

More than 1.7 million traumatic brain injuries occur in adults and children each year in the United States, with approximately 30% occurring in children aged <14 years. Traumatic brain injury is a significant cause of morbidity and mortality in pediatric trauma patients. The early management of severe traumatic brain injury is focused on mitigation and prevention of secondary injury, specifically by avoiding hypotension and hypoxia, which have been associated with poorer outcomes. This review discusses methods to maintain adequate oxygenation, maximize management of intracranial hypertension, and optimize blood pressure in the emergency department to improve neurologic outcomes following pediatric severe traumatic brain injury.
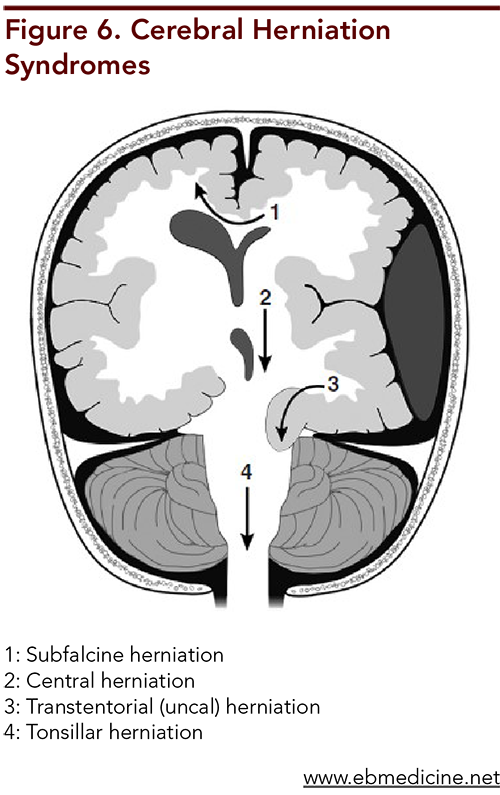
The mother, who is 22 years old and has 2 other children, is vague in her description of the child’s symptoms. The nurse calls you into triage because she notes the child appears unresponsive. The mother denies any trauma. The infant’s vital signs are as follows: afebrile; heart rate, 160 beats/min; blood pressure, 70/40 mm Hg; respiratory rate, 30 breaths/min; and oxygen saturation, 93% on room air. You struggle to calculate a GCS score, as this patient is not yet verbal. On physical examination, the child is minimally responsive and has irregular and shallow respiration, so you prepare to intubate. During placement of an IV line, the child flexes his left arm in response to pain, but no spontaneous movement of the right arm or leg is noted. During the secondary survey, you note a bulging fontanelle and a dilated left pupil, with deviation of the left eye both downward and peripherally. You have the clerk page neurosurgery emergently. The respiratory therapist asks you if you would like to hyperventilate the patient.
What should your target PaCO2 level be? What medication(s) should be given immediately? Once stabilized, are there any other services or specialists that should be involved with this patient, based on the history?
When the patient arrives, you quickly calculate a GCS score of 7 (E1, M4, V2), and you page the trauma surgery team to the ED. The patient's vital signs are as follows: afebrile; heart rate, 115 beats/min; blood pressure, 110/60 mm Hg; respiratory rate, 10 breaths/min; and oxygen saturation, 90% on room air. She has obvious right-sided head trauma and is in cervical spine immobilization. You immediately place a nonrebreather mask on the patient and call for rapid sequence intubation medications and equipment. You intubate the patient while maintaining cervical spine precautions. The neurosurgeon calls you back and states that he is on his way to the hospital.
What initial steps should be taken to stabilize this patient? How will you determine the disposition for this patient?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
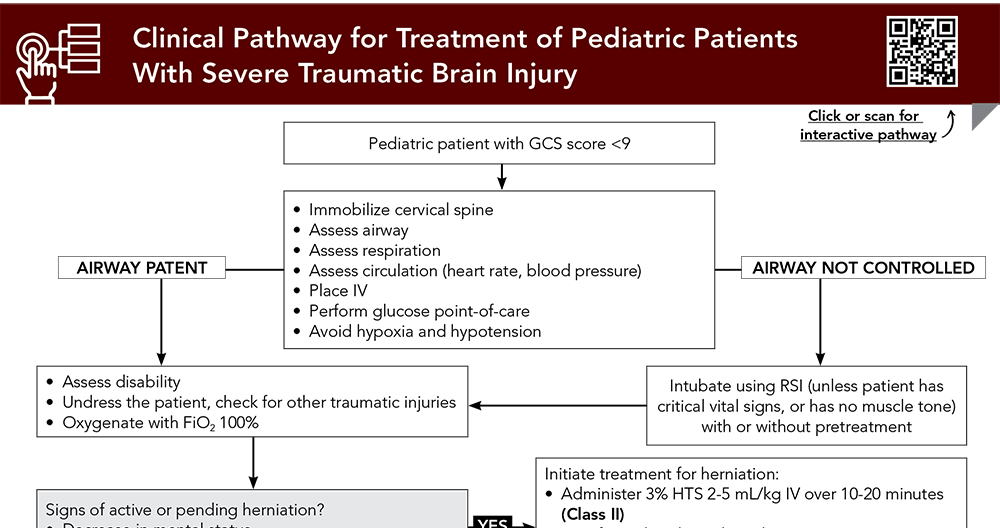
Subscribe to access the complete flowchart to guide your clinical decision making.
