

Traumatic wounds and lacerations are common pediatric presenting complaints to emergency departments. Although there is a large body of literature on wound care, many emergency clinicians base management of wounds on theories and techniques that have been passed down over time. Therefore, controversial, conflicting, and unfounded recommendations are prevalent. This issue reviews evidence-based recommendations for wound care, including wound cleansing and irrigation, anxiolysis/sedation techniques, closure methods, and postrepair wound care.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
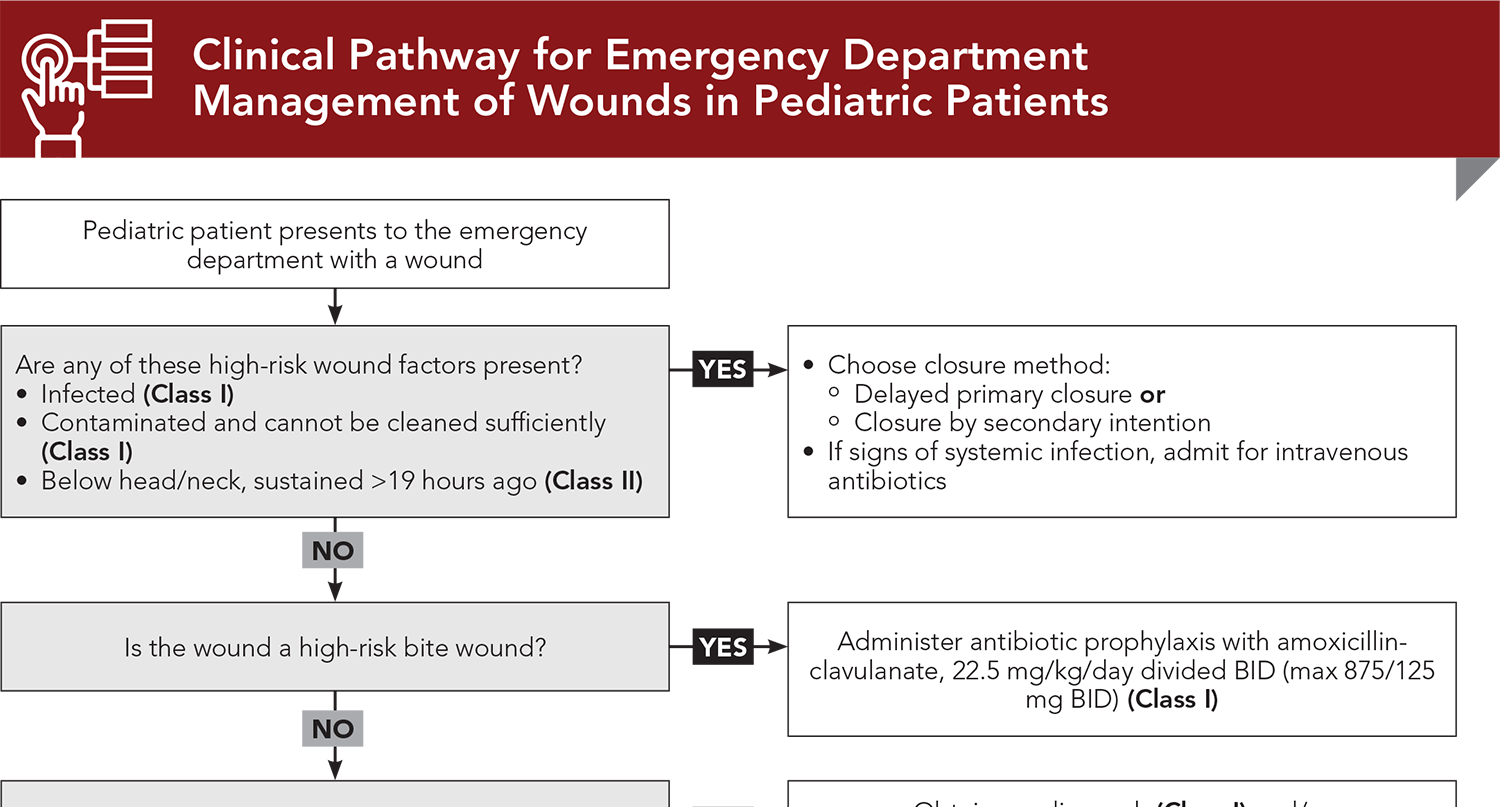
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
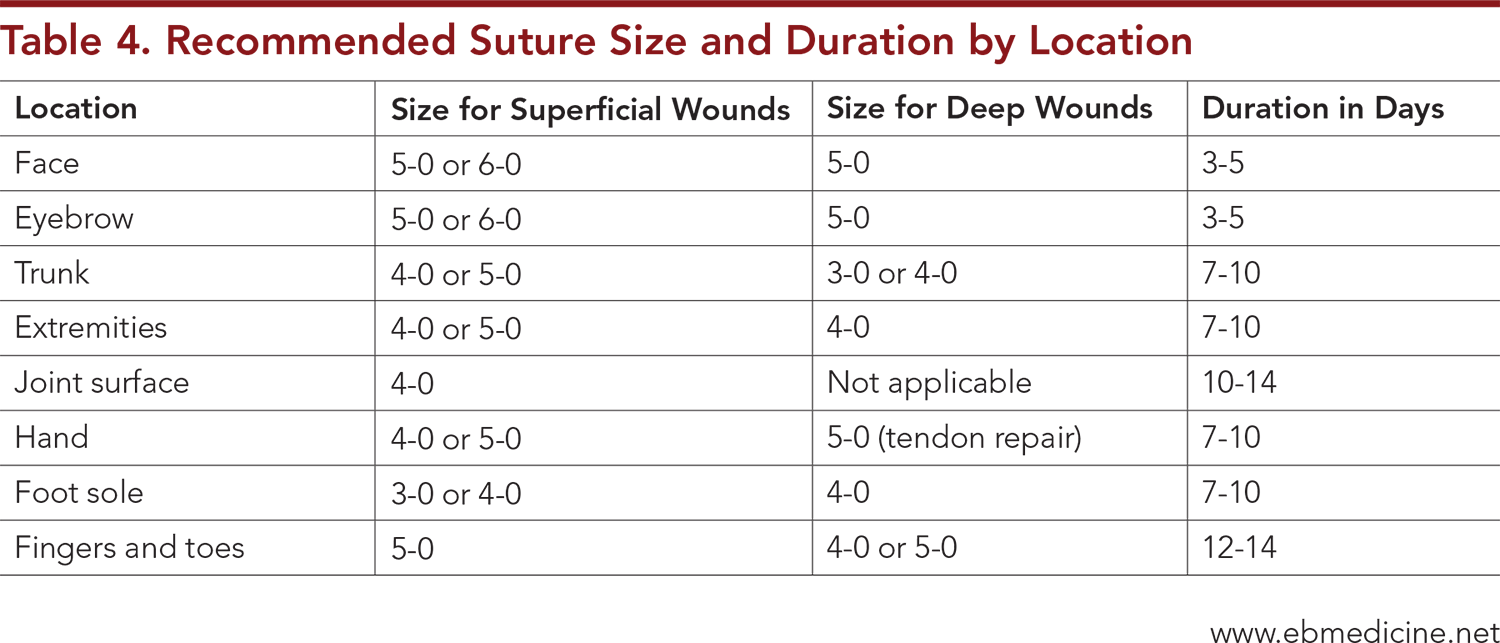
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
6. * Berk WA, Osbourne DD, Taylor DD. Evaluation of the ‘golden period’ for wound repair: 204 cases from a Third World emergency department. Ann Emerg Med. 1988;17(5):496-500. (Prospective study; 372 patients) DOI: 10.1016/s0196-0644(88)80246-4
20. * Fernandez R, Green HL, Griffiths R, et al. Water for wound cleansing. Cochrane Database Syst Rev. 2022;9(9):CD003861. (Systematic review; 13 studies) DOI: 10.1002/14651858.CD003861.pub3
47. * Eidelman A, Weiss JM, Baldwin CL, et al. Topical anaesthetics for repair of dermal laceration. Cochrane Database Syst Rev. 2011(6):CD005364. (Meta-analysis; 23 trials) DOI: 10.1002/14651858.CD005364.pub2
61. * Hogan ME, vanderVaart S, Perampaladas K, et al. Systematic review and meta-analysis of the effect of warming local anesthetics on injection pain. Ann Emerg Med. 2011;58(1):86-98.e81. (Meta-analysis; 18 studies) DOI: 10.1016/j.annemergmed.2010.12.001
65. * Birnie KA, Noel M, Chambers CT, et al. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2018; 10(10):CD005179. (Meta-analysis; 59 trials) DOI: 10.1002/14651858.CD005179.pub4
82. * Xu B, Xu B, Wang L, et al. Absorbable versus nonabsorbable sutures for skin closure: a meta-analysis of randomized controlled trials. Ann Plast Surg. 2016;76(5):598-606. (Meta-analysis; 19 trials) DOI: 10.1097/SAP.0000000000000418
