Table of Contents
About This Issue
Status epilepticus is the most common life-threatening neurologic emergency in childhood, and there continues to be significant associated morbidity and mortality. Over the last few decades, the definition and management of status epilepticus has evolved. This issue reviews the updated International League Against Epilepsy (ILAE) definition of status epilepticus and discusses evidence-based medication recommendations and treatment protocols for management of pediatric status epilepticus in the emergency department. In this issue, you will learn:
The definitions of the different types of status epilepticus, as well as the updated ILAE definition of status epilepticus and classification of convulsive status epilepticus
Conditions in the broad differential diagnosis of status epilepticus
Evidence-based recommendations for prehospital care and initial management in the emergency department
Key information to elicit when obtaining the history and components of the physical examination that need to be included
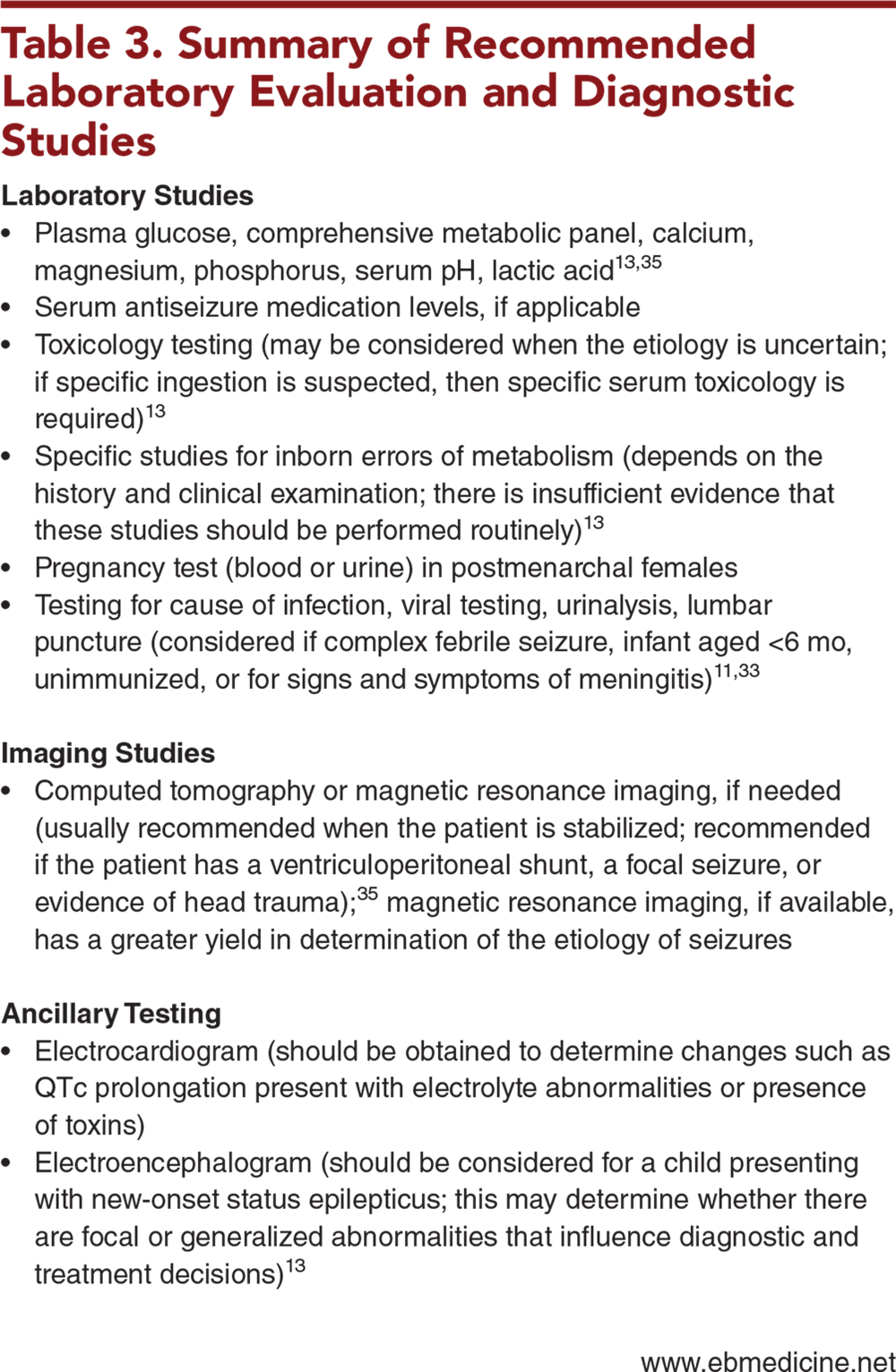
Recommended laboratory, imaging, and ancillary testing to diagnose status epilepticus
Evidence-based recommendations for first-, second-, and third-line medications to abort seizure activity
Special considerations for neonatal seizures, febrile status epilepticus, eclampsia, and functional neurologic disorder
Topics of ongoing research including adjunctive diagnostic studies and therapies
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- Initial Management
