Table of Contents
About This Issue
Emergency clinicians will always encounter head trauma, and thus, face the critical task of efficiently and accurately identifying those with potentially life-threatening intracranial trauma. In this issue of Emergency Medicine Practice: Trauma EXTRA!, you will learn:
How the history, mechanism of injury, and Glascow Coma Score determine indications for imaging;
When computed tomography (CT) is always indicated versus when observation is warranted;
What populations require hospital admission or specialist consultation, as well as which patients are at increased risk for intracranial injury, deterioration, and postconcussive syndrome; and
The need for careful discharge instructions for patients with mTBI.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Definitions
- Epidemiology
- Morbidity and Mortality
- Pathophysiology
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Neurological Examination
- Level of Alertness, Orientation, and Glasgow Coma Scale Score
- Head, Neck, and Cranial Nerve Examination
- Peripheral Examination
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Computed Tomography
- Key Questions/Situations in the Use of Computed Tomography
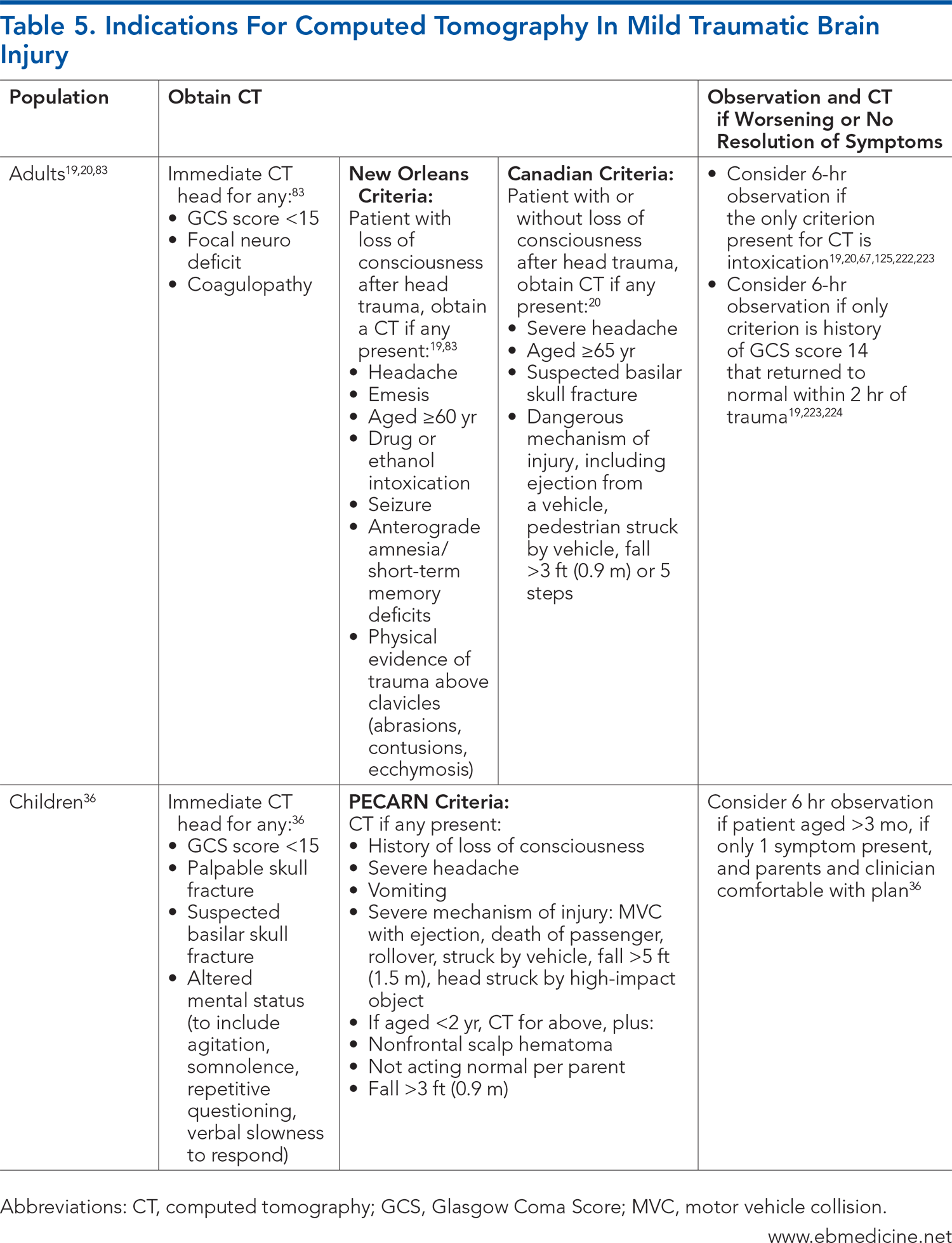
- Which patients with mild traumatic brain injury benefit from computed tomographic imaging?
