Table of Contents
About This Issue
As laws and regulations surrounding the use of medical and recreational cannabis use continue to evolve, emergency departments are increasingly managing patients experiencing ill effects of phytocannabinoids and synthetic cannabinoids. In this issue, you will learn:
What the differences are between phytocannabinoids and synthetic cannabinoids in chemical composition and their effects on physiological processes.
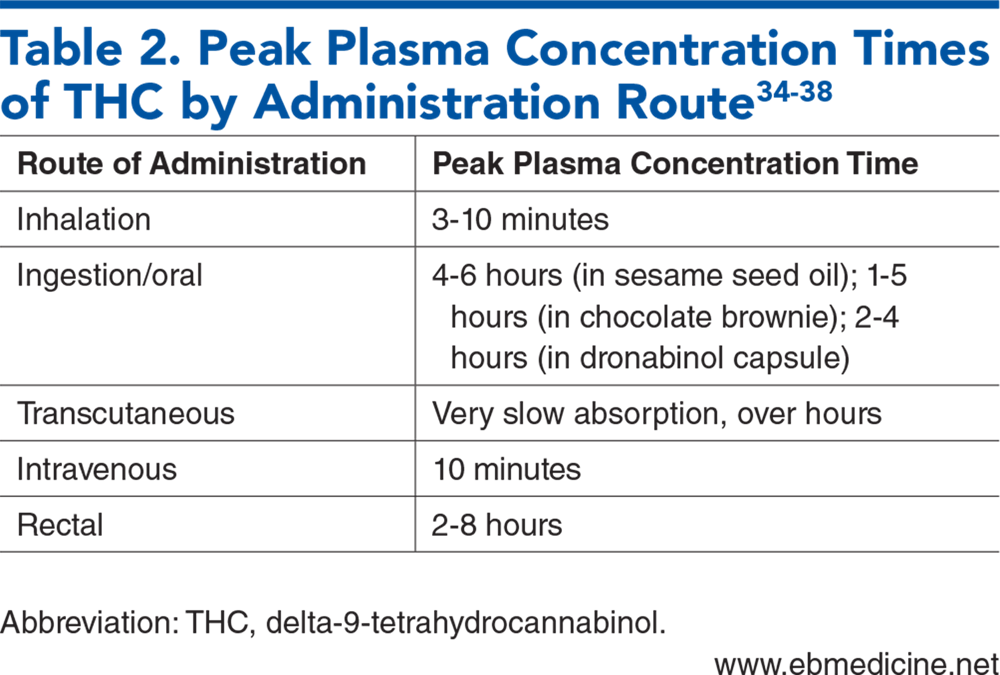
The different formulations of cannabis delivery routes, and the expected timelines of symptom appearance.
What case reports and data show are the most significant effects of cannabis on the neuropsychiatric, cardiovascular, renal, metabolic, and gastrointestinal systems.
How cannabinoid hyperemesis syndrome (CHS) can be differentiated from other vomiting syndromes.
The latest evidence on treatments that will help manage CHS: antiemetics, butyrophenones, metoclopramide, and IV hydration.
The signs, symptoms, and treatment options for patients with cannabis withdrawal.
The special considerations for pediatric patients who present to the ED with signs of cannabinoid use.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- The Endogenous Cannabinoid System
- Phytocannabinoids
- Synthetic Cannabinoids
- Current Indications for Cannabinoids
- Formulations and Routes of Administration
- Clinical Findings Associated with Cannabis Use
- Psychiatric Effects
- Cardiovascular Effects
- Pulmonary Effects
- Renal Effects
- Metabolic Effects
- Oral/Dental Effects
- Ophthalmologic Effects
- Cannabinoid Hyperemesis Syndrome
- Cannabis Withdrawal
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Laboratory Testing
- Electrocardiogram
- Imaging
- Treatment
- Treatment for Acute Cannabis and Synthetic Cannabinoid Toxicity
- Treatment for Cannabinoid Hyperemesis Syndrome
