Table of Contents
About This Issue
While prolonged pediatric fever is most often due to a self-limiting infectious illness, it can sometimes be a sign of much more serious illness. The care of children with prolonged fever can be challenging because the definition of when a fever becomes “prolonged” is not well defined, and evidence-based decision support tools are limited. This issue constructs a framework for initial emergency department evaluation and management of children with fever lasting ≥5 days and fever of unknown origin lasting ≥8 days. In this issue, you will learn:
Relevant definitions of fever
Possible conditions in the differential diagnosis of pediatric prolonged fever without an obvious source
Criteria for Kawasaki disease and incomplete Kawasaki disease
Specific risk factors for certain causes of prolonged fever
Key components of the physical examination, and diagnoses to consider from physical examination findings in children with prolonged fever
Which laboratory studies to order to evaluate for Kawaski disease
When studies such as urinalysis and/or urine culture or viral panel testing are indicated
Which laboratory studies are recommended for children with fever lasting ≥8 days
Additional tests that are recommended only in specific circumstances
Uses and precautions for procalcitonin testing
Imaging studies that can be used to evaluate for focal sources of infection or other pathology
General treatment principles for prolonged fever in children, by suspected or identified cause of fever
Recommendations for which patients need to be admitted, and which can be discharged with follow up with their primary care clinician or an appropriate specialist if fever continues
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
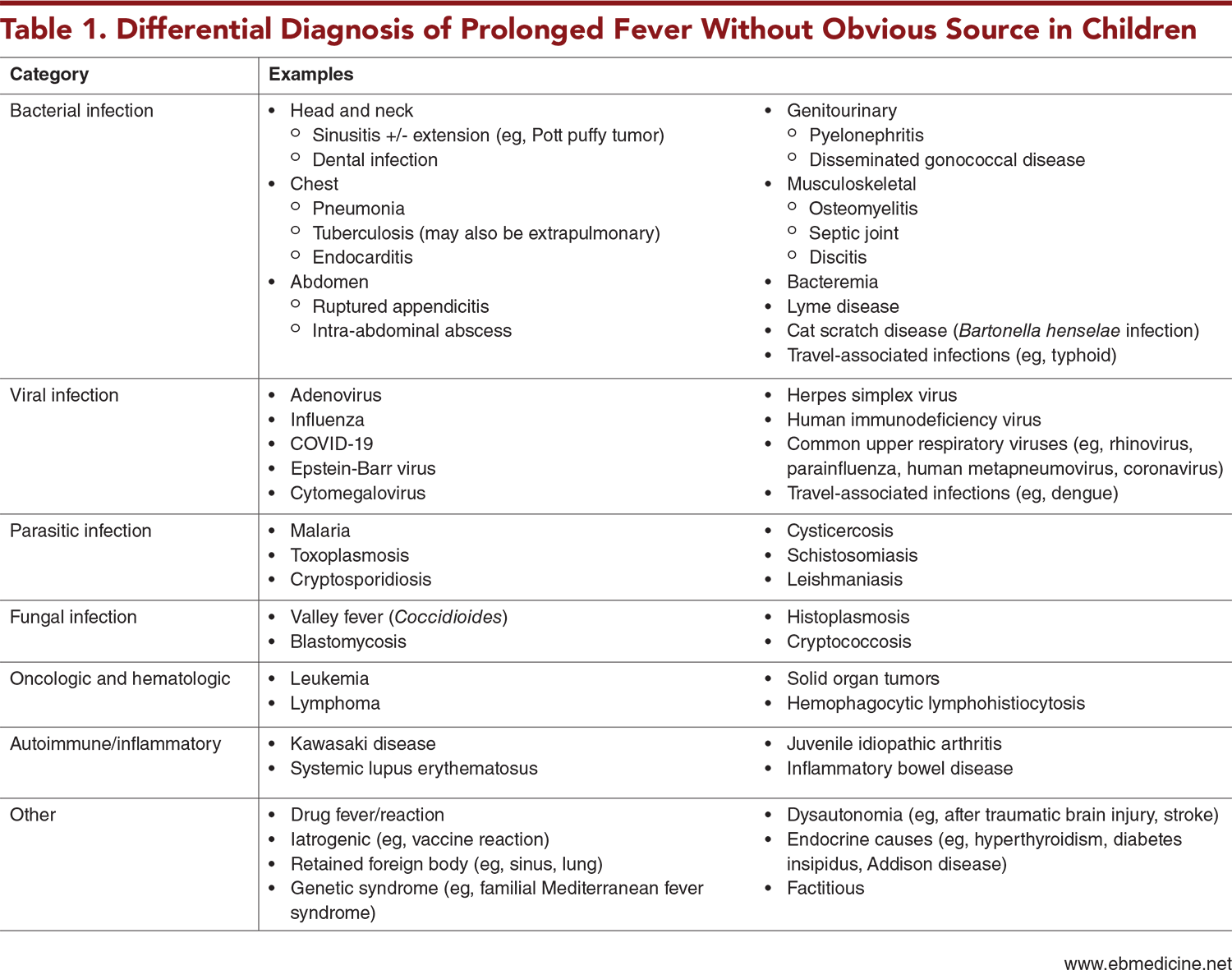
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- Initial Evaluation
- History
- Criteria for Kawasaki Disease
- Specific Risk Factors
- Physical Examination
- Head, Ears, Eyes, Nose, and Throat Examination
- Chest Examination
- Abdominal Examination
- Musculoskeletal Examination
- Skin Examination
- Genitourinary Examination
- Neurologic Examination
- Diagnostic Studies
- Laboratory Studies
- Fever of at Least 38°C for 5 Days or More
- Fever of at Least 38°C for 8 Days or More Without a Clear Source
- Risk-Factor–Based Testing
