

plications
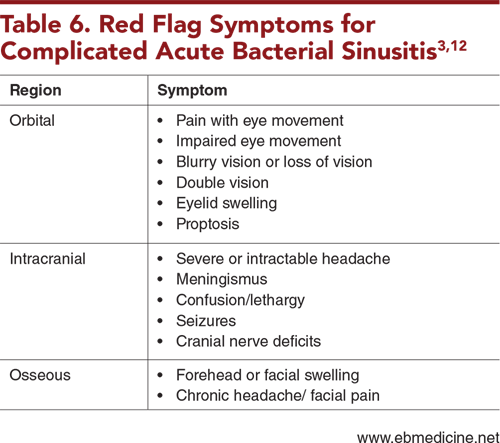
Upper respiratory infections are some of the most common reasons for pediatric patients to present to the emergency department. A small percentage of these viral infections can evolve into acute bacterial sinusitis (ABS), which can be further complicated by the development of orbital, intracranial, and osseous complications. Differentiating between viral upper respiratory infections and ABS and identifying cases of ABS that require antibiotics can pose a challenge. This issue highlights the patterns of illness that are most consistent with ABS, based on the most current clinical practice guidelines. Additionally, this issue reviews clinical features that should raise suspicion for complicated disease and provides associated diagnostic and management pearls.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
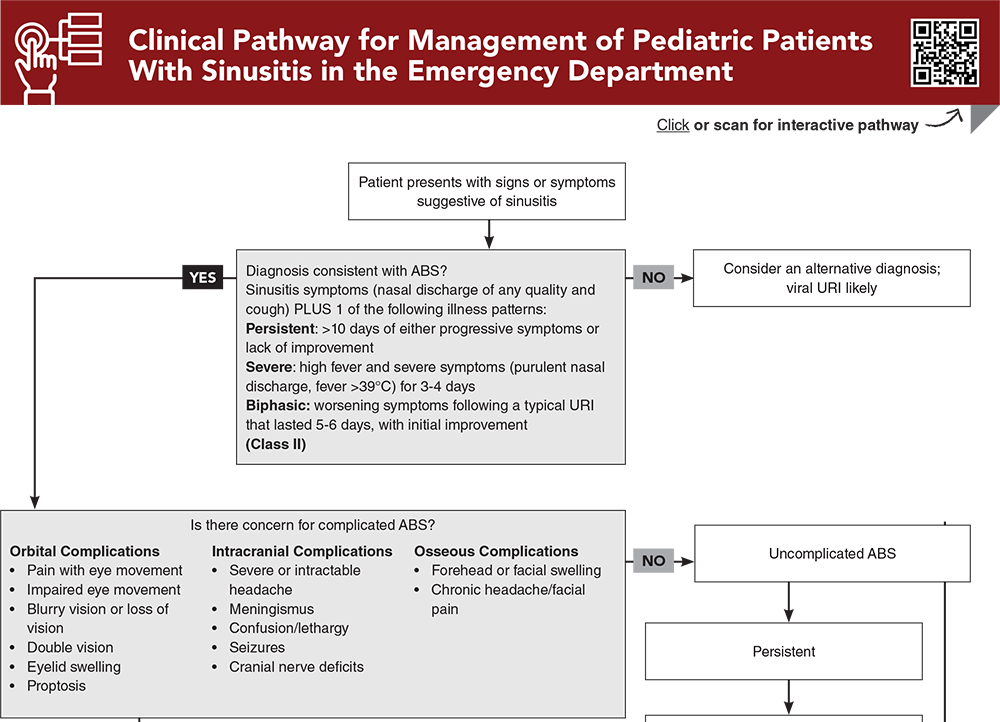
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
4. * Wald ER, Applegate KE, Bordley C, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262-e280. (AAP clinical practice guideline) DOI: 10.1542/peds.2013-1071
5. * Chow AW, Benninger MS, Brook I, et al. Executive summary: IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):1041-1045. (IDSA clinical practice guideline) DOI: 10.1093/cid/cir1043
29. * Sawada S, Matsubara S. Microbiology of acute maxillary sinusitis in children. Laryngoscope. 2021;131(10):E2705-E2711. (Prospective; 31 patients) DOI: 10.1002/lary.29564
46. * Tekes A, Palasis S, Durand DJ, et al. ACR Appropriateness Criteria® sinusitis-child. J Am Coll Radiol. 2018;15(11):S403-S412. (ACR clinical practice guideline) DOI: 10.1016/j.jacr.2018.09.029
66. * Savage TJ, Kronman MP, Sreedhara SK, et al. Treatment failure and adverse events after amoxicillin-clavulanate vs amoxicillin for pediatric acute sinusitis. JAMA. 2023;330(11):1064-1073. (Retrospective cohort; 198,942 patients) DOI: 10.1001/jama.2023.15503
69. * Garcia GH, Harris GJ. Criteria for nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988-1998. Ophthalmology. 2000;107(8):1454-1456. (Prospective; 40 patients) DOI: 10.1016/s0161-6420(00)00242-6
76. * Saposnik G, Bushnell C, Coutinho JM, et al. Diagnosis and management of cerebral venous thrombosis: a scientific statement from the American Heart Association. Stroke. 2024;55(3):e77-e90. (AHA clinical practice guideline) DOI: 10.1161/str.0000000000000456
Subscribe to get the full list of 78 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: pediatric sinusitis, bacterial sinusitis, viral sinusitis, allergic sinusitis, fungal sinusitis, sinusitis complications, sinusitis treatment, cerebral sinus thrombosis, anticoagulation, rhinosinusitis, pansinusitis, upper respiratory infection, sinus development, sinus anatomy, Chandler classification system, orbital cellulitis, forehead swelling, periorbital swelling, pediatric facial swelling, osteolysis, osteomyelitis, cerebral vein thrombosis, subperiosteal abscess, runny nose, nasal congestion, pediatric nasal discharge, Pott puffy tumor
Jaryd Zummer, MD; Alexis Luedke, MD
Sabah Fatima Iqbal, MD; Jennifer E. Sanders, MD, FAAP, FACEP
August 1, 2024
August 1, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 ACEP Category I Credits, 4 AAP Prescribed Credits, 4 AOA Category 2-B Credits.