Table of Contents
About This Issue
Low back pain (LBP) in emergency department patients is typically the result of relatively benign causes, but emergency clinicians must be vigilant in identifying the red-flag signs that can signal potential disability, death, and legal liability. In this issue you will learn:
What are the likelihood ratios of red-flag findings in patients with LBP?
How can the key signs of cauda equina syndrome be differentiated from sciatica, spinal stenosis, and disk herniation?
What are the risk factors for infectious causes of LBP?
What percentage of patients with spinal epidural abscess present with the classic triad of fever, back pain, and neurologic deficits?
What might be the cause of pain referred to the low back, and can they be life-threatening?
Are laboratory studies helpful when there is suspicion for infectious causes of LBP?
X-ray, CT, and MRI: which test (if any) is best?
What are the indications for emergent surgical consult?
Are there any medications or nonpharmacologic therapies that show evidence of usefulness?
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Mechanical
- Intervertebral Disc Herniation
- Fracture
- Compression Syndromes
- Spinal Epidural Hematoma
- Sciatica
- Spondylosis
- Compartment Syndrome
- Infectious
- Spondylodiscitis
- Spinal Epidural Abscess
- Inflammatory
- Referred Pain
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Compression and Mechanical Causes
- Conus Medullaris Syndrome
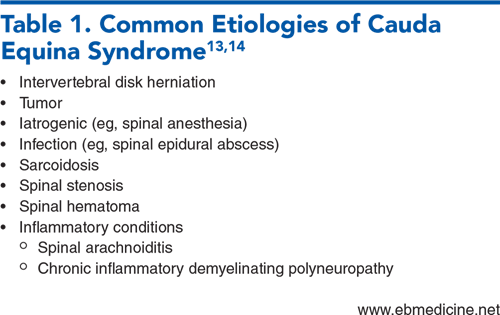
- Cauda Equina Syndrome
- Malignancy
- Fracture
- Spinal Stenosis and Herniation
- Infectious Causes
- Referred Pain Causes
- Physical Examination
- Diagnostic Studies
- Laboratory Testing
- Imaging Studies
- X-ray
- Computed Tomography
- Magnetic Resonance Imaging
- Ultrasound
- Treatment
- Treatment of Emergent Causes of Back Pain
- Treatment for Nonspecific Back Pain
- Nonsteroidal Anti-Inflammatory Drugs
- Acetaminophen
- Skeletal Muscle Relaxants
- Opioids
- Corticosteroids
- Diazepam
- Gabapentin
- Trigger Point Injections
- Nonpharmacologic Management
- Controversies and Cutting Edge
- Disposition
- Summary
- Time- and Cost-Effective Strategies
- Risk Management Pitfalls in Emergency Department Management of Patients With Low Back Pain
- 5 Things That Will Change Your Practice
- Case Conclusions
- Clinical Pathways
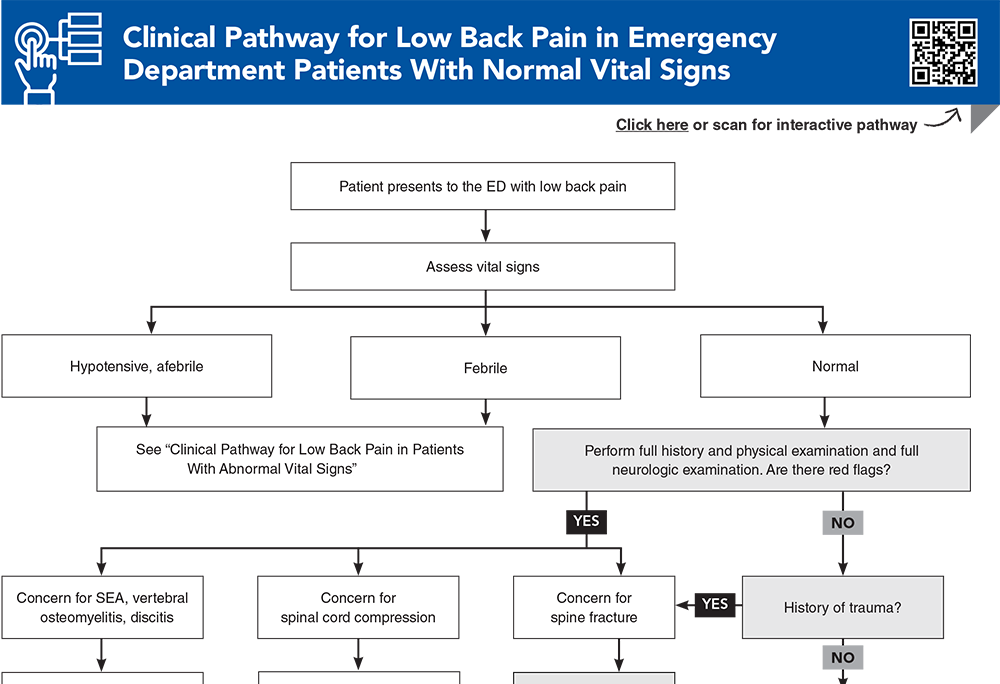
- Clinical Pathway for Low Back Pain in Emergency Department Patients With Normal Vital Signs
- Clinical Pathway for Low Back Pain in Emergency Department Patients With Abnormal Vital Signs
- Tables and Figures
- References
Abstract
Low back pain is a common presentation in the emergency department, and determining whether the cause is benign or life-threatening can be challenging. A systematic strategy for the history and physical examination can help reduce unecessary imaging, and an evidence-based approach will inform safe and effective pain management recommendations. This issue reviews the evidence on red flag signs and symptoms for low back pain, current diagnostic studies recommendations, and best-practice treatment and disposition strategies.
