

The American Society of Anesthesiologists and the United Kingdom's Difficult Airway Society have generated and revised guidelines over the past 30 years based on analyses of the causes of airway catastrophes. Guideline components include airway management algorithms, equipment standardization, and routine training. Algorithms utilize intubation, supraglottic airway insertion, fiberoptic intubation, awake intubation, and front of neck surgical access. This review summarizes difficult airway management guidelines and discusses their application to trauma patients, including patients with physiologically difficult airways and patients with maxillofacial and laryngotracheal trauma.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
2. “EMS reported they were unable to intubate an 8-year-old patient who had been in a MVC. I’m residency trained in emergency medicine and expected I could easily secure the airway. However, the child had findings consistent with Pierre Robin sequence. I was unable to intubate, and I didn’t have an appropriate size SAD.” NAP4 and Closed Claims Analysis found that poor preparation was the cause of unnecessary mortalities.6,7 An EMS report of a difficult airway should prompt appropriate preparation, including opening the difficult airway cart.
3. “I called the on-call ENT and told him that we had a patient coming in who had tried to hang himself and was hypoxic despite SAD placement. ENT replied, 'OK, I’m available,' and hung up. ENT never arrived at the bedside.” Closed loop communication is essential to ensure that emergency clinicians and consultants understand each other. Development of a DART would also ensure that there were shared institutional expectations and accountability in such situations.
6. “I decided to prophylactically intubate my burn patient for transport even though she was effectively breathing spontaneously. We used RSI with etomidate and rocuronium. I was unable to intubate her or place an SAD, and she began to desaturate. I decided to awaken her, but it took 10 minutes to obtain sugammadex from pharmacy, by which time she had coded.” Weigh the risks versus benefits before proceeding with elective intubation and ensure that all rescue medications and airway adjuncts are readily available. A reversal agent should always be immediately available if long-acting paralytics are used.
