun LK, Beach S, Rosen T, et al. Changes in elder abuse risk factors reported by caregivers of older adults during the COVID-19 pandemic. J Am Geriatr Soc. 2021;69(3):602-603. (Cross-sectional study; 433 surveys) DOI: 10.1111/jgs.17009
5. * Rosen T, Bloemen EM, LoFaso VM, et al. Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. TJ Emerg Med. 2016;50(3):518-526. (Observational study; 572 ED visits) DOI: 10.1016/j.jemermed.2015.10.037
7. * Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100(2):292-297. (Observational study; 5777 participants) DOI: 10.2105/AJPH.2009.163089
13. * Lachs MS, Pillemer K. Elder abuse. Lancet. 2004;364(9441):1263-1272. (Review) DOI: 10.1016/S0140-6736(04)17144-4
14. * Rosen T, Lien C, Stern ME, et al. Emergency medical services perspectives on identifying and reporting victims of elder abuse, neglect, and self-neglect. J Emerg Med. 2017;53(4):573-582. (Qualitative, cross-sectional study; 350 paramedics) DOI: 10.1016/j.jemermed.2017.04.021
22. * Lee M, Rosen T, Murphy K, et al. A new role for imaging in the diagnosis of physical elder abuse: results of a qualitative study with radiologists and frontline providers. J Elder Abuse Negl. 2019;31(2):163-180. (Qualitative study; 25 participants) DOI: 10.1080/08946566.2019.1573160
27. * Yaffe MJ, Wolfson C, Lithwick M, et al. Development and validation of a tool to improve physician identification of elder abuse: the Elder Abuse Suspicion Index (EASI)©. J Elder Abuse Negl. 2008;20(3):276-300. (Observational study; 953 patients) DOI: 10.1080/08946560801973168
44. * Rosen T, Bao Y, Zhang Y, et al. Identifying patterns of health care utilisation among physical elder abuse victims using Medicare data and legally adjudicated cases: protocol for case-control study using data linkage and machine learning. BMJ Open. 2021;11(2):e044768. (Case control; 204 legally adjudicated cases of elder abuse) DOI: 10.1136/bmjopen-2020-044768
Subscribe to get the full list of 46 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: elderly, abuse, neglect, reporting, geriatric, caregiver, dependency, cognitive, social, bruise, purpura, protective, EASI, screening
Nicole Cimino-Fiallos, MD, FACEP
Cortlyn F. Jeter, MD, FACEP; Ashley Shreves, MD
September 1, 2024
September 1, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 ACEP Category I Credits, 4 AAFP Prescribed Credits, 4 AOA Category 2-B Credits. Specialty CME Credits:Included as part of the 4 credits, this CME activity is eligible for 2 Domestic Violence CME credits and 4 Geriatrics CME credits, subject to your state and institutional approval.