Case Presentations
- She arrives clutching her back and limps to the gurney. She said she has had low back pain before, but it is more severe today.
- Her vital signs are: temperature, 36.7°C; heart rate, 95 beats/min; blood pressure, 161/95 mm Hg; respiratory rate, 22 breaths/min; and oxygen saturation, 98% on room air.
- On examination, you elicit pain, without radiation, with palpation of her right lower back and elevation of her leg. You wonder whether this presentation warrants imaging and how best to treat her pain...
- For 4 days, he has had difficulty controlling his urination. Yesterday, he developed low back pain, and his legs gave out when he got out of bed.
- His vital signs are: temperature, 37.8°C; heart rate, 104 beats/min; blood pressure, 142/87 mm Hg; respiratory rate, 20 breaths/min; and oxygen saturation, 100% on room air.
- On examination, the patient is warm to touch, but he is not in distress. He has midline tenderness to palpation of his lower thoracic spine, and bilateral lower extremity weakness. This presentation is concerning for its “red-flag” findings, but your facility does not have MRI. You wonder how emergent the diagnostic testing needs to be, and how best to expedite management...
- He has a history of low back pain, but it intensified suddenly in a different location. He says he has been a life-long cigarette smoker.
- His vital signs are: temperature, 37°C; heart rate, 124 beats/min; blood pressure, 81/52 mm Hg, respiratory rate, 18 breaths/min; and oxygen saturation, 96% on room air.
- He appears cool, clammy, and diaphoretic, and he is in distress. He has no focal weakness or neurologic findings on examination. This is clearly more than a muscle strain, and you wonder what the best test would be to evaluate the cause of his back pain and hypotension…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Low Back Pain in Emergency Department Patients With Normal Vital Signs
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
20. * Galliker G, Scherer DE, Trippolini MA, et al. Low back pain in the emergency department: prevalence of serious spinal pathologies and diagnostic accuracy of red flags. Am J Med. 2020;133(1):60-72. (Systematic review; 22 studies) DOI: 10.1016/j.amjmed.2019.06.005
25. * Friedman BW, Mulvey L, Davitt M, et al. Predicting 7-day and 3-month functional outcomes after an ED visit for acute nontraumatic low back pain. Am J Emerg Med. 2012;30(9):1852-1859. (Prospective study; 556 patients) DOI: 10.1016/j.ajem.2012.03.027
29. * Dionne N, Adefolarin A, Kunzelman D, et al. What is the diagnostic accuracy of red flags related to cauda equina syndrome (CES), when compared to magnetic resonance imaging (MRI)? A systematic review. Musculoskelet Sci Pract. 2019;42:125-133. (Systematic review; 7 studies) DOI: 10.1016/j.msksp.2019.05.004
46. * Chou R, Fu R, Carrino JA, et al. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. 2009;373(9662):463-472. (Meta-analysis; 7 studies) DOI: 10.1016/S0140-6736(09)60172-0
50. * Downie A, Hancock M, Jenkins H, et al. How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med. 2020;54(11):642-651. (Meta-analysis; 45 studies) DOI: 10.1136/bjsports-2018-100087
70. * van der Gaag WH, Roelofs PD, Enthoven WT, et al. Non-steroidal anti-inflammatory drugs for acute low back pain. Cochrane Database Syst Rev. 2020;4(4):CD013581. (Cochrane review; 32 trials) DOI: 10.1002/14651858.CD013581
78. * Friedman BW, Dym AA, Davitt M, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: a randomized clinical trial. JAMA. 2015;314(15):1572-1580. (Randomized controlled trial; 323 ED patients) DOI: 10.1001/jama.2015.13043
86. * Ashbrook J, Rogdakis N, Callaghan MJ, et al. The therapeutic management of back pain with and without sciatica in the emergency department: a systematic review. Physiotherapy. 2020;109:13-32. (Systematic review; 26 articles) DOI: 10.1016/j.physio.2020.07.005
Subscribe to get the full list of 113 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: herniation, compression, epidural, hematoma, abscess, myelitis, sciatica, immunocompromise, cauda equina, stenosis, skip lesion, opioid, NSAID