

Portions of this content were previously published in: Molyneux K, Vaswani S. Emergency Department Management of Patients With Low Back Pain: A Review of Current Evidence. Emerg Med Pract. 2024; 26(11):1-24. Used with permission of EB Medicine.
Low back pain is a common presentation in the urgent care setting, and determining whether the cause is benign, serious, or even life-threatening can be challenging. A systematic strategy for the history and physical examination can help reduce unnecessary imaging, and an evidence-based approach will inform safe and effective pain management recommendations. This issue reviews the evidence on red-flag signs and symptoms for low back pain, current diagnostic studies recommendations, and best-practice treatment and disposition strategies.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
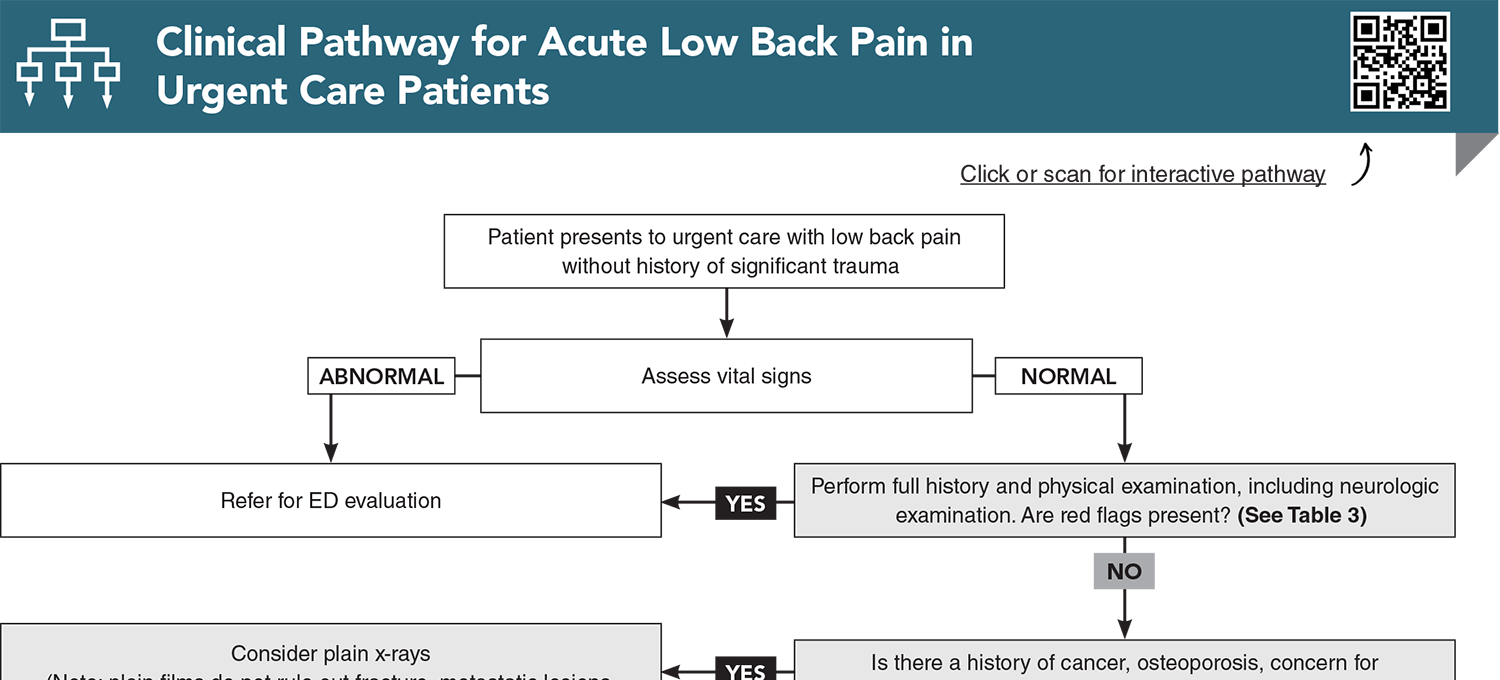
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
2. * Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60(10):3072-3080. (Cohort; 1172 patients) DOI: 10.1002/art.24853
5. * Han CS, Hancock MJ, Downie A, et al. Red flags to screen for vertebral fracture in people presenting with low back pain. Cochrane Database Syst Rev. 2023;8(8):CD014461. (Cochrane review; 14 studies) DOI: 10.1002/14651858.CD014461.pub2
9. * Anderson SW, Bhattacharjee S, Patanwala AE. Effect of opioid analgesics on emergency department length of stay among low back pain patients in the United States. Am J Emerg Med. 2020;38(9):1802-1806. (Comparative study; 8.6 million visits) DOI: 10.1016/j.ajem.2020.06.002
17. * Galliker G, Scherer DE, Trippolini MA, et al. Low back pain in the emergency department: prevalence of serious spinal pathologies and diagnostic accuracy of red flags. Am J Med. 2020;133(1):60-72. (Systematic review; 22 studies, 41,320 patients) DOI: 10.1016/j.amjmed.2019.06.005
24. * Shaw B, Kinsella R, Henschke N, et al. Back pain “red flags”: which are most predictive of serious pathology in the emergency department? Eur Spine J. 2020;29(8):1870-1878. (Retrospective observational study; 1000 patients) DOI: 10.1007/s00586-020-06452-1
25. * Expert Panel on Neurological Imaging and Musculoskeletal Imaging, Beckmann NM, West OC, et al. ACR Appropriateness Criteria® suspected spine trauma. J Am Coll Radiol. 2019;16(5S):S264-S285. (Practice guideline) DOI: 10.1016/j.jacr.2019.02.002
36. * Ropper AH, Zafonte RD. Sciatica. N Engl J Med. 2015;372(13):1240-1248. (Review) DOI: 10.1056/NEJMra1410151
38. * Macedo F, Annaswamy T, Coller R, et al. Diagnosis and treatment of low back pain: ynopsis of the 2021 US Department of Veterans Affairs and US Department of Defense clinical practice guideline. Am J Phys Med Rehabil. 2024;103(4):350-355. (Practice guideline) DOI: 10.1097/PHM.0000000000002356
