

Acute stroke is one of the most common neurologic emergencies encountered by emergency clinicians. While point-of-care ultrasound has been a core part of emergency clinicians’ training and practice for many years, the use of specialized ultrasound modalities in the care of acute ischemic stroke has not been as widely adopted. This review discusses the use of ultrasound in acute stroke, with a focus on applications of interest to emergency clinicians. Transcranial Doppler, carotid Doppler, microembolic signal detection, transthoracic echocardiography, evaluation for collateral circulation, and optic nerve sheath diameter measurement are discussed in a case-based format, with a focus on practical applications for emergency clinicians.
Acute stroke is one of the most common neurologic emergencies and causes of significant disability worldwide.1 Thrombolysis and mechanical thrombectomy, the mainstays of acute ischemic stroke care, are time-sensitive interventions and therefore require rapid evaluation in the emergency department (ED). While the initial evaluation of patients suspected of suffering from acute stroke has been standardized and operationalized by most institutions through “code stroke” or “brain code” protocols, computed tomography (CT)-based imaging is sometimes not immediately available or may not reveal the cause of the neurological change.
Emergency clinicians are responsible for the care of most acute stroke patients presenting to EDs in the United States. Their role in acute stroke care, as well as expertise in point-of-care ultrasound (POCUS), makes the use of ultrasound in the care of acute stroke patients a topic of interest for emergency clinicians. Currently, neurovascular ultrasound (ie, transcranial Doppler [TCD] and carotid ultrasound) in stroke is primarily performed by neurovascular sonographers in an accredited neurovascular ultrasound laboratory. However, emergency clinicians need to be aware of the indications for performing neuro-ultrasound in acute stroke patients. This review will discuss the use of ultrasound in patients with acute ischemic strokes and transient ischemic attacks (TIAs), utilizing clinical cases to answer some key questions:
The clinical cases presented in this issue are intended to serve as a reference for emergency clinicians to understand the clinical-decision framework for the cerebrovascular evaluation of acute ischemic stroke and TIA. However, these case discussions are not a substitute for guideline-based evaluation and management of patients in consultation with a neurologist. Institutional practice and consultation availability vary, within the United States and internationally. Emergency clinicians should continue to follow their institutional standards in these matters.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
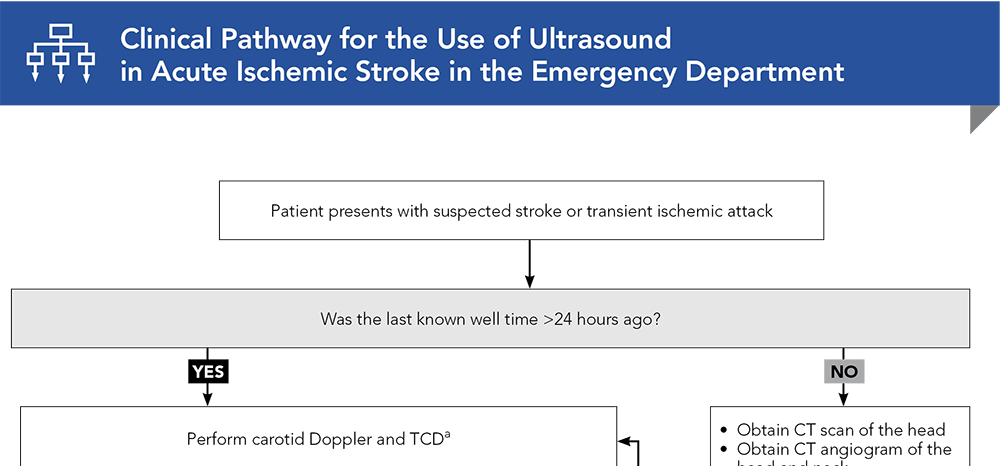
Subscribe to access the complete flowchart to guide your clinical decision making.
