Table of Contents
About This Issue
An important aspect of the management of pediatric community-acquired pneumonia is identifying patients who are more likely to have bacterial pneumonia and will benefit from antibiotic therapy, while avoiding unnecessary testing and treatment in children who have viral pneumonia. Urgent care clinicians must also be able to recognize patients who require transfer to a higher level of care for assessment and treatment. In this course, you will learn:
Common viral and bacterial etiologies of community-acquired pneumonia
Key historical information and physical examination findings that can help differentiate viral and bacterial causes of pneumonia
When chest x-rays and/or laboratory tests are recommended
Which patients should receive antibiotics, and which should be discharged home with return precautions and appropriate follow-up
Recommendations for empiric antibiotic regimens
When asthma should be suspected in children who present with symptoms of pneumonia
The historical and clinical indications for referral or transfer to the emergency department
CODING & CHARTING: Learn how to select the appropriate level of service for the management of pediatric patients with community-acquired pneumonia in urgent care.
-
About This Issue
-
Abstract
-
Case Presentations
-
Introduction
-
Etiology
-
Differentiation of Viral Causes from Bacterial Causes
-
Viral Etiologies
-
Bacterial Etiologies
-
Streptococcus pneumoniae
-
Staphylococcus aureus and Streptococcus pyogenes
-
Mycoplasma pneumoniae
-
Less Common Bacterial Causes
-
Differential Diagnosis
-
Bronchiolitis
-
Recurrent Viral-Induced Wheeze and Asthma
-
Foreign-Body Aspiration
-
Other Alternative Diagnoses
-
Congenital Heart Disease
-
Metabolic Disorders
-
Urgent Care Evaluation
-
Initial Assessment
-
History
-
History of Present Illness
-
Past Medical History
-
Immunization Status
-
Family History
-
Vital Signs
-
Temperature
-
Respiratory Rate
-
Pulse Oximetry
-
Physical Examination
-
General Appearance
-
Pulmonary Examination
-
Cardiac Examination
-
Diagnostic Studies
-
Laboratory Studies
-
Complete Blood Count
-
Inflammatory Markers
-
Chemistries
-
Blood Culture
-
Other Microbiological Assays
-
Imaging
-
Chest X-Ray
-
Possible Indications for Chest X-Ray
-
Chest X-Ray Findings in Pneumonia
-
Patients With Asthma
-
Ultrasound
-
Treatment
-
Oxygen
-
Antipyretics
-
Intravenous Fluids
-
Albuterol and Corticosteroids
-
Antibiotics
-
Management of Parapneumonic Effusion and Empyema
-
Special Populations
-
Patients With Bronchopulmonary Dysplasia
-
Patients With Neuromuscular Disease
-
Patients Who Are Immunodeficient
-
Cutting Edge
-
Transcriptomics
-
Scoring Systems/Risk Models
-
Disposition
-
Time- and Cost-Effective Strategies
-
Summary
-
Risk Management Pitfalls in the Urgent Care Management of Pediatric Patients with Community-Acquired Pneumonia
-
Case Conclusions
-
Critical Appraisal of the Literature
-
Coding & Charting: What You Need to Know
-
Number and Complexity of Problems Addressed
-
Amount and/or Complexity of Data to be Reviewed and Analyzed
-
Risk of Complications and/or Morbidity or Mortality of Patient Management
-
Coding Challenge
-
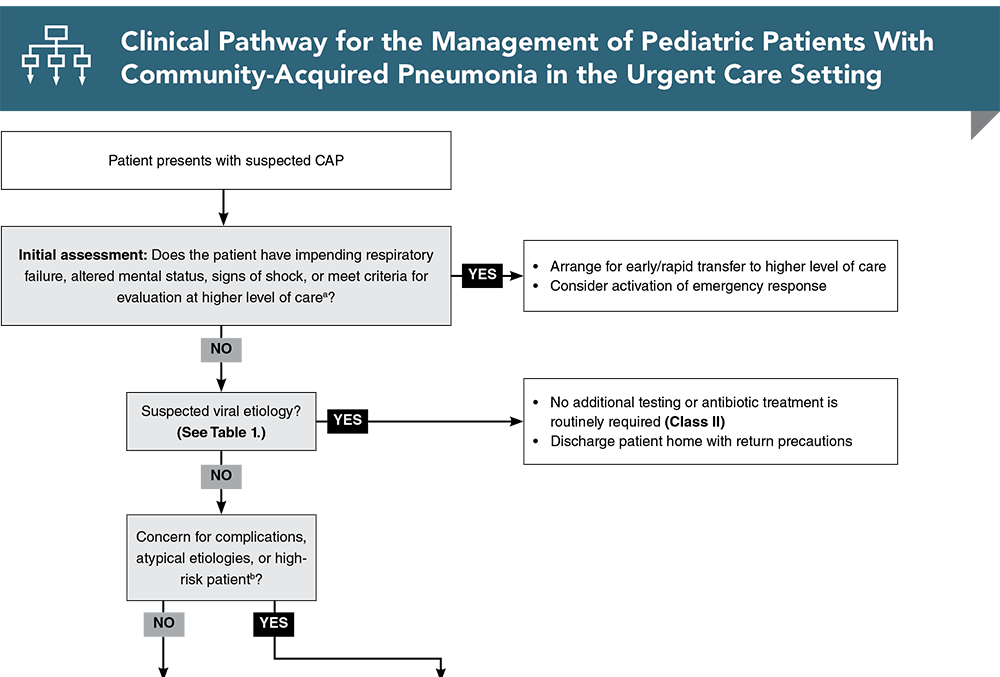
Clinical Pathway for the Management of Pediatric Patients With Community-Acquired Pneumonia in the Urgent Care Setting
-
References
-
Acknowledgments
Abstract
Distinguishing viral from bacterial causes of pneumonia in the urgent care setting is paramount to providing effective treatment but remains a significant challenge. For pediatric patients who can be managed with outpatient treatment, the utility of laboratory tests and radiographic studies, as well as the need for empiric antibiotics, remains questionable. This issue reviews viral and bacterial etiologies of community-acquired pneumonia in pediatric patients, offers guidance for obtaining historical information and interpreting physical examination findings, discusses the utility of various diagnostic techniques, and provides recommendations for the treatment of previously healthy and medically fragile children.