- Testing Recommended for Specific Circumstances
- Imaging Studies
- X-Ray
- Ultrasound
- Computed Tomography and Magnetic Resonance Imaging
- Electroencephalogram
- Electrocardiogram
- Treatment
- Special Populations
- Controversies and Cutting Edge
- Whole-Body Imaging
- Positron Emission Tomography/Computed Tomography
- Magnetic Resonance Imaging
- Biomarkers
- Diagnostic Pathogen Panels
- Disposition
- Summary
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Management of Pediatric Patients With Prolonged Fever
- Case Conclusions
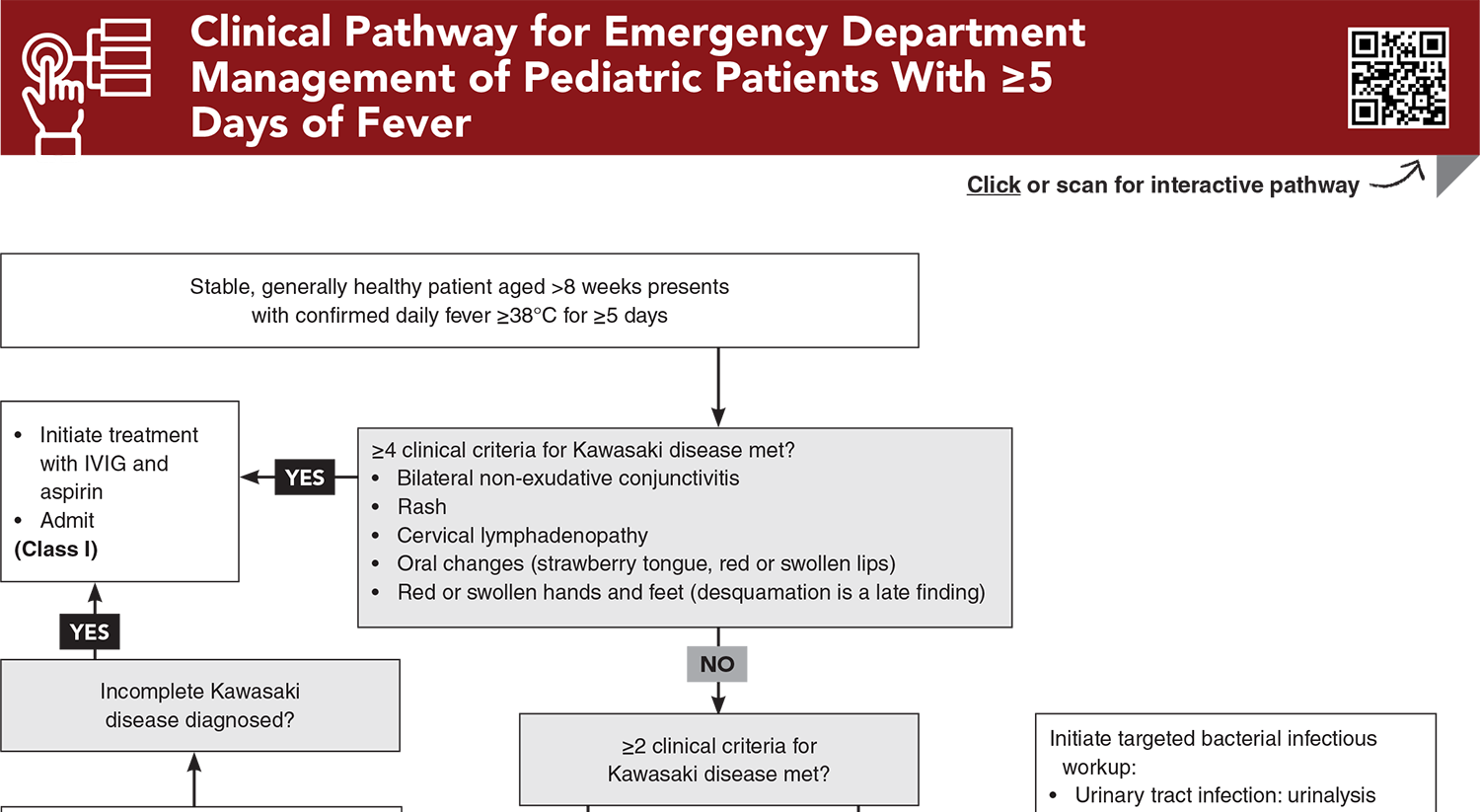
- Clinical Pathways
- Clinical Pathway for Emergency Department Management of Pediatric Patients With ≥5 Days of Fever
- Clinical Pathway for Emergency Department Management of Pediatric Patients With ≥8 Days of Fever
- Tables
- References
Abstract
Prolonged pediatric fever is most often due to a self-limiting infectious illness, but can sometimes be a sign of much more serious disease. The care of children with prolonged fever can be challenging, since there is significant variation in the definition of prolonged pediatric fever, and evidence-based decision support tools to guide evaluation and management of children with prolonged fever are limited. This issue constructs a framework for initial emergency department evaluation and management of children with fever lasting ≥5 days and fever of unknown origin lasting ≥8 days.
Case Presentations
- The child’s parents tell you he has been sick with cough, congestion, and rhinorrhea for at least 2 weeks, and he has had tactile fevers “every night.”
- He is fully vaccinated, well hydrated, and playful in the examination room, with clear nasal rhinorrhea and an occasional cough.
- Your leading diagnosis is viral illness, but you wonder whether you should investigate further, due to the family’s report of fever for 2 weeks...
- Her mother says she has had daily fevers to a maximum temperature of 103.8°F, with low energy, red eyes without discharge, and a rash of small red bumps on her chest and back.
- The family thought it was “just a cold” and have been treating her with antipyretics, rest, and fluids, but tell you her symptoms are not getting better.
- You consider that this could still be a viral infection, but also wonder whether you should investigate for bacterial infection or other conditions, since the girl has had a fever for more than 5 days...
