

Over 40% of children will experience dental trauma by the age of 4 years. Timely and effective care is important in the management of dental injuries, as several studies have shown poor outcomes with delayed treatment. The current evidence in the management of dental injuries is primarily from a dentist’s perspective, with limited evidence specific to management in the emergency department. The goal of pediatric dental injury management is dictated largely by whether the dentition is primary or permanent. This issue provides a systematic emergency medicine-based approach to address pediatric dental injuries, along with a review of basic dental procedures that will lead to improved dental outcomes.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
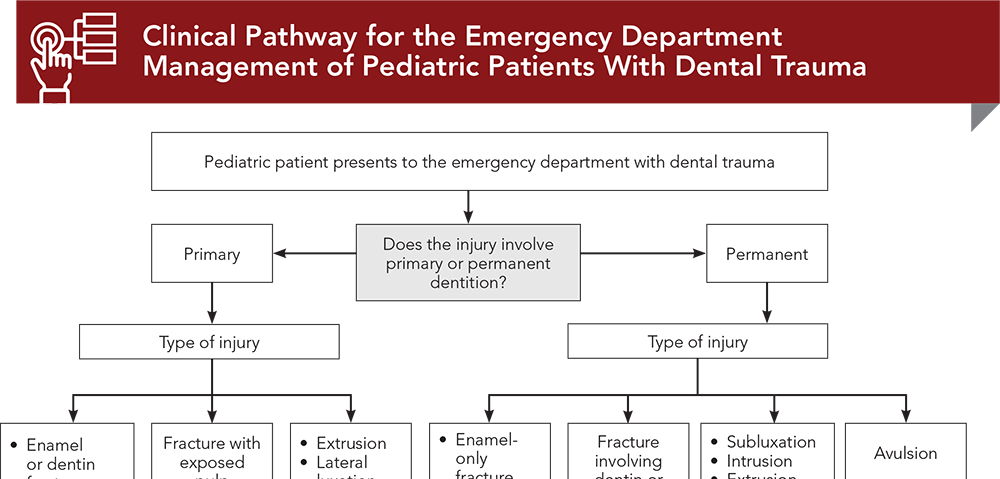
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
7. * Flores MT. Traumatic injuries in the primary dentition. Dent Traumatol. 2002;18(6):287-298. (Systematic review; 75 studies) DOI: 10.1034/j.1600-9657.2002.00153.x
12. * Mitchell J, Sheller B, Velan E, et al. Managing pediatric dental trauma in a hospital emergency department. Pediatr Dent. 2014;36(3):205-210. (Retrospective chart review; 265 patients) PMID: 24960386
28. * American Dental Association. Baby Teeth Eruption Chart. Accessed December 1, 2024. (Review)
31. * Day PF, Flores MT, O’Connell AC, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent Traumatol. 2020;36(4):343-359. (Guideline) DOI: 10.1111/edt.12576
32. * Bourguignon C, Cohenca N, Lauridsen E, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent Traumatol. 2020;36(4):314-330. (Guideline) DOI: 10.1111/edt.12576
38. * Fouad AF, Abbott PV, Tsilingaridis G, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2020;36(4):331-342. (Guideline) DOI: 10.1111/edt.12573