Case Presentations
-
The girl’s temperature is 39.4°C (103°F).
-
On examination, she is ill-appearing states that her belly hurts. Although she complains of severe abdominal pain, the pain cannot be localized to a specific quadrant.
-
There is no respiratory distress, and her lungs are clear to auscultation.
-
You recall that pneumonia can present as abdominal pain and wonder if that could be the case for this patient. Should you transfer the patient to a higher level of care for further evaluation or continue the evaluation in the urgent care?
-
She was started on amoxicillin-clavulanate 2 days prior but has not improved. On examination, she is alert, nontoxic, and not in respiratory distress.
-
Chest auscultation reveals decreased breath sounds and rales in the left lower lobe.
-
The high fever and localized chest findings prompt you to order a chest x-ray, which shows a large left-sided pleural effusion.
-
As you look at the film, you begin to wonder…what is the best next step in management for this patient?
-
His past medical history includes a prior hospitalization for pneumonia. His immunizations are up to date.
-
His temperature is 39.4°C (103°F). He appears nontoxic. He is in moderate respiratory distress with a pulse oximetry of 92% on ambient air, and his respiratory rate is 56 breaths/min.
-
Chest auscultation reveals bilateral wheezes and localized rales in the left lower lobe.
-
As you consider starting antibiotics and transferring the patient to a higher level of care, you wonder whether it is common for children to have repeat episodes of pneumonia. Are there are other questions on the review of systems that might be helpful in this patient?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for the Management of Pediatric Patients With Community-Acquired Pneumonia in the Urgent Care Setting
Subscribe to access the complete flowchart to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Kronman MP, Hersh AL, Feng R, et al. Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994-2007. Pediatrics. 2011;127(3):411-418. (Population-based surveillance) DOI: 10.1542/peds.2010-2008
5. * Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372(9):835-845. (Prospective study; 2358 patients) DOI: 10.1056/NEJMoa1405870
10. * Korppi M, Don M, Valent F, et al. The value of clinical features in differentiating between viral, pneumococcal and atypical bacterial pneumonia in children. Acta Paediatr. 2008;97(7):943-947. (Case-control study; 101 patients) DOI: 10.1111/j.1651-2227.2008.00789.x
23. * Li ST, Tancredi DJ. Empyema hospitalizations increased in US children despite pneumococcal conjugate vaccine. Pediatrics. 2010;125(1):26-33. (Retrospective study; 2898 patients) DOI: 10.1542/peds.2009-0184
44. National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute (US); 2007. Accessed December 10, 2023. (Guidelines)
49. * Shah SN, Bachur RG, Simel DL, et al. Does this child have pneumonia?: The rational clinical examination systematic review. JAMA. 2017;318(5):462-471. (Systematic review; 23 prospective cohort studies, 13,833 children) DOI: 10.1001/jama.2017.9039
54. * Bachur R, Perry H, Harper MB. Occult pneumonias: empiric chest radiographs in febrile children with leukocytosis. Ann Emerg Med. 1999;33(2):166-173. (Prospective cohort study; 278 patients) DOI: 10.1016/s0196-0644(99)70390-2
55. * Mathews B, Shah S, Cleveland RH, et al. Clinical predictors of pneumonia among children with wheezing. Pediatrics. 2009;124(1):e29-e36. (Prospective cohort study; 526 subjects) DOI: 10.1542/peds.2008-2062
73. * St Peter SD, Tsao K, Spilde TL, et al. Thoracoscopic decortication vs tube thoracostomy with fibrinolysis for empyema in children: a prospective, randomized trial. J Pediatr Surg. 2009;44(1):106-111. (Randomized controlled trial; 36 patients) DOI: 10.1016/j.jpedsurg.2008.10.018
123. *Bielicki JA, Stohr W, Barratt S, et al. Effect of amoxicillin dose and treatment duration on the need for antibiotic re-treatment in children with community-acquired pneumonia: the CAP-IT randomized clinical trial. JAMA. 2021;326(17):1713-1724. (Multicenter, randomized controlled trial; 824 patients) DOI: 10.1001/jama.2021.17843
Acknowledgments
Portions of this content were adapted from: Cooper-Sood J, Wallihan R, Naprawa J. Pediatric community-acquired pneumonia: diagnosis and management in the emergency department. Pediatr Emerg Med Pract. 2019;16(4):1-28 Used with permission of EB Medicine.
Subscribe to get the full list of 139 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: pediatric pneumonia, community-acquired pneumonia, CAP, pediatric CAP, viral pneumonia, bacterial pneumonia, mycoplasma pneumoniae, CXR, asthma, antibiotic, COVID, influenza, pleural effusion