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
11. * Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the Brain Trauma Foundation Guidelines, executive summary. Neurosurgery. 2019;84(6):1169-1178. (Guidelines) DOI: 10.1093/neuros/nyz051
12. * Kochanek PM, Tasker RC, Bell MJ, et al. Management of pediatric severe traumatic brain injury: 2019 consensus and guidelines-based algorithm for first and second tier therapies. Pediatr Crit Care Med. 2019;20(3):269-279. (Treatment algorithm) DOI: 10.1097/PCC.0000000000001737
13. * American College of Surgeons. Chapter 10 - Pediatric Trauma. Advanced Trauma Life Support Student Course Manual. 10th ed. American College of Surgeons; 2018. (Course manual chapter)
27. * Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24 Suppl 1:S1-S106. (Practice guidelines) DOI: 10.1089/neu.2007.9999
28. * Kochanek PM, Tasker RC, Carney N, et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: update of the Brain Trauma Foundation Guidelines. Pediatr Crit Care Med. 2019;20(3S Suppl 1):S1-S82. (Guidelines) DOI: 10.1097/PCC.0000000000001735
97. * Kochanek PM, Adelson PD, Rosario BL, et al. Comparison of intracranial pressure measurements before and after hypertonic saline or mannitol treatment in children with severe traumatic brain injury. JAMA Netw Open. 2022;5(3):e220891. (Comparative effectiveness study; 518 patients) DOI: 10.1001/jamanetworkopen.2022.0891
107. * Kolias AG, Adams H, Timofeev IS, et al. Evaluation of outcomes among patients with traumatic intracranial hypertension treated with decompressive craniectomy vs standard medical care at 24 months: a secondary analysis of the RESCUEicp randomized clinical trial. JAMA Neurol. 2022;79(7):664-671. (Randomized controlled trial; 408 patients aged 10 years to adult) DOI: 10.1001/jamaneurol.2022.1070
126. * Pierce MC, Kaczor K, Lorenz DJ, et al. Validation of a clinical decision rule to predict abuse in young children based on bruising characteristics. JAMA Netw Open. 2021;4(4):e215832. (Prospective trial; 2161 patients) DOI: 10.1001/jamanetworkopen.2021.5832
143. * Utsumi S, Amagasa S, Yasuda H, et al. Targeted temperature management in pediatric traumatic brain injury: a systematic review and network meta-analysis. World Neurosurg. 2023;173:158-166. (Met-analysis; 6 trials, 448 patients) DOI: 10.1016/j.wneu.2023.01.056
144. * Adelson PD, Ragheb J, Kanev P, et al. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery. 2005;56(4):740-754. (Prospective, phase II randomized controlled trial; 48 patients)
147. * Hutchison JS, Ward RE, Lacroix J, et al. Hypothermia therapy after traumatic brain injury in children. N Engl J Med. 2008;358(23):2447-2456. (Prospective, randomized controlled trial; 225 patients) DOI: 10.1056/NEJMoa0706930
Subscribe to get the full list of 171 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: TBI, severe traumatic brain injury, severe TBI, subdural hematoma, epidural hematoma, subarachnoid hemorrhage, cerebral contusion, diffuse axonal injury, intraventricular hemorrhage, intracranial pressure, ICP, subfalcine herniation, central herniation, transtentorial herniation, tonsillar herniation, nonaccidental trauma, shaken baby syndrome, abusive head trauma
Hilary Fairbrother, MD, MPH, FACEP; Kirsten Morrissey, MD, FAAP
Genevieve Santillanes, MD, FACEP, FAAP
June 15, 2024
June 15, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Trauma CME credits, subject to your state and institutional approval.