- The boy’s parents report that he has had fever to at least 101°F each day for 10 days and that he seems less active than usual, with poor appetite and not wanting to run and play as he normally does. The boy‘s parents say he speaks only a few words and does not often express pain, so they have a hard time knowing whether anything specific has been bothering him.
- The boy is febrile and tired-appearing, with a nonfocal examination.
- You consider what further workup you should pursue or if he needs further monitoring, given his difficulty communicating and his inability to clearly indicate pain.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Pediatric Patients With ≥5 Days of Fever
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables
Subscribe for full access to all Tables.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
3. * Leazer RC. Evaluation and management of young febrile infants: an overview of the new AAP guideline. Pediatr Rev. 2023;44(3):127-138. (Review) DOI: 10.1542/pir.2022-005624
8. * Antoon JW, Potisek NM, Lohr JA. Pediatric fever of unknown origin. Pediatr Rev. 2015;36(9):380-391. (Review) DOI: 10.1542/pir.36-9-380
21. * Trapani S, Fiordelisi A, Stinco M, et al. Update on fever of unknown origin in children: focus on etiologies and clinical approach. Children. 2024;11(1):20. (Review) DOI: 10.3390/children11010020
22. * McCrindle BW, Rowley AH, Jane WN, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927-e999. (Scientific statement) DOI: 10.1161/CIR.0000000000000484
31. * Jone P-N, Tremoulet A, Choueiter N, et al. Update on diagnosis and management of Kawasaki disease: a scientific statement from the American Heart Association. Circulation. 2024;150(23):e481-e500. (Scientific statement) DOI: 10.1161/CIR.0000000000001295
Subscribe to get the full list of 79 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: fever, prolonged fever, fever without a source, fever of unknown origin, FUO, pseudo-FUO, tactile fever, subjective fever, infectious illness, bacterial infection, viral infection, parasitic infection, fungal infection, autoimmune, inflammatory, Kawasaki disease, incomplete Kawaski disease, drug reaction, drug fever, malignancy, endocrine, neurologic, genetic, procalcitonin, whole-body imaging, biomarkers