83. * Luck R, Tredway T, Gerard J, et al. Comparison of cosmetic outcomes of absorbable versus nonabsorbable sutures in pediatric facial lacerations. Pediatr Emerg Care. 2013;29(6):691-695. (Randomized controlled trial; 89 patients)
99. * Farion KJ, Osmond MH, Hartling L, et al. Tissue adhesives for traumatic lacerations: a systematic review of randomized controlled trials. Acad Emerg Med. 2003;10(2):110-118. (Review) DOI: 10.1111/j.1553-2712.2003.tb00027.x
101. * Karounis H, Gouin S, Eisman H, et al. A randomized, controlled trial comparing long-term cosmetic outcomes of traumatic pediatric lacerations repaired with absorbable plain gut versus nonabsorbable nylon sutures. Acad Emerg Med. 2004;11(7):730-735. (Randomized controlled trial; 95 patients) DOI: 10.1197/j.aem.2003.12.029
112. * Andreana L, Isgro G, Metaxa V. Wound care of pretibial thin-skin lacerations with the combined use of sterile adhesive strips and sutures. J Emerg Med. 2015;49(3):345-346. (Techniques and procedures report) DOI: 10.1016/j.jemermed.2013.08.155
121. * Cummings P, Del Beccaro MA. Antibiotics to prevent infection of simple wounds: a meta-analysis of randomized studies. Am J Emerg Med. 1995;13(4):396-400. (Meta-analysis; 7 trials) DOI: 10.1016/0735-6757(95)90122-1
122. * Zehtabchi S. Evidence-based emergency medicine/critically appraised topic. The role of antibiotic prophylaxis for prevention of infection in patients with simple hand lacerations. Ann Emerg Med. 2007;49(5):682-689. (Meta-analysis; 4 trials) DOI: 10.1016/j.annemergmed.2006.12.014
126. * Edlich RF, Kenney JG, Morgan RF, et al. Antimicrobial treatment of minor soft tissue lacerations: a critical review. Emerg Med Clin North Am. 1986;4(3):561-580. (Review) DOI: 10.1016/S0733-8627(20)31023-3
130. * Dire DJ, Coppola M, Dwyer DA, et al. Prospective evaluation of topical antibiotics for preventing infections in uncomplicated soft-tissue wounds repaired in the ED. Acad Emerg Med. 1995;2(1):4-10. (Randomized controlled trial; 465 patients) DOI: 10.1111/j.1553-2712.1995.tb03070.x
