Table of Contents
About This Issue
Sports injuries are common, and patients with these injuries often present to the emergency department (ED) for evaluation and treatment. It is sometimes difficult to differentiate apophyseal injuries from other common pediatric sports injuries. Prompt recognition of apophyseal injuries can help facilitate optimal healing, prevent future injury, and minimize unnecessary testing. This issue reviews the classic clinical findings associated with apophysitis, offers guidance for evaluation, and provides evidence-based recommendations for the management of patients with apophyseal injuries in the ED. In this issue, you will learn:
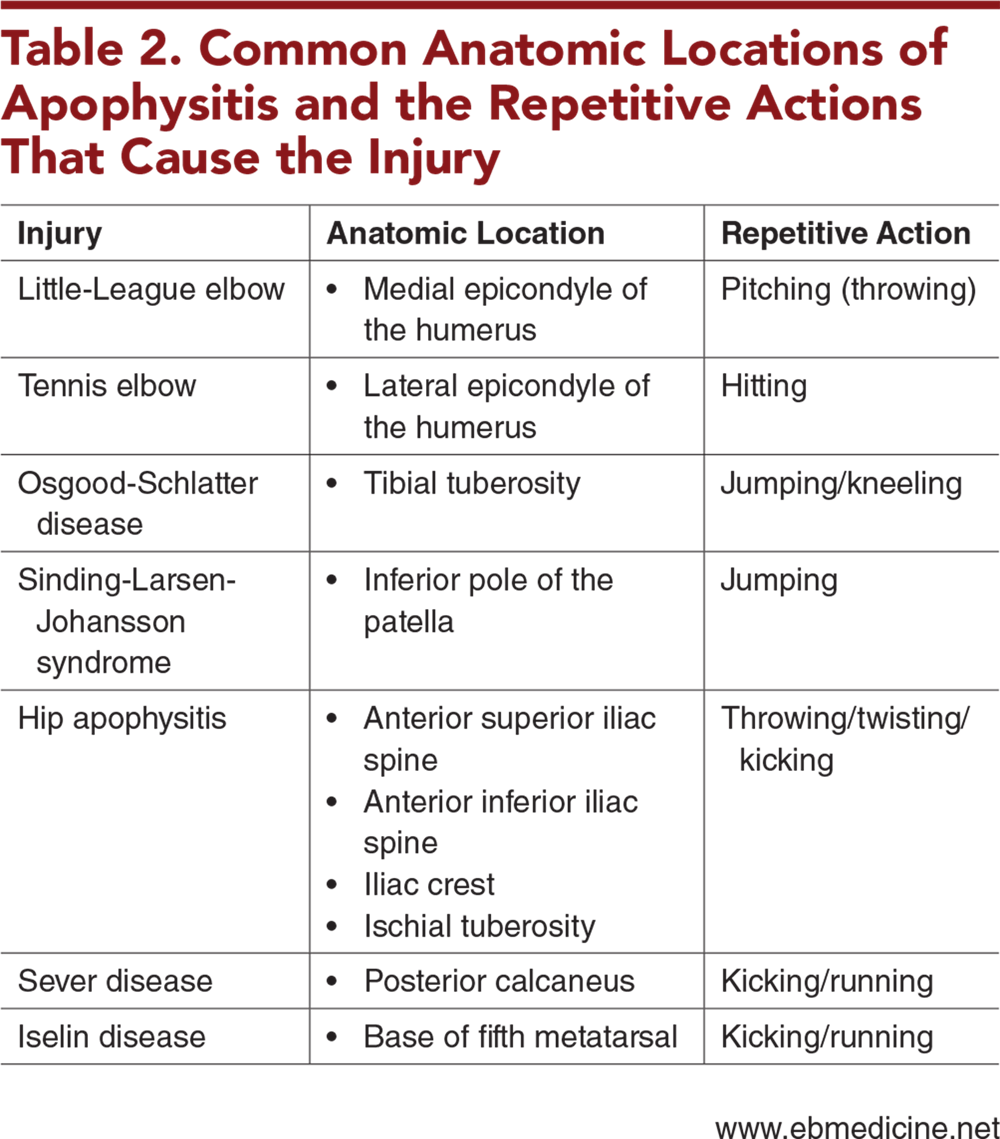
Common locations of apophysitis and the repetitive actions that cause those injuries
Red-flag symptoms that can help differentiate apophysitis from more serious conditions
Key questions to ask when obtaining the history that will help narrow the diagnosis
Physical examination findings that can aid in confirming the diagnosis
Which imaging studies are useful for evaluation of apophysitis
Which medications are the treatment of choice for apophysitis
Which adjunctive therapies have been shown to be effective
Recommendations for severe or refractive apophysitis
Which patients can be safely discharged home with return precautions and follow-up with their primary care provider
