

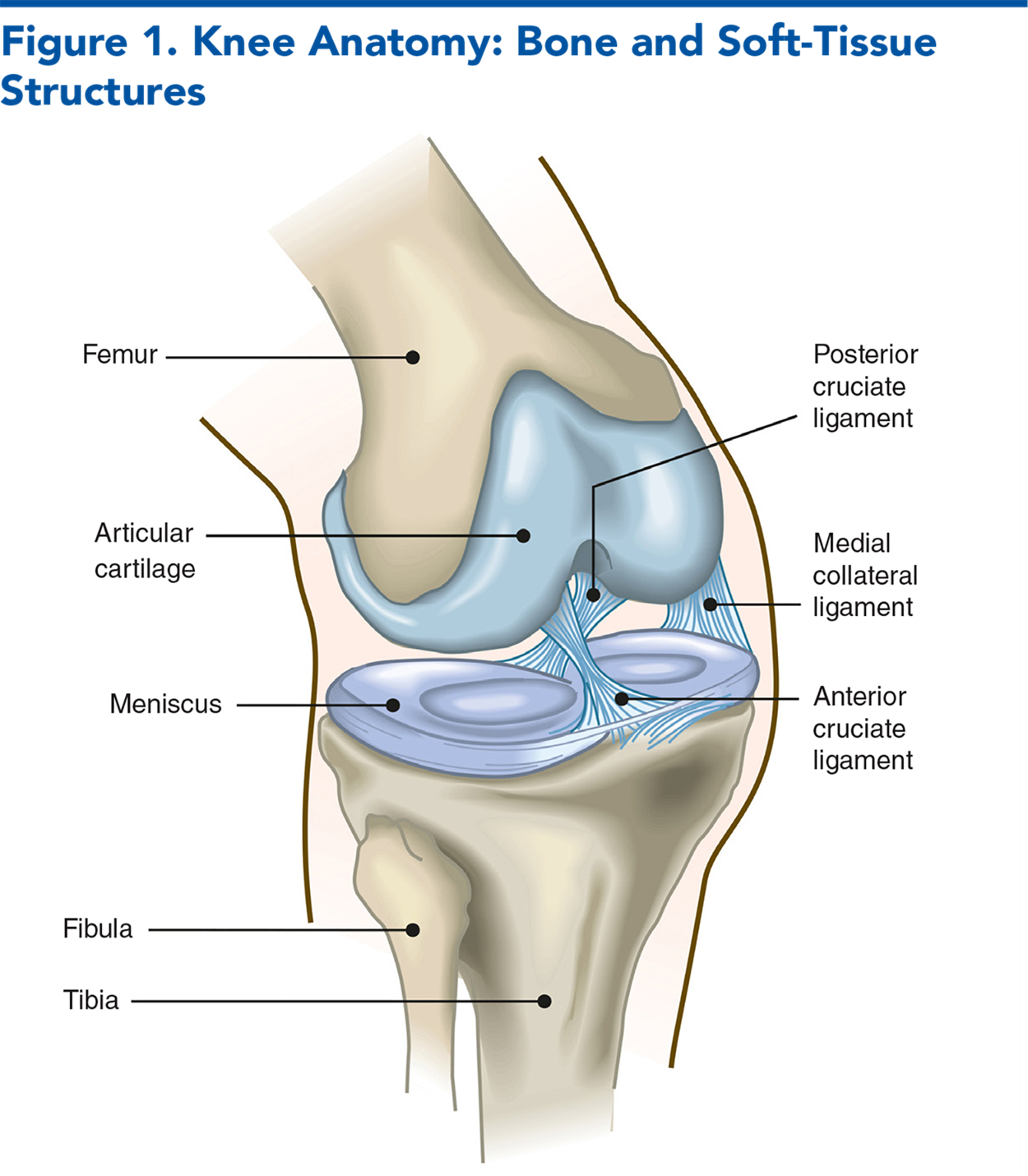
Knee pain is a common presenting complaint in the emergency department, and although the major etiologies are overuse and degenerative, inflammatory and infectious causes must be ruled out. This issue reviews the potential causes of knee pain from the history and physical examination, symptom location-based differential, clinical clues, and special testing strategies. Evidence on the uses of x-ray and ultrasound for diagnostic imaging is reviewed. For suspected infectious causes, procedures for palpation-guided and ultrasound-guided arthrocentesis are outlined. Treatment strategies are summarized, with evidence on the effectiveness of weight loss, physical therapy, orthotics, medication therapies, joint injections, and nerve blocks considered.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