140. * Toon CD, Sinha S, Davidson BR, et al. Early versus delayed post-operative bathing or showering to prevent wound complications. Cochrane Database Syst Rev. 2015(7):CD010075. (Meta-analysis; 1 trial) DOI: 10.1002/14651858.CD010075.pub3
150. * Cheng HT, Hsu YC, Wu CI. Does primary closure for dog bite wounds increase the incidence of wound infection? A meta-analysis of randomized controlled trials. J Plast Reconstr Aesthet Surg. 2014. (Meta-analysis) DOI: 10.1016/j.bjps.2014.05.051
151. * Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis. 2014;59(2):147-159. (Practice guideline) DOI: 10.1093/cid/ciu296
170. * Moscati RM, Mayrose J, Reardon RF, et al. A multicenter comparison of tap water versus sterile saline for wound irrigation. Acad Emerg Med. 2007;14(5):404-409. (Randomized controlled trial; 715 patients) PMID: 17456554
Subscribe to get the full list of 170 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: wounds, skin injuries, wound care, laceration, animal bite, human bite, tissue adhesive, postrepair wound care, epithelialization, primary closure, healing by primary intention, secondary closure, healing by secondary intention, delayed primary closure, healing by tertiary intention, “golden period”, wound preparation, irrigation, antisepsis, intradermal anesthetics, topical anesthesia, nerve blocks, child life specialist, anxiolysis, procedural sedation, sutures, staples, adhesive strips, hair apposition, simple interrupted suture, deep dermal suture, running suture, locked running suture, running subcuticular suture, mattress suture, vertical mattress suture, horizontal mattress suture, corner stitch, eversion, antibiotic prophylaxis, bite wounds, fight bite
Svetlana Duvidovich, DO; Jennifer E. Sanders, MD, FAAP, FACEP
Maria M. LoTempio, MD, FACS
April 15, 2025
April 15, 2028 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Trauma credits, subject to your state and institutional approval.