When follow-up with orthopedics or sprots medicine is indicated
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Treatment
- Medications
- Adjunctive Devices
- Physical Therapy
- Severe or Refractory Disease
- Preventative Measures
- Controversies and Cutting Edge
- Disposition
- Risk Management Pitfalls in Emergency Department Management of Patients With Apophysitis
- Case Conclusions
- 5 Things That Will Change Your Practice
- Summary
- Time- and Cost-Effective Strategies
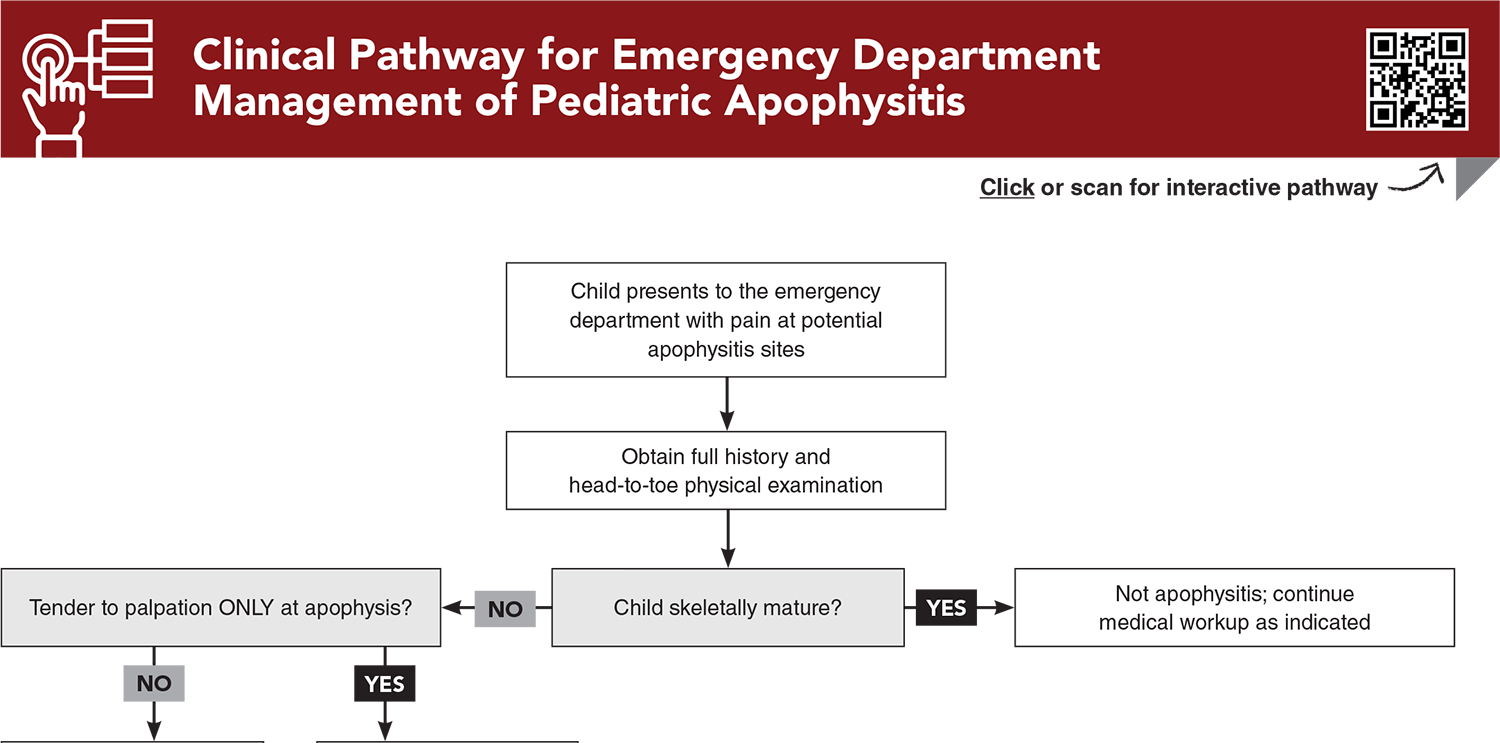
- Clinical Pathway for Emergency Department Management of Pediatric Apophysitis
- Tables and Figures
- References
Abstract
Children with sports injuries often present to the emergency department for evaluation and treatment. It can be difficult to differentiate apophyseal injuries from other common pediatric sports medicine injuries, such as fractures, muscular injuries, or ligamentous injuries. However, recognition of apophyseal injuries can help facilitate optimal healing, prevent future injury, and minimize unnecessary testing. This issue aims to help the emergency clinician correctly identify the major anatomic areas of apophysitis in a child, diagnose the condition, and appropriately manage apophyseal injuries in the emergency department. Guidance for activity modification and return precautions are also provided, and indications for when to refer the patient to a specialist are also reviewed.
