

Although there is a large body of existing research on traumatic intracranial hemorrhage, there are few clear and consistent recommendations that have emerged. Appropriate management is guided by an understanding of the pathophysiology of traumatic brain injury as well as by clinical observation and radiographic assessment. This review provides a comprehensive analysis of the literature and recommendations based on the best available evidence, including expeditious management of critically elevated intracranial pressure and acquisition of follow-up studies.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
EB Medicine is excited to add a new subscriber benefit, EMP: IRrL (In Rural Life) with real-time utility for EM clinicians, especially those practicing in rural settings. This supplemental content will focus on challenges and solutions when the pressure is on and resources are limited. Learn more about EMP: IRrL here.
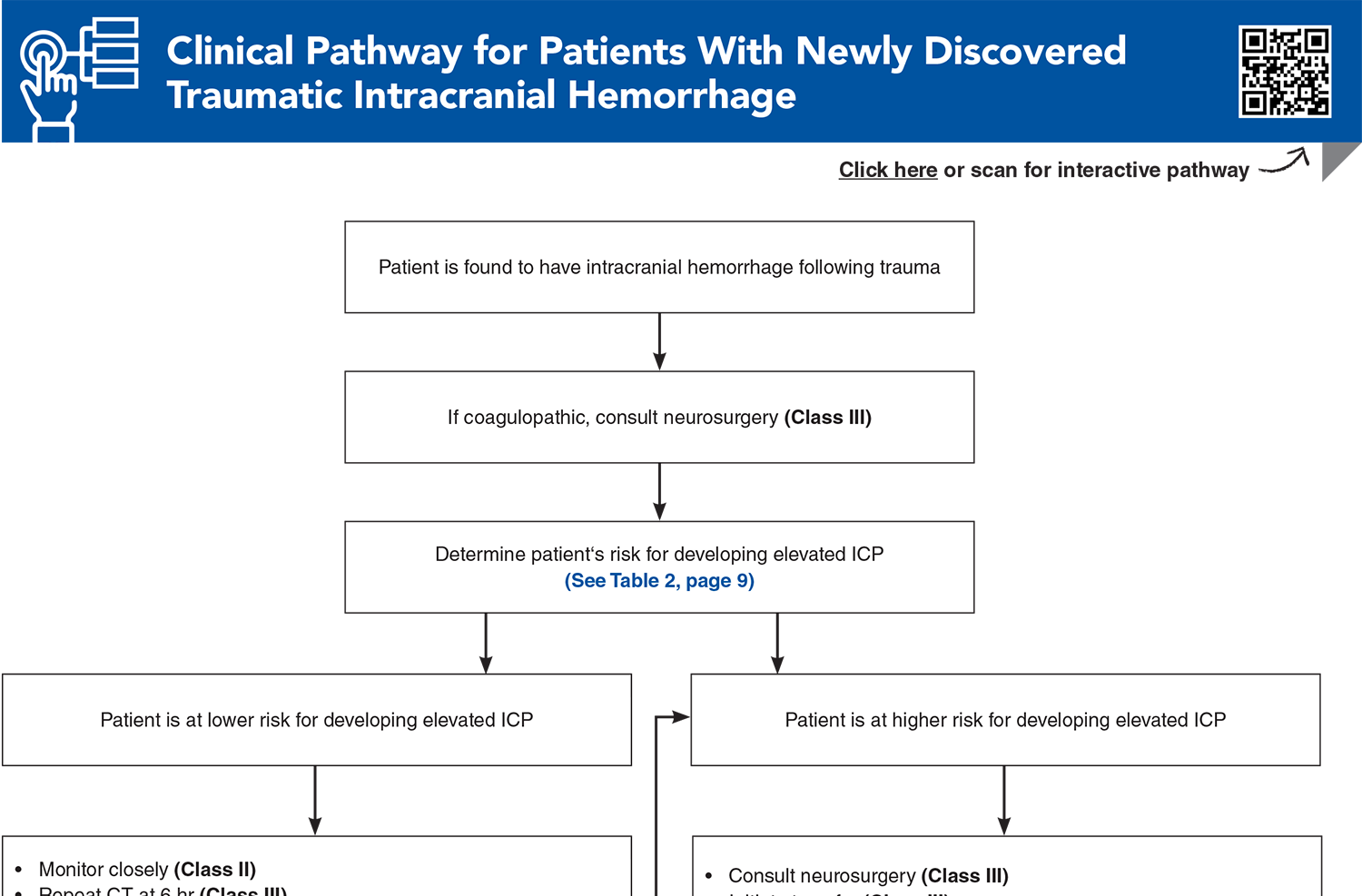
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
Subscribe for full access to all Tables and Figures.