- What about patients with an abnormal Glasgow Coma Scale score who return to normal in the emergency department?
- What about patients with mild traumatic brain injury who had no loss of consciousness?
- Is there such a thing as “clinically unimportant” or “inconsequential” intracranial injury?
- How do guidelines differ for children and infants, compared to adults with mild traumatic brain injury?
- What is the best diagnostic approach in infants with mild traumatic brain injury?
- Do elderly patients with mild traumatic brain injury have an increased risk of intracranial injury?
- What about patients taking anticoagulants or antiplatelet agents?
- Anticoagulants
- Antiplatelets
- Bleeding Diatheses
- Reversal Agents
- When should I be worried about delayed intracranial injury after a normal computed tomography?
- How should an intoxicated patient with suspected mild traumatic brain injury be evaluated?
- Magnetic Resonance Imaging
- Concussion and Postconcussive Syndrome
- Sports-Related Concussion
- Controversies and Cutting Edge
- Biomavrkers
- Diffusion-Weighted Imaging
- Disposition
- Risk Management Pitfalls for Mild Traumatic Brain Injuries
- Key Points for Evaluating and Treating Mild Traumatic Brain Injury
- Areas in Need of Future Research
- Conclusion
- Critical Appraisal of the Literature
- Case Conclusions
- Clinical Pathways
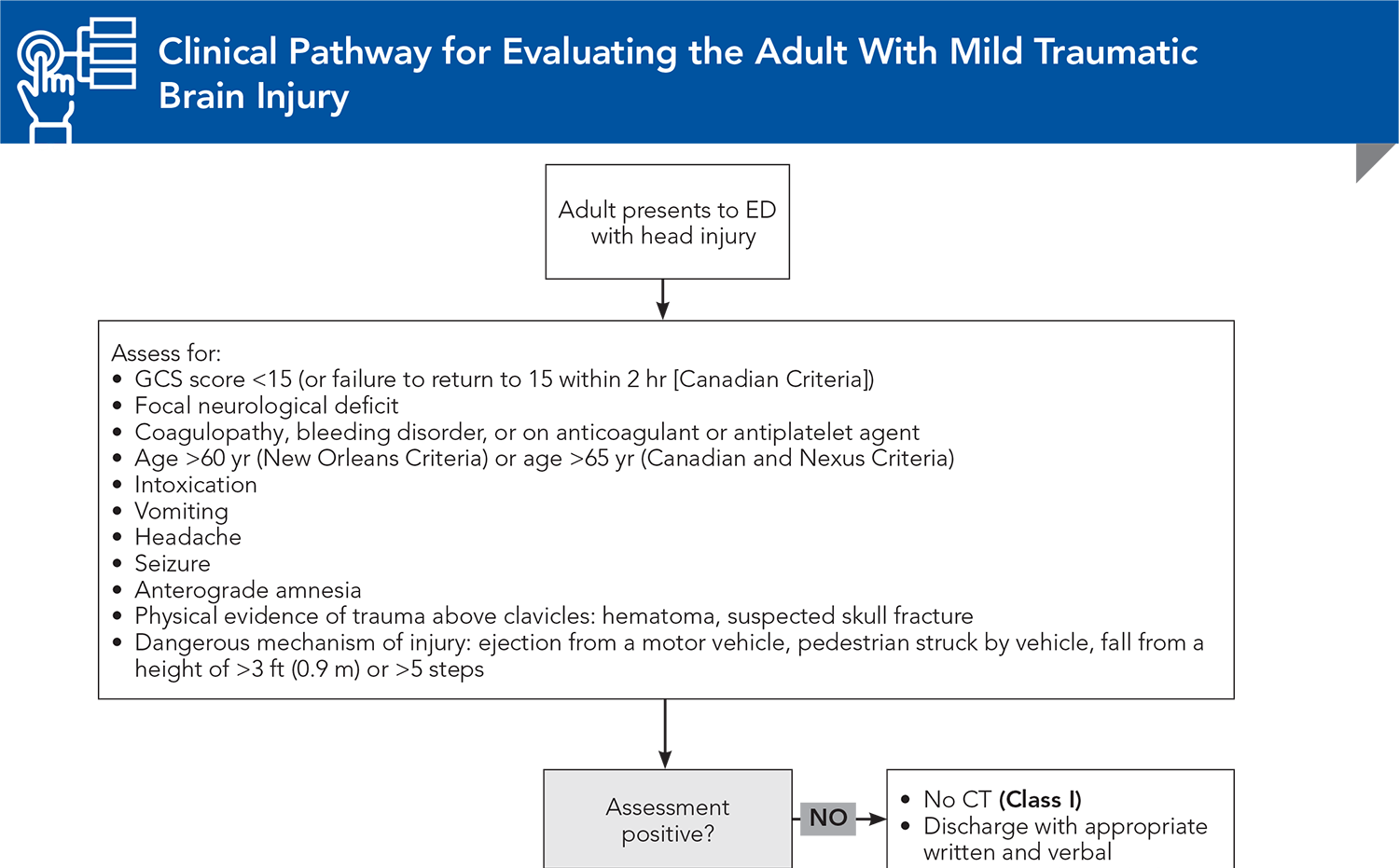
- Clinical Pathway for Evaluating the Adult With Mild Traumatic Brain Injury
- Clinical Pathway for Evaluating the Child With Mild Traumatic Brain Injury
- Tables and Figures
- References
Abstract
With almost 2.9 million people in the United States seeking medical attention for head trauma each year, emergency clinicians face the critical task of efficiently and accurately identifying patients with potentially life-threatening intracranial trauma. This issue of Emergency Medicine Practice: Trauma EXTRA! reviews clinical guidelines, discusses challenges in the care of patients at extremes of ages, and provides indications for imaging. Management and disposition of patients with mild traumatic brain injury that includes neurosurgery consultation, hospital admission for observation or repeat imaging, and discharge precautions are also reviewed.