Case Presentations
- The patient has been playing basketball for the past month as part of practices for the upcoming season. To address the pain, the boy’s mother has been giving him ibuprofen “every so often,” but she has not tried other medications or interventions. The patient reports that it hurts particularly in the right heel when he jumps and lands on his feet.
- The boy has had no fevers, rashes, night sweats, or weight loss. The review of systems is negative. On examination, he has an antalgic gait but is able to bear weight. He has full range of motion of the right foot and ankle, and he is neurovascularly intact. He has a positive calcaneal squeeze test. His physical examination is otherwise negative.
- What diagnoses are on your differential?
- The girl is a soccer player and has been participating in a soccer camp this past week. She has been playing for approximately 5 hours a day. She has had some vague knee pain, but on the afternoon of presentation, she had worsening discomfort “just below the knee” and noticed a “bump” that she had not noticed before. The girl reports the pain as 7/10, especially when she is trying to squat or kneel. She is able to bear weight but with some difficulty.
- The girl has not had any fevers, rashes, night sweats, weight gain, or weight loss. She has not yet started her menstrual cycle. To try to relieve the pain, she tried acetaminophen, without much relief, but icing the knee seemed to help. Her physical examination is notable for point tenderness to the right tibial tuberosity, with mild surrounding edema without overlying erythema or calor.
- What management recommendations do you have for this patient?
- The boy is a high-level pitcher on his Little League team. The boy tells you his team hopes to make the Little League World Series this year, and he is the best pitcher on the team. He reports that he has been pitching multiple innings “almost every game.” He recently had a growth spurt but has otherwise been in his normal state of health.
- On examination, he has point tenderness to the medial epicondyle and winces in pain. He is neurovascularly intact otherwise, with good perfusion and full muscle strength.
- Do this patient’s symptoms warrant emergent orthopedic evaluation or outpatient orthopedic follow-up?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Pediatric Apophysitis
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Jones C, Wolf M, Herman M. Acute and chronic growth plate injuries. Pediatr Rev. 2017;38(3):129-138. (Review) DOI: 10.1542/pir.2015-0160
3. * DiFiori JP, Benjamin HJ, Brenner J, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24(1):3-20. (Review) DOI: 10.1097/JSM.0000000000000060
21. * Nakase J, Goshima K, Numata H, et al. Precise risk factors for Osgood-Schlatter disease. Arch Orthop Trauma Surg. 2015;135(9):1277-1281. (Prospective study; 300 patients) DOI: 10.1007/s00402-015-2270-2
25. * Gaulrapp H, Nuhrenborger C. The Osgood-Schlatter disease: a large clinical series with evaluation of risk factors, natural course, and outcomes. Int Orthop. 2022;46(2):197-204. (Prospective study; 126 patients) DOI: 10.1007/s00264-021-05178-z
32. * Neuhaus C, Appenzeller-Herzog C, Faude O. A systematic review on conservative treatment options for Osgood-Schlatter disease. Phys Ther Sport. 2021;49:178-187. (Systematic review; 28 studies, 747 patients) DOI: 10.1016/j.ptsp.2021.03.002
Subscribe to get the full list of 42 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: apophysitis, apophysis, apophysis inflammation, apophyseal injury, overuse injury, sports injury, Osgood-Schlatter disease, Sever disease, Little League elbow, Sinding-Larsen-Johansson disease, Iselin disease, tennis elbow, calcaneal squeeze test