Table of Contents
About This Issue
For many patients with opioid use disorder (OUD) in the United States, an ED presentation for overdose or withdrawal crisis may be their only contact with the healthcare system. In addition to managing these patients’ acute medical events, evidence is emerging that emergency clinicians can have a significant, positive effect in helping these patients with ED initiation of medication for OUD: MOUD. In this issue, you will learn:
How to manage patients with opioid intoxication by recognizing the signs and treating the respiratory and central nervous system depression: naloxone dosing, routes of administration, timing, and cautions.
How to recognize and manage potential multidrug ingestions, and when CT imaging might be indicated.
Strategies for recognizing when a patient is in opioid withdrawal, using the COWS score to calculate severity.
The risks, benefits, and cautions for the 3 drugs approved for MOUD: methadone, buprenorphine, and naltrexone.
Initiating buprenorphine in the ED: when to start, recommended dosages according to opioids used, and avoiding precipitating withdrawal symptoms.
Strategies for managing patients who are pregnant, in police custody, without stable housing, or currently using methadone, as well as the importance of follow-up care.
New strategies in buprenorphine initiation: low-dose, high-dose, long-acting, and home initiation.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Epidemiology
- Pathophysiology
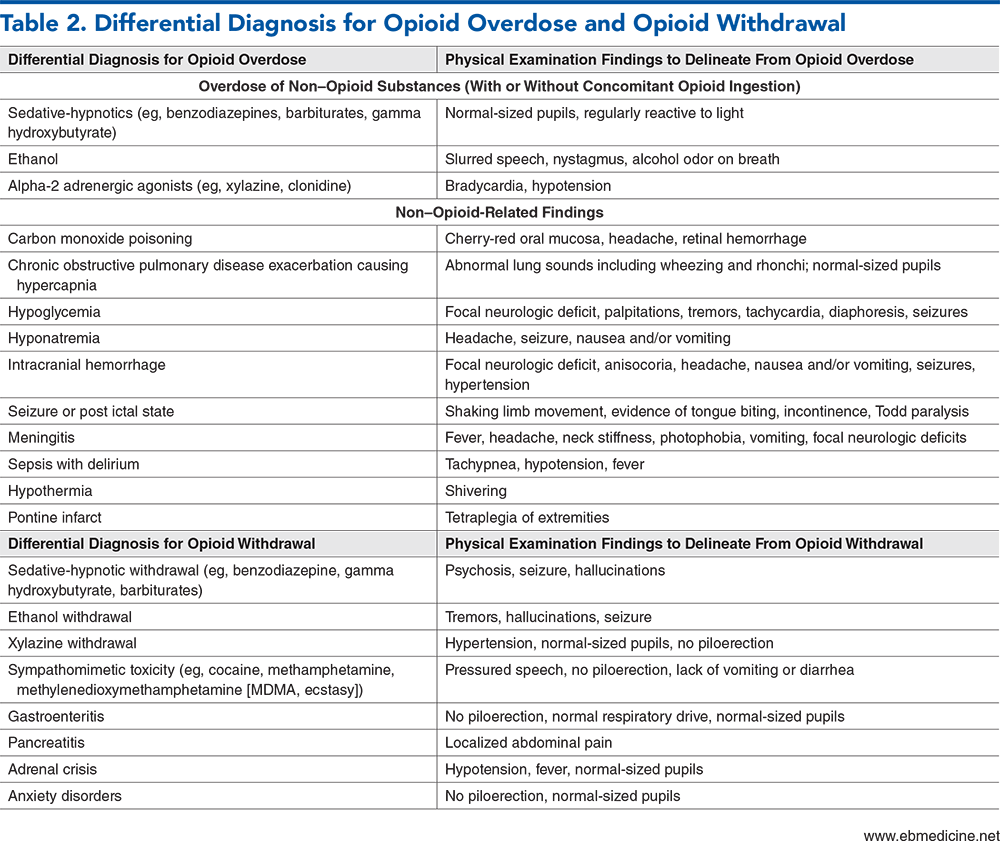
- Differential Diagnosis
- Prehospital Care
- Opioid Overdose
- Opioid Withdrawal
- Emergency Department Evaluation
- History
- Physical Examination
- Potential Opioid Overdose
- Potential Opioid Withdrawal
- Diagnostic Studies
- Laboratory Studies
- Complete Blood Cell Count, Basic Metabolic Panel, Creatinine Phosphokinase
- Venous Blood Gas
- Urine Drug Screen
- Urine Pregnancy Testing
- Lumbar Puncture
- Electrocardiogram
- Imaging Studies
- Chest X-Ray
- Computed Tomographic Imaging
- Magnetic Resonance Imaging
- Treatment
- Opioid Overdose
- Opioid Withdrawal
- Supportive Care
- Emergency Department Initiation of Medications for Opioid Use Disorder
- Screening, Brief Intervention, and Referral to Treatment
- Buprenorphine
- Barriers to Buprenorphine Use
- Buprenorphine Initiation
- Methadone
- Naltrexone
- Special Populations
- Pregnant Patients
- Pediatric Patients
- Patients Without Stable Housing
- Patients Accompanied by Police
- Controversies and Cutting Edge
- Newer Approaches to Buprenorphine Dosing
- High-Dose Buprenorphine
- Low-Dose Buprenorphine
- ED-Initiated Buprenorphine Following Mu-Opioid Antagonist-Induced Opioid Withdrawal
- Long-Acting Injectable Buprenorphine Formulation Use in the Emergency Department
- Nalmefene
- Opioid Vaccines and Monoclonal Antibodies
- Disposition
- Opioid Overdose
- Opioid Withdrawal
- Summary
- Opioid Overdose
- Opioid Withdrawal
- Time- and Cost-Effective Strategies
- Risk Management Pitfalls for Managing Emergency Department Patients With Opioid Use Disorder
- 5 Things That Will Change Your Practice
- Case Conclusions
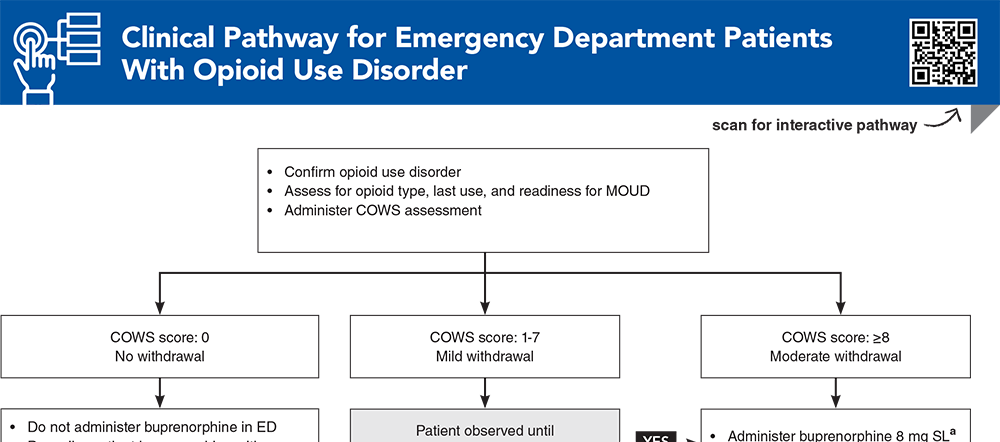
- Clinical Pathway for Emergency Department Patients With Opioid Use Disorder
- Tables and Figures
- References
Abstract
As the United States continues to grapple with the opioid crisis, emergency clinicians are on the front lines of managing patients with opioid use disorder. This issue reviews tools and best practices in emergency department management of patients with opioid overdose and opioid withdrawal, and how substance use history will inform treatment planning and disposition. As growing evidence shows that medications for opioid use disorder (MOUD)—buprenorphine, methadone, and naltrexone—can have lasting impacts on patients’ addiction recovery, strategies for assessing patient readiness for MOUD and overcoming barriers to emergency department initiation of these medications are reviewed. Newer approaches to buprenorphine dosing (high-dose, low-dose, home induction, and long-acting injectable dosing) are also reviewed.