59. * Caputo ND, Raja A, Shields C, et al. Re-evaluating the diagnostic accuracy of the tongue blade test: still useful as a screening tool for mandibular fractures? J Emerg Med. 2013;45(1):8-12. (Controlled clinical trial; 190 patients) DOI: 10.1016/j.jemermed.2012.11.078
64. * da Fonseca MA, Feigal RJ, ten Bensel RW. Dental aspects of 1248 cases of child maltreatment on file at a major county hospital. Pediatr Dent. 1992;14(3):152-157. (Retrospective chart review; 1248 patients) PMID: 1528783
76. * Connecticut Emergency Medical Services for Children (CT EMSC). Keep calm and chill on: intranasal Versed for pediatric anxiolysis in the community emergency department. Accessed December 1, 2024. (Guidelines)
101. * Nelson T, Nelson G. The role of sedation in contemporary pediatric dentistry. Dent Clin North Am. 2013;57(1):145-161. (Guideline) DOI: 10.1016/j.cden.2012.09.007
102. * Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116(15):1736-1754. (Guideline) DOI: 10.1161/CIRCULATIONAHA.106.183095
Subscribe to get the full list of 119 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
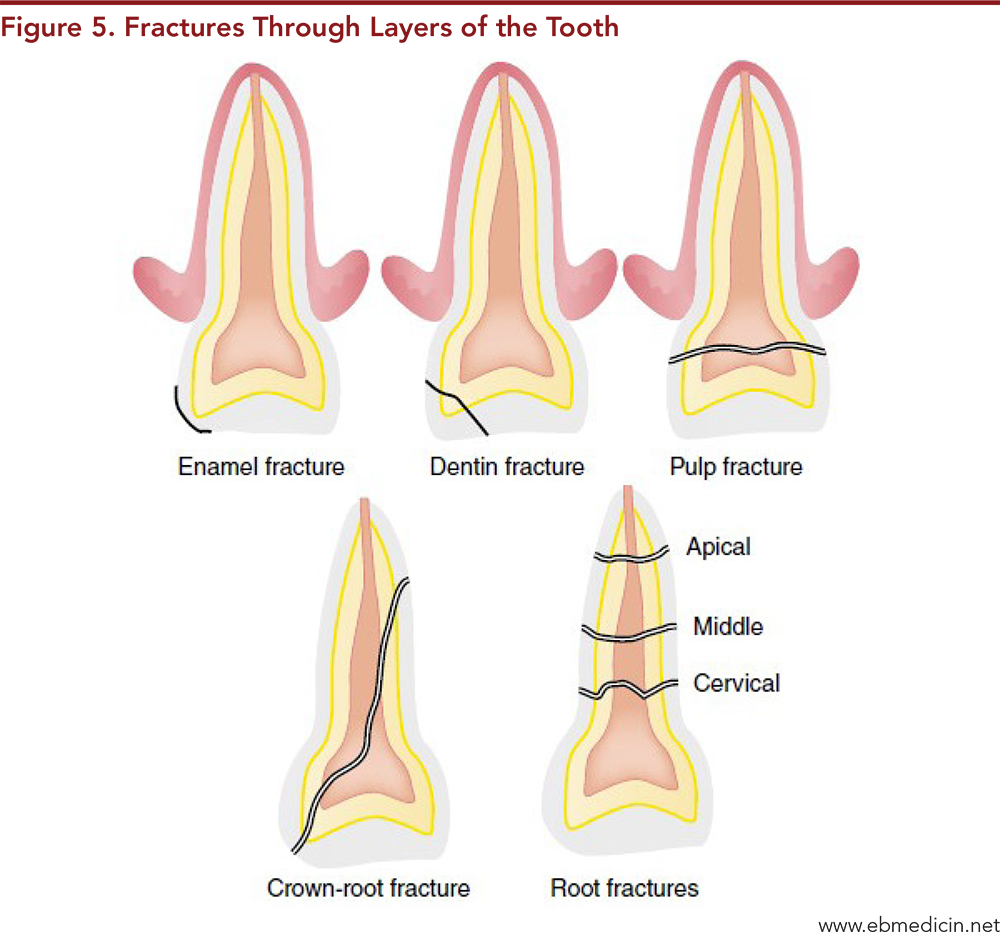
Keywords: Dental trauma, dental emergency, tooth trauma, oral trauma, dental injuries, dental injury, dental fracture, dental intrusion, dental extrusion, dental luxation, luxation tooth, dental avulsion, crown fracture, root fracture, crown-root fracture, concussion, subluxation, infraction, fractured tooth, tooth fracture, avulsed tooth, tooth avulsion, primary tooth, primary teeth, permanent tooth, permanent teeth, extraoral examination, intraoral examination, Ellis classification, tooth splint, tooth splinting, splint for teeth, dental splint, intraoral laceration, supraperiosteal infiltration, supraperiosteal nerve block, periodontal dressing paste
Joyce Li, MD, MPH
Michael Gorn, MD
December 15, 2024
December 15, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Trauma CME credits, subject to your state and institutional approval.