39. * Chiarotto A, Koes BW. Nonspecific low back pain. N Engl J Med. 2022;386(18):1732-1740. (Review) DOI: 10.1056/NEJMcp2032396
43. * Chou R, Fu R, Carrino JA, et al. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. 2009;373(9662):463-472. (Meta-analysis; 7 studies) DOI: 10.1016/S0140-6736(09)60172-0
47. * Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002;137(7):586-597. (Review) DOI: 10.7326/0003-4819-137-7-200210010-00010
49. * Hutchins TA, Peckham M, Shah LM, et al. ACR Appropriateness Criteria® low back pain: 2021 update. J Am Coll Radiol. 2021;18(11s):S361-S379. (Practice guideline) DOI: 10.1016/j.jacr.2021.08.002
50. * Patel ND, Broderick DF, Burns J, et al. ACR Appropriateness Criteria® low back pain. J Am Coll Radiol. 2016;13(9):1069-1078. (Practice guideline) DOI: 10.1016/j.jacr.2016.06.008
53. * Cashin AG, Wand BM, O’Connell NE, et al. Pharmacological treatments for low back pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2023;4(4):CD013815. (Cochrane review; 103 studies) DOI: 10.1002/14651858.CD013815.pub2
55. * Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514-530. (Practice guideline) DOI: 10.7326/M16-2367
60. * van der Gaag WH, Roelofs PD, Enthoven WT, et al. Non-steroidal anti-inflammatory drugs for acute low back pain. Cochrane Database Syst Rev. 2020;4(4):CD013581. (Cochrane review; 32 trials, 5356 participants) DOI: 10.1002/14651858.CD013581
65. * Cashin AG, Folly T, Bagg MK, et al. Efficacy, acceptability, and safety of muscle relaxants for adults with non-specific low back pain: systematic review and meta-analysis. BMJ. 2021;374:n1446. (Systematic review/meta-analysis; 49 trials) DOI: 10.1136/bmj.n1446
66. * Friedman BW, Dym AA, Davitt M, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: a randomized clinical trial. JAMA. 2015;314(15):1572-1580. (Randomized controlled trial; 323 patients) DOI: 10.1001/jama.2015.13043
84. * Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79-86. (Systematic review; 11 guidelines) DOI: 10.1136/bjsports-2018-099878
89. * Dahm KT, Brurberg KG, Jamtvedt G, et al. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010(6):CD007612. (Cochrane review/meta-analysis; 10 randomized controlled trials) DOI: 10.1002/14651858.CD007612.pub2
Subscribe to get the full list of 99 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: low back pain, cauda equina syndrome, spinal epidural abscess, spinal stenosis, pseudoclaudication, disk herniation, sciatica, straight leg raise test, crossed leg raise test, lumbar, spinal cord compression, spinal cord, lumbar stress fractures, spinal epidural hematoma, spondylosis, spondylodiscitis, transverse myelitis, conus medullaris syndrome, topical NSAIDs, topical diclofenac, topical menthol, skeletal muscle relaxants
Tracey Quail Davidoff, MD, FCUCM
Martha Williams, DHSc, MS, PA-C; Roger Wu, MD, MBA
September 1, 2025