- Hot-Water Showers and Bathing
- Medications
- Butyrophenones
- Capsaicin
- Managing Refractory Cannabinoid Hyperemesis Syndrome
- Treatment for Cannabis Withdrawal
- Special Populations
- Pediatric Patients
- Testing and Screening
- Special Considerations in Pediatric Presentations of Cannabis Exposure
- Pregnant Patients
- Controversies and Cutting Edge
- Legal Status of Cannabis and Cannabinoids
- Disposition
- Risk Management Pitfalls for Emergency Department Management of Patients With Acute Cannabinoid Use
- Summary
- 5 Things That Will Change Your Practice
- Time- and Cost-Effective Strategies
- Case Conclusions
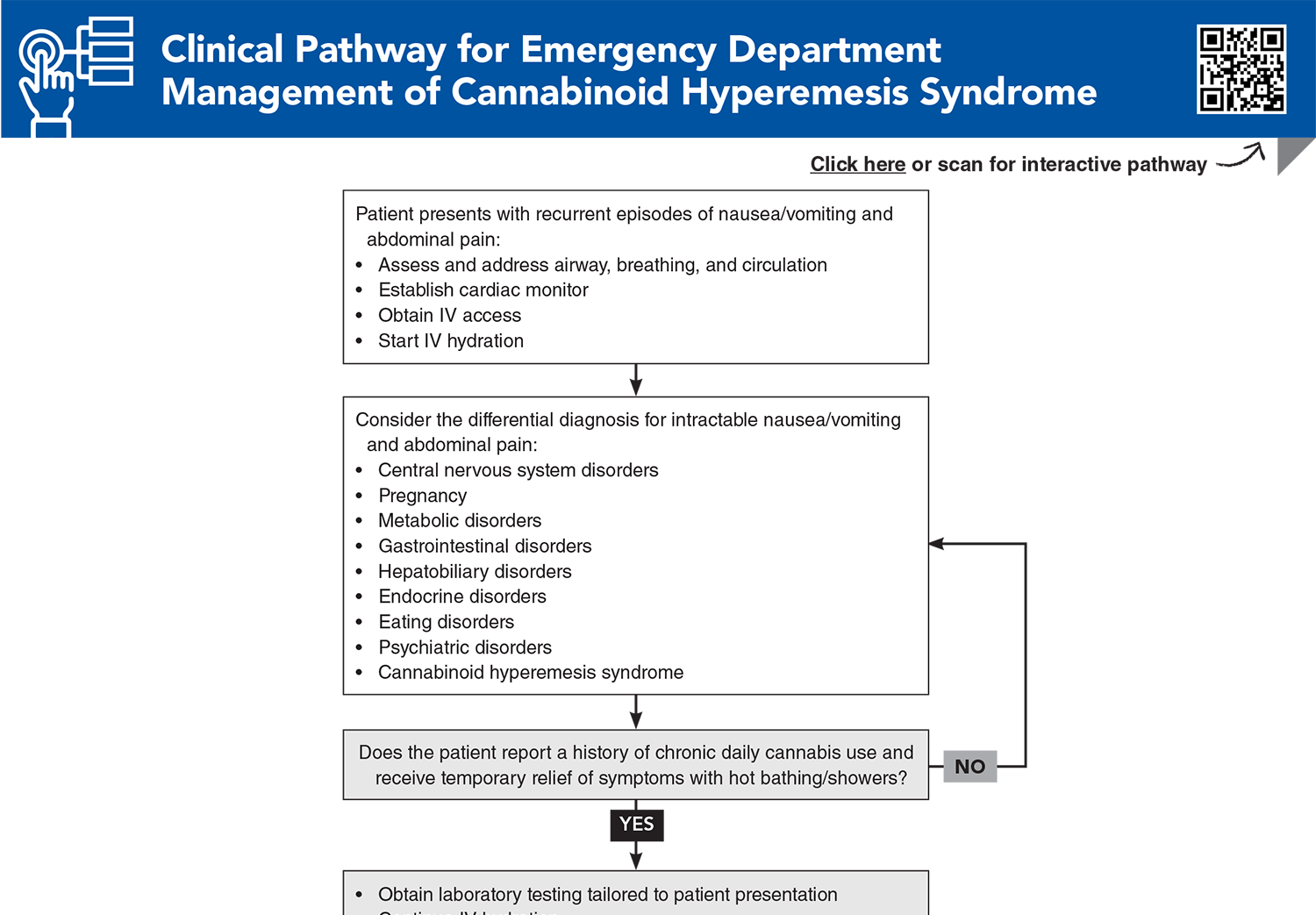
- Clinical Pathway for Emergency Department Management of Cannabinoid Hyperemesis Syndrome
- Tables
- References
Abstract
Despite current legal and medical controversies surrounding cannabinoids, it is a fact that emergency departments are seeing an increasing number of patients presenting with symptoms associated with the use of these drugs. This review outlines the pathophysiology of cannabinoids, the potential clinical findings associated with their use, and the current evidence for best-practice management of patients who present with signs of acute intoxication and chronic use. Differences between natural and synthetic cannabinoids are discussed, along with evidence for diagnosing and managing patients presenting with the intractable vomiting of cannabinoid hyperemesis syndrome. Emerging treatments for cannabinoid hyperemesis syndrome are presented as well as an update on the legal status of medical cannabinoid substances.
Case Presentations
- The patient was observed to stumble and fall as she attempted to board a bus. Upon arrival to the ED, she said, “I feel fine, everything is OK. I just smoked a little pot and felt light-headed.”