Case Presentations
- The patient starts to raise his voice asking for the medication. His vital signs are normal.
- As you assess the patient for opioid withdrawal, he is pacing the room and reports experiencing chills, body aches, and abdominal cramping. The patient states that he feels very anxious.
- Physical examination reveals normal-sized pupils, rhinorrhea, and piloerection. You calculate a Clinical Opiate Withdrawal Scale (COWS) score of 12 and think to yourself: Can this patient be safely started on medication for opioid use disorder, and if so, should I give methadone or offer another medication?
- The paramedics report that there was drug paraphernalia at the scene. They state that they found the patient to be apneic with pinpoint pupils, and despite administration of 4 mg of intranasal naloxone she continues to have poor respiratory effort.
- What are your next steps? Are there any adulterants that could exacerbate an opioid toxidrome?
- When you speak with them, they report that they receive 100 mg of oral methadone daily for opioid use disorder (OUD), and their last dose was yesterday morning.
- You recently learned about using buprenorphine as treatment for OUD. You wonder whether the patient would be more satisfied with a 30-day prescription of buprenorphine rather than having to visit a methadone clinic daily. Can patients on methadone be safely transitioned to buprenorphine without precipitating withdrawal?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Patients With Opioid Use Disorder
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
10. * D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636-1644. (Randomized control trial; 329 patients) DOI: 10.1001/jama.2015.3474
11. Moe J, Badke K, Pratt M, et al. Microdosing and standard-dosing take-home buprenorphine from the emergency department: a feasibility study. J Am Coll Emerg Physicians Open. 2020;1(6):1712-1722. (Randomized feasibility trial; 54 patients) DOI: 10.1002/emp2.12289
23. * Greenwald MK, Herring AA, Perrone J, et al. A neuropharmacological model to explain buprenorphine induction challenges. Ann Emerg Med. 2022;80(6):509-524. (Review article) DOI: 10.1016/j.annemergmed.2022.05.032
60. * Childers R, Castillo EM, Cronin AO, et al. Emergency department-initiated buprenorphine treatment in a population with a high rate of homelessness: an observational study. J Emerg Med. 2023;64(2):129-135. (Descriptive analysis; 210 patients) DOI: 10.1016/j.jemermed.2022.12.004
73. * Whiteside LK, D’Onofrio G, Fiellin DA, et al. Models for implementing emergency department-initiated buprenorphine with referral for ongoing medication treatment at emergency department discharge in diverse academic centers. Ann Emerg Med. 2022;80(5):410-419. (Project proposal and description) DOI: 10.1016/j.annemergmed.2022.05.010
87. * Snyder H, Chau B, Kalmin MM, et al. High-dose buprenorphine initiation in the emergency department among patients using fentanyl and other opioids. JAMA Netw Open. 2023;6(3):e231572. (Retrospective cohort study; 439 patients) DOI: 10.1001/jamanetworkopen.2023.1572
Subscribe to get the full list of 98 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: opioid, disorder, MOUD, withdrawal, overdose, methadone, buprenorphine, naloxone, naltrexone, fentanyl, xylazine, COWS