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
2. * Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. 2022;136(1):31-81. (Guidelines) DOI: 10.1097/ALN.0000000000004002
4. * Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827-848. (Guidelines) DOI: 10.1093/bja/aev371
10. * Patel A, Saadi R, Lighthall JG. Securing the airway in maxillofacial trauma patients: a systematic review of techniques. Craniomaxillofac Trauma Reconstr. 2021;14(2):100-109. (Systematic review; 16 studies) DOI: 10.1177/1943387520950096
11. * Mercer SJ, Jones CP, Bridge M, et al. Systematic review of the anaesthetic management of non-iatrogenic acute adult airway trauma. Br J Anaesth. 2016;117 Suppl 1:i49-i59. (Systematic review) DOI: 10.1093/bja/aew193
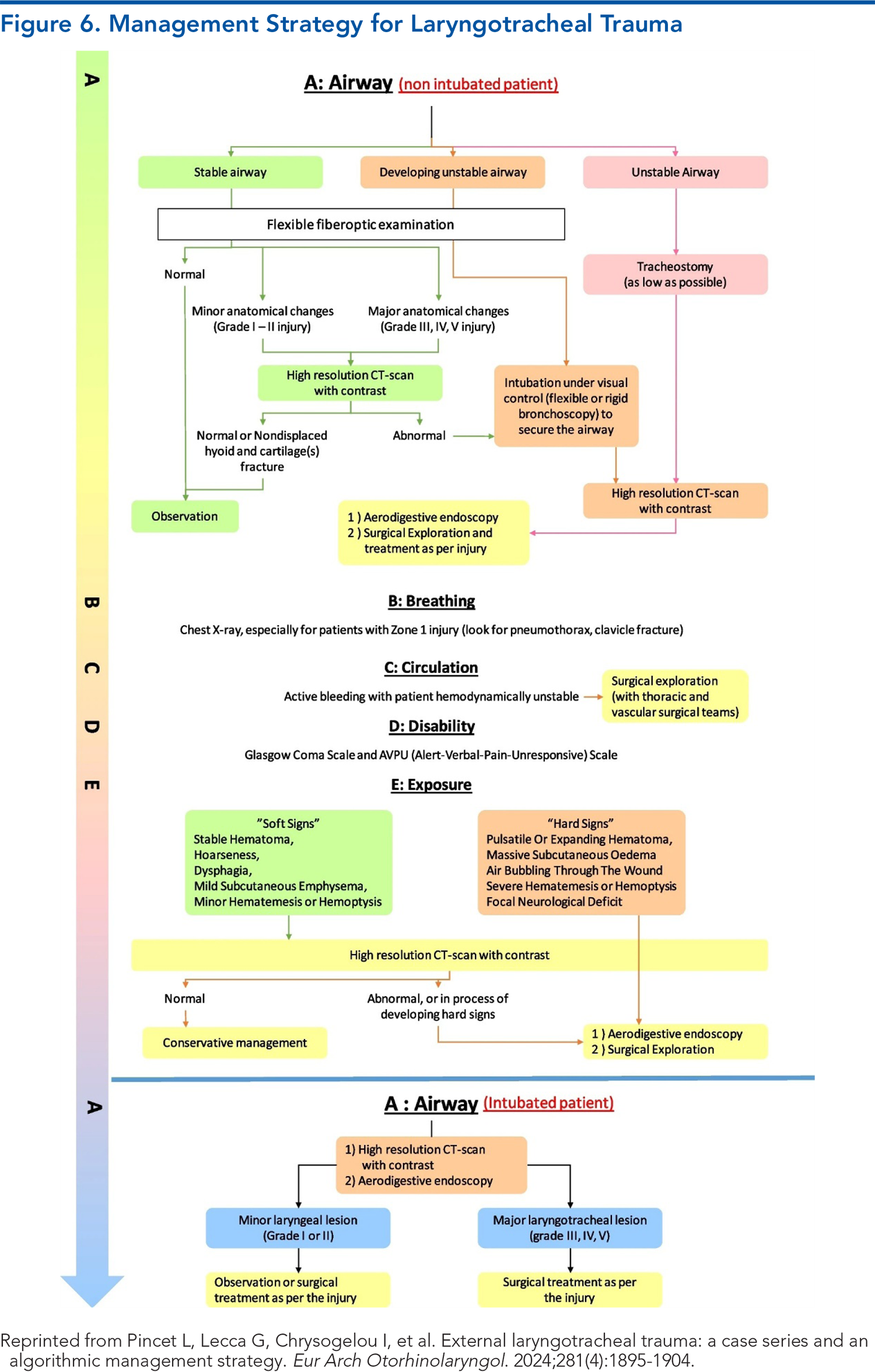
15. * Pincet L, Lecca G, Chrysogelou I, et al. External laryngotracheal trauma: a case series and an algorithmic management strategy. Eur Arch Otorhinolaryngol. 2024;281(4):1895-1904. (Case series) DOI: 10.1007/s00405-024-08456-9
18. * Kornas RL, Owyang CG, Sakles JC, et al. Evaluation and management of the physiologically difficult airway: consensus recommendations from Society for Airway Management. Anesth Analg. 2021;132(2):395-405. (Guidelines) DOI: 10.1213/ANE.0000000000005233
24. * Ahmad I, El-Boghdadly K, Bhagrath R, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020;75(4):509-528. (Guidelines) DOI: 10.1111/anae.14904
Subscribe to get the full list of 61 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: difficult airway, airway compromise, craniomaxillofacial trauma, laryngotracheal trauma, intubation, supraglottic airway device (SAD), front of neck access (FONA), physiologically difficult airway, extubation, surgical airway procedure, Difficult Airway Response Team (DART), direct laryngoscopy (DL), video laryngoscopy (VL), endotracheal tube (ETT), fiberoptic bronchoscopy, fiberoptic intubation, rapid sequence induction (RSI), laryngeal handshake, “stab, twist, bougie, tube” technique, cricothyroidotomy, difficult airway cart, modified Mallampati test, bag valve mask ventilation
Christian Menard, MD, PhD, FACEP; Sarah Pierce, CRNA; Thomas R. deTar, MD, FACS
Heatherlee Bailey, MD, FAAEM, MCCM; Kamal Gursahani, MD, MBA
August 15, 2025
August 15, 2028 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Trauma credits, subject to your state and institutional approval.