- Airway and Breathing
- Circulation
- Disability/Exposure
- History
- Physical Examination
- Diagnostic Studies
- Treatment
- First-Line Medications
- Second- and Third-Line Medications
- Continuous Infusion
- Treatment of Electrolyte Abnormalities
- Hypoglycemia
- Hyponatremia
- Hypocalcemia
- Special Considerations
- Neonatal Seizures
- Febrile Status Epilepticus
- Eclampsia
- Functional Neurologic Disorder
- Controversies and Cutting Edge
- Point-of-Care Electroencephalogram Devices
- Surgical Options
- Ketogenic Diet
- Lacosamide
- Brivaracetam
- NORSE and FIRES
- Ketamine and Topiramate
- Disposition
- Risk Management Pitfalls in the Management of Pediatric Status Epilepticus in the Emergency Department
- 5 Things That Will Change Your Practice
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
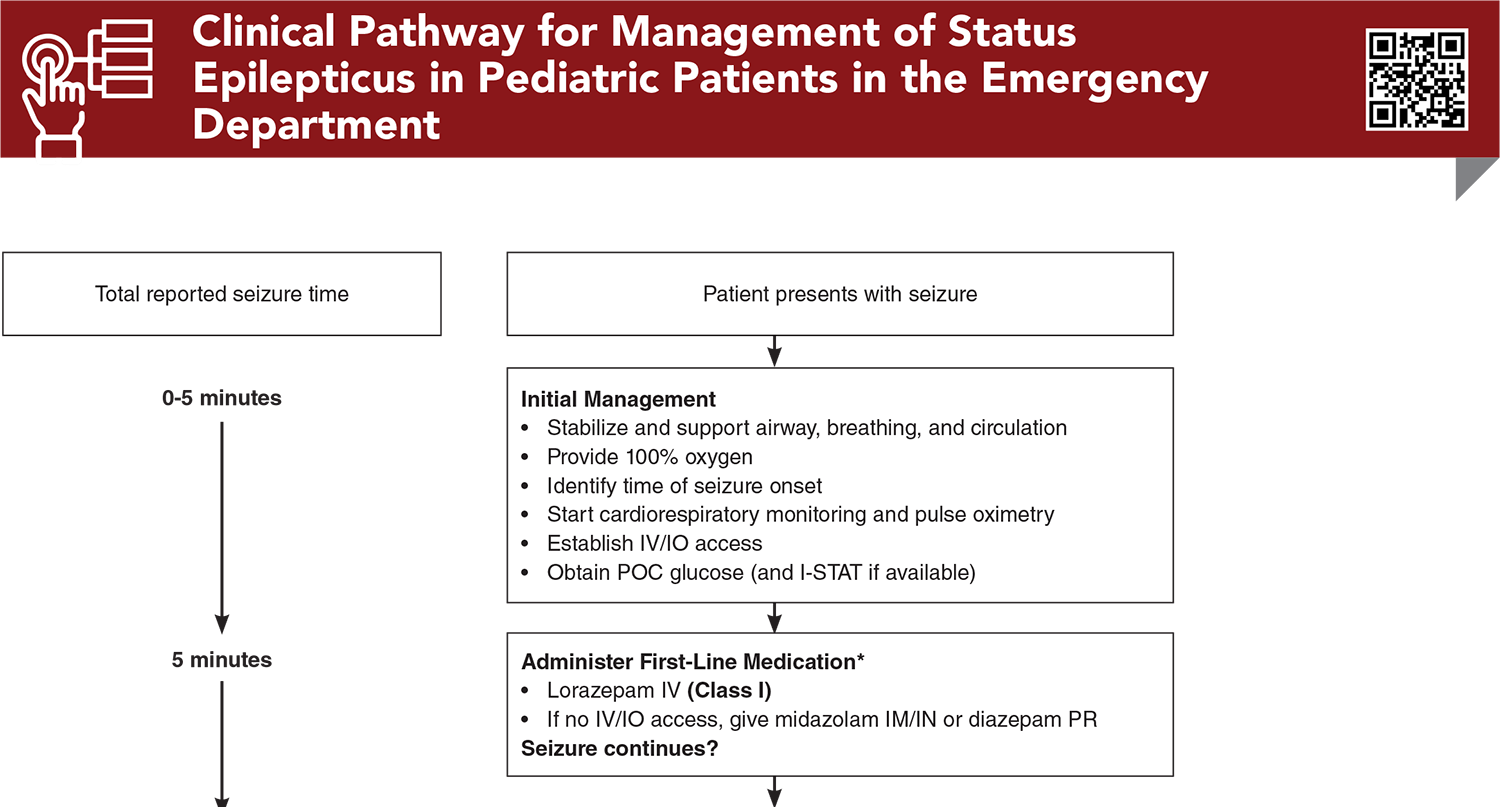
- Clinical Pathway for Management of Status Epilepticus in Pediatric Patients in the Emergency Department
- Tables
- References
Abstract
Pediatric status epilepticus requires prompt recognition and treatment in the emergency department. When left untreated, status epilepticus can lead to neuronal death, neuronal injury, and alteration of neuronal networks, depending on the type and duration of the seizures. This issue reviews the International League Against Epilepsy definition of status epilepticus and provides recommendations for the evaluation and management of pediatric patients presenting to the emergency department in status epilepticus.