Case Presentations
- The teen reports having several minutes of disorientation after the collision.
- He states that his only symptom now is a residual mild headache, but his coach recommended that his parents take him to the ER to be medically cleared before returning to play.
- You consider whether he needs a CT.
- She reports that she passed out and then had an episode of nausea.
- She is feeling fine now, but you wonder what the likelihood is that this patient will have clinically important injury on head CT.
- The parents explain that their babysitter reported that the baby accidentally rolled off the bed during a diaper change.
- The baby appears to be sleeping comfortably in her father’s arms, arousing appropriately, but you note a bruise on her left temple.
- You're reluctant to order a CT and question if she needs to be admitted. You also wonder if there might be more to the babysitter’s story.
- There was no loss of consciousness, but he does have a laceration on his chin.
- EMS personnel report that he is not on anticoagulants, although he does take aspirin and clopidogrel.
- They also note that his current state of “pleasantly confused” is consistent with his baseline mental status.
- You question whether you should order a CT and whether he will need admission or will it be safe to discharge him to the nursing home.
- He tells you that he was drinking alcohol earlier that evening and does not recall how he sustained the injury.
- His CT shows a small focal subarachnoid hemorrhage.
- You think he should be admitted, but the neurosurgeons in your hospital have been reluctant to admit and sometimes don’t even come in to see some patients with small intracranial injuries.
- You wonder if this patient can be discharged safely.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Managing Patients Presenting with Acute Diarrhea in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
12. * Kirelik SB. Concussion in the emergency department: a review of current guidelines. Emerg Med Pract. 2019;21(Suppl 9):1-29. (Guideline review)
13. * Pandor A, Goodacre S, Harnan S, et al. Diagnostic management strategies for adults and children with minor head injury: a systematic review and an economic evaluation. Health Technol Assess. 2011;15(27):1-202. (Systematic review; 93 patients) DOI: 10.3310/hta15270
36. * Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. (Prospective study; 42,412 patients) DOI: 10.1016/S0140-6736(09)61558-0
45. * Greenes DS, Schutzman SA. Clinical indicators of intracranial injury in head-injured infants. Pediatrics. 1999;104(4 Pt 1):861-867. (Prospective study; 608 patients) DOI: 10.1542/peds.104.4.861
53. * Nishijima DK, Offerman SR, Ballard DW, et al. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.e1-7. (Prospective study; 1064 patients) DOI: 10.1016/j.annemergmed.2012.04.007
94. * Atzema C, Mower WR, Hoffman JR, et al. Defining “clinically unimportant” CT findings in patients with blunt head trauma. Acad Emerg Med. 2002;9(5):451. (Secondary analysis; 8374 patients)
95. * Clement CM, Stiell IG, Schull MJ, et al. Clinical features of head injury patients presenting with a Glasgow Coma Scale score of 15 and who require neurosurgical intervention. Ann Emerg Med. 2006;48(3):245-251. (Secondary analysis; 4551 patients) DOI: 10.1016/j.annemergmed.2006.04.008
96. * Joseph B, Aziz H, Pandit V, et al. Prospective validation of the brain injury guidelines: managing traumatic brain injury without neurosurgical consultation. J Trauma Acute Care Surg. 2014;77(6):984-988. (Guidelines) DOI: 10.1097/TA.0000000000000428
165. * Hamilton M, Mrazik M, Johnson DW. Incidence of delayed intracranial hemorrhage in children after uncomplicated minor head injuries. Pediatrics. 2010;126(1):e33-e39. (Retrospective comparative study; 17,962 patients) DOI: 10.1542/peds.2009-0692
Subscribe to get the full list of 223 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: intracranial injury, concussion, mild traumatic brain injury, intracranial trauma, postconcussive syndrome, head injury, blunt head trauma, cerebral contusions, Glascow Coma Scale, headache, computed tomography, New Orleans Criteria, Canadian CT Head Rule, neurology, Brain Injury Guidelines, sports-related concussion