- On evaluation, the patient is seated comfortably on the stretcher but nods off during questioning. She reports a past medical history of anxiety. Her vital signs are: temperature, 37.2°C; heart rate, 107 beats/min; blood pressure, 135/77 mm Hg; respiratory rate, 16 breaths/min while seated; and oxygen saturation, 98% on room air. Upon examination, you note conjunctival injection, dry oral mucosa, and tachycardia, but the examination is otherwise unremarkable, including neurologic assessment.
- At the end of your encounter, the patient says “thanks,” and requests to leave the ED for work. You consider whether she should have a syncope workup and be kept for observation. Because you suspect cannabis intoxication, perhaps she should be advised to not go to work…
- His mother called 911 because she found him behaving strangely when she arrived home from work.
- The patient appears very agitated and is unable to remain seated on the stretcher during your examination. He reports chest pain and palpitations, and his vital signs are: temperature, 38°C; heart rate, 146 beats/min; blood pressure, 169/99 mm Hg; respiratory rate, 21 breaths/min; and oxygen saturation, 100% on room air. Fingerstick glucose is measured at 65 mg/dL.
- You suspect a toxic ingestion and wonder what diagnostic tests and/or interventions are indicated…
- You note in his records that he has made frequent visits to the ED over the past 2 years for abdominal pain and intractable vomiting. His vital signs are unremarkable.
- The patient reports that his symptoms have become so severe over the last 2 months that he has had to visit the ED frequently to gain relief, and has lost approximately 10 pounds over the last month. He says that over that time, he has had multiple blood draws in the ED and by his primary care doctor, ultrasounds of the complete abdomen, 2 CT scans of the abdomen/pelvis, and an esophagogastroduodenoscopy, revealing chronic gastritis, with no evidence of peptic ulcer disease or Helicobacter pylori. The patient states that his symptoms are usually very difficult to control, and he is frequently admitted and later discharged home with a diagnosis of gastritis, only to return again the next month.
- You develop a differential for intractable vomiting and then ask the patient a key question that leads to the diagnosis…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Cannabinoid Hyperemesis Syndrome
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables
Subscribe for full access to all Tables.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
24. * de Oliveira MC, Vides MC, Lassi DLS, et al. Toxicity of synthetic cannabinoids in K2/spice: a systematic review. Brain Sci. 2023;13(7):990. (Review) DOI: 10.3390/brainsci13070990
29. * Prete MM, Feitosa GTB, Ribeiro MAT, et al. Adverse clinical effects associated with the use of synthetic cannabinoids: a systematic review. Drug Alcohol Depend. 2025;272:112698. (Systematic review; 49 studies) DOI: 10.1016/j.drugalcdep.2025.112698
74. * Loganathan P, Gajendran M, Goyal H. A comprehensive review and update on cannabis hyperemesis syndrome. Pharmaceuticals (Basel). 2024;17(11):1549. (Review) DOI: 10.3390/ph17111549
75. * Razban M, Exadaktylos AK, Santa VD, et al. Cannabinoid hyperemesis syndrome and cannabis withdrawal syndrome: a review of the management of cannabis-related syndrome in the emergency department. Int J Emerg Med. 2022;15(1):45. (Review) DOI: 10.1186/s12245-022-00446-0
99. * Richards JR, Gordon BK, Danielson AR, et al. Pharmacologic treatment of cannabinoid hyperemesis syndrome: a systematic review. Pharmacotherapy. 2017;37(6):725-734. (Systematic review; 63 studies) DOI: 10.1002/phar.1931
100. *Sorensen CJ, DeSanto K, Borgelt L, et al. Cannabinoid hyperemesis syndrome: diagnosis, pathophysiology, and treatment-a systematic review. J Med Toxicol. 2017;13(1):71-87. (Systematic review; 183 studies) DOI: 10.1007/s13181-016-0595-z
111. *Borgundvaag B, Bellolio F, Miles I, et al. Guidelines for reasonable and appropriate care in the emergency department (GRACE-4): alcohol use disorder and cannabinoid hyperemesis syndrome management in the emergency department. Acad Emerg Med. 2024;31(5):425-455. (Guidelines) DOI: 10.1111/acem.14911
121. *Spiga F, Parkhouse T, Tang VM, et al. Pharmacotherapies for cannabis use disorder. Cochrane Database Syst Rev. 2025;9(9):CD008940. (Cochrane review; 35 randomized controlled trials) DOI: 10.1002/14651858.CD008940.pub4
Subscribe to get the full list of 154 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: cannabis, cannabinoid, synthetic, hyperemesis, vomiting, withdrawal, butyrophenone, antiemetic, pediatric