Case Presentations
- The mother tells you the infant is breastfed, and that she thinks that he is not getting enough milk.
- On examination, the boy’s vital signs are: rectal temperature, 36.6°C; heart rate, 180 beats/min; blood pressure, 80/40 mm Hg; respiratory rate, 40 breaths/min; and oxygen saturation, 95% on room air. Tonic-clonic movements of the arms and legs with deviation of the eyes are noted, during which the infant is not interacting with the parent. This activity has been going on for 5 minutes. The neurologic examination is otherwise nonfocal. The airway is intact, and the infant is breathing spontaneously. Capillary refill is 3 seconds. Tympanic membranes are normal, and the anterior fontanelle is open and flat. No scalp swelling or skin bruising is noted.
- Based on the patient’s age and presentation, what differential diagnoses should be considered? What testing should be performed in the first 5 minutes following presentation? What medication or treatment will abort seizure activity?
- The girl’s mother tells you the child is fully immunized and has had a runny nose for the past 3 days and fever for 1 day.
- On examination, the girl’s vital signs are: temperature, 39.4°C; heart rate, 150 beats/min; blood pressure, 82/50 mm Hg; respiratory rate, 32 breaths/min; and oxygen saturation, 94% on room air. The girl’s airway is intact and she is breathing spontaneously, with clear breath sounds bilaterally. Her capillary refill is 2 seconds. Her tympanic membranes are normal, and her anterior fontanelle is open and flat. No scalp swelling or skin bruising is noted. The neurologic examination is nonfocal, and no further seizure activity is noted.
- Based on the patient’s age and presentation, what is the most likely differential diagnosis? Does this patient require a lumbar puncture? What medications should you consider administering?
- The patient takes levetiracetam at home for seizures. Diazepam per rectum was given by the mother, but seizure activity persists.
- On examination, the boy’s vital signs are: temperature, 36.4°C; heart rate, 132 beats/min, blood pressure, 165/85 mm Hg; respiratory rate, 24 breaths/min; and oxygen saturation, 95% on room air. The boy’s airway is intact, and he is breathing spontaneously. Capillary refill is 2 seconds. The patient has tonic-clonic movements of the bilateral upper and lower extremities, with eyes deviated to the left. The neurologic examination is otherwise nonfocal.
- You order a bedside glucose test, comprehensive metabolic panel, magnesium, phosphorus, urine toxicology and urinalysis, computed tomography brain, and shunt x-rays.
- How does the presence of a ventriculoperitoneal shunt impact the differential diagnosis? Does the presence of the shunt change management? What medication should you give next?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Status Epilepticus in Pediatric Patients in the Emergency Department
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Seinfeld S, Shinnar S, Sun S, et al. Emergency management of febrile status epilepticus: results of the FEBSTAT study. Epilepsia. 2014;55(3):388-395. (Prospective; 199 patients) DOI: 10.1111/epi.12526
6. * Minardi C, Minacapelli R, Valastro P, et al. Epilepsy in children: from diagnosis to treatment with focus on emergency. J Clin Med. 2019;8(1):39. (Review) DOI: 10.3390/jcm8010039
7. * Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus - report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56(10):1515-1523. (Review) DOI: 10.1111/epi.13121
9. * Kazl C, LaJoie
35. * Brophy GM, Bell R, Claasen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3-23. (Practice guideline) DOI: 10.1007/s12028-012-9695-z
Subscribe to get the full list of 85 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: status epilepticus, seizure, convulsive status epilepticus, nonconvulsive status epilepticus, focal motor status epilepticus, myoclonic status epilepticus, super-refractory convulsive status epilepticus, refractory convulsive status epilepticus, established convulsive status epilepticus, impending convulsive status epilepticus, antiseizure medication, antiepileptic drug, antiepileptic medication, first-line medication, second-line medication, third-line medication, continuous infusion, electrolyte abnormalities, neonatal seizure, febrile status epilepticus, eclampsia, functional neurologic disorder, point-of-care electroencephalogram