Following are the most informative references cited in this paper, as determined by the authors.
4. * Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1):6-15. (Brain Trauma Foundation consensus guidelines) DOI: 10.1227/NEU.0000000000001432
23. * Pace J, Parry N, Vogt K, et al. A clinical prediction model for raised intracranial pressure in patients with traumatic brain injuries. J Trauma Acute Care Surg. 2018;85(2):380-386. (Retrospective cohort; 580 patients) DOI: 10.1097/TA.0000000000001965
30. * Lulla A, Lumba-Brown A, Totten AM, et al. Prehospital guidelines for the management of traumatic brain injury - 3rd edition. Prehosp Emerg Care. 2023;27(5):507-538. (Brain Trauma Foundation consensus guidelines for prehospital providers) DOI: 10.1080/10903127.2023.2187905
41. * American College of Surgeons Expert Panel. Best practice guidelines: the management of traumatic brain injury. ACS Brief. 2024. Accessed January 10, 2025. (Expert panel guidelines)
49. * Joseph B, Friese RS, Sadoun M, et al. The BIG (Brain Injury Guidelines) project: defining the management of traumatic brain injury by acute care surgeons. J Trauma Acute Care Surg. 2014;76(4):965-969. (Retrospective cohort; 3801 patients) DOI: 10.1097/TA.0000000000000161
54. * Hawryluk GWJ, Aguilera S, Buki A, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019;45(12):1783-1794. (Consensus-based algorithms) DOI: 10.1007/s00134-019-05805-9
55. * Joseph B, Obaid O, Dultz L, et al. Validating the Brain Injury Guidelines: results of an American Association for the Surgery of Trauma prospective multi-institutional trial. J Trauma Acute Care Surg. 2022;93(2):157-165. (Prospective, observational, multi-institutional trial; 2432 patients) DOI: 10.1097/TA.0000000000003554
65. * Cook AM, Morgan Jones G, Hawryluk GWJ, et al. Guidelines for the acute treatment of cerebral edema in neurocritical care patients. Neurocrit Care. 2020;32(3):647-666. (Consensus statement from the Neurocritical Care Society) DOI: 10.1007/s12028-020-00959-7
85. * Kannan S, Gillespie CS, Lee KS, et al. Diagnostic utility of Brain Injury Guidelines (BIG): systematic review and meta-analysis for prediction of neurosurgical intervention in traumatic brain injury. Brain Inj. 2024:1-8. (Systematic review and meta-analysis; 9032 patients) DOI: 10.1080/02699052.2024.2375593
Subscribe to get the full list of 85 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: traumatic, spontaneous, intracranial, hemorrhage, pressure, ICP, TBI, SAH, herniation, hematoma, intraparenchymal, GCS, asymmetry, CT, CTA, MRI, coagulopathy, blood pressure, airway
Erin D’Agostino, MD; Miguel Reyes-Zaragoza, MD, MS; Matthew Siket, MD, MHCI, FACEP; Ashley Weisman, MD (In Rural Life* )
Marc Kanter, MD, FACEP; Eric Legome, MD; Erin D'Agostino, MD (In Rural Life*)
February 1, 2025
February 1, 2028 CME Information
4 AMA PRA Category 1 Credits™, 4 ACEP Category I Credits, 4 AAFP Prescribed Credits, 4 AOA Category 2-B Credits. Specialty CME Credits:Included as part of the 4 credits, this CME activity is eligible for 4 Trauma CME credits, subject to your state and institutional approval.