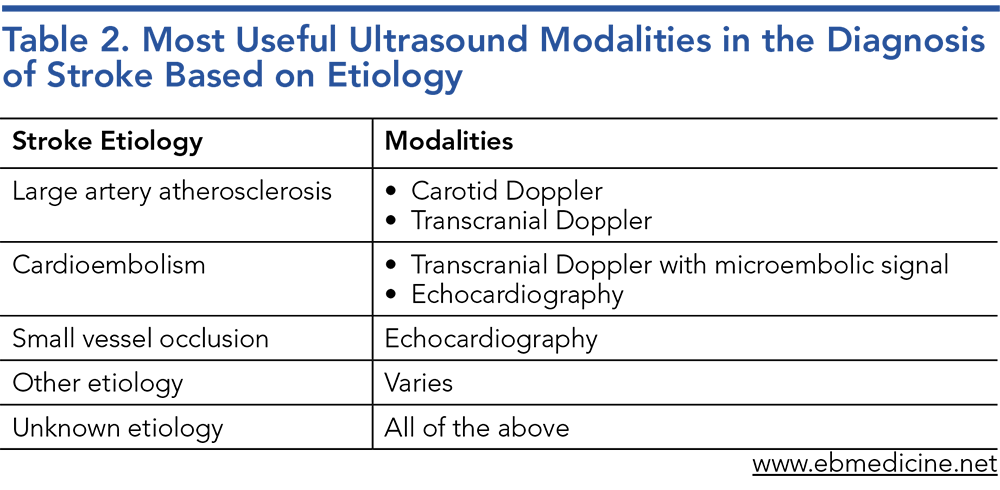

Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
4. * Alexandrov AV, Sloan MA, Wong LKS, et al. Practice standards for transcranial Doppler ultrasound: part I-test performance. J Neuroimaging. 2007;17(1):11-18. (Guideline) DOI: 10.1111/j.1552-6569.2006.00088.x
6. * Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35-41. (Feasibility of stroke classification system; 20 patients) DOI: 10.1161/01.str.24.1.35
7. * Lovett JK, Coull AJ, Rothwell PM. Early risk of recurrence by subtype of ischemic stroke in population-based incidence studies. Neurology. 2004;62(4):569-573. (Meta-analysis; 2 studies, 1709 patients) DOI: 10.1212/01.wnl.0000106917.39526.56
9. * Abbott AL, Paraskevas KI, Kakkos SK, et al. Systematic review of guidelines for the management of asymptomatic and symptomatic carotid stenosis. Stroke. 2015;46(11):3288-3301. (Systematic review; 34 guidelines) DOI: 10.1161/strokeaha.115.009985
15. * Brunser AM, Mansilla E, Hoppe A, et al. The role of TCD in the evaluation of acute stroke: TCD in acute stroke. J Neuroimaging. 2016;26(4):420-425. (Prospective observational study; 86 patients) DOI: 10.1111/jon.12334
17. * Bazan R, Luvizutto GJ, Braga GP, et al. Relationship of spontaneous microembolic signals to risk stratification, recurrence, severity, and mortality of ischemic stroke: a prospective study. Ultrasound J. 2020;12(1):6. (Prospective cohort; 111 patients) DOI: 10.1186/s13089-020-0156-1
18. * Spence JD, Tamayo A, Lownie SP, et al. Absence of microemboli on transcranial Doppler identifies low-risk patients with asymptomatic carotid stenosis. Stroke. 2005;36(11):2373-2378. (Prospective cohort; 319 patients) DOI: 10.1161/01.STR.0000189651.90810.8d
19. * Markus HS, King A, Shipley M, et al. Asymptomatic embolisation for prediction of stroke in the asymptomatic carotid emboli study (ACES): a prospective observational study. Lancet Neurol. 2010;9:7:663-671. (Prospective observational study; 467 patients) DOI: 10.1016/S1474-4422(10)70120-4
21. * Best LMJ, Webb AC, Gurusamy KS, et al. Transcranial Doppler ultrasound detection of microemboli as a predictor of cerebral events in patients with symptomatic and asymptomatic carotid disease: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2016;52(5):565-580. (Meta-analysis; 38 studies) DOI: 10.1016/j.ejvs.2016.07.015
25. * Saqqur M, Khan K, Derksen C, et al. Transcranial Doppler and transcranial color duplex in defining collateral cerebral blood flow: TCD and TCCD in defining collateral blood flow. J Neuroimaging. 2018;28(5):455-476. (Narrative review) DOI: 10.1111/jon.12535
27. * Messé SR, Gronseth GS, Kent DM, et al. Practice advisory update summary: patent foramen ovale and secondary stroke prevention: report of the Guideline Subcommittee of the American Academy of Neurology. Neurology. 2020;94(20):876-885. (Guideline) DOI: 10.1212/wnl.0000000000009563
Subscribe to get the full list of 29 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: Neurovascular ultrasound, POCUS, Transcranial Doppler, carotid Doppler, microembolic signal detection, transthoracic echocardiography, collateral circulation, flow velocity, optic nerve sheath diameter measurement, high-intensity transient signals, POCUS, acute ischemic stroke, transient ischemic attack, TIA
Grigory Ostrovskiy, MD; Alexandra S. Reynolds, MD, RPNI; Aarti Sarwal, MD, FNCS, FAAN, FCCM, RPNI
Ryan Hakimi, DO, MS, NVS, RPNI, CPB, FNCS, FCCM, FAAN; Jennifer H. Kang, MD
May 15, 2024
May 15, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 4 Stroke CME credits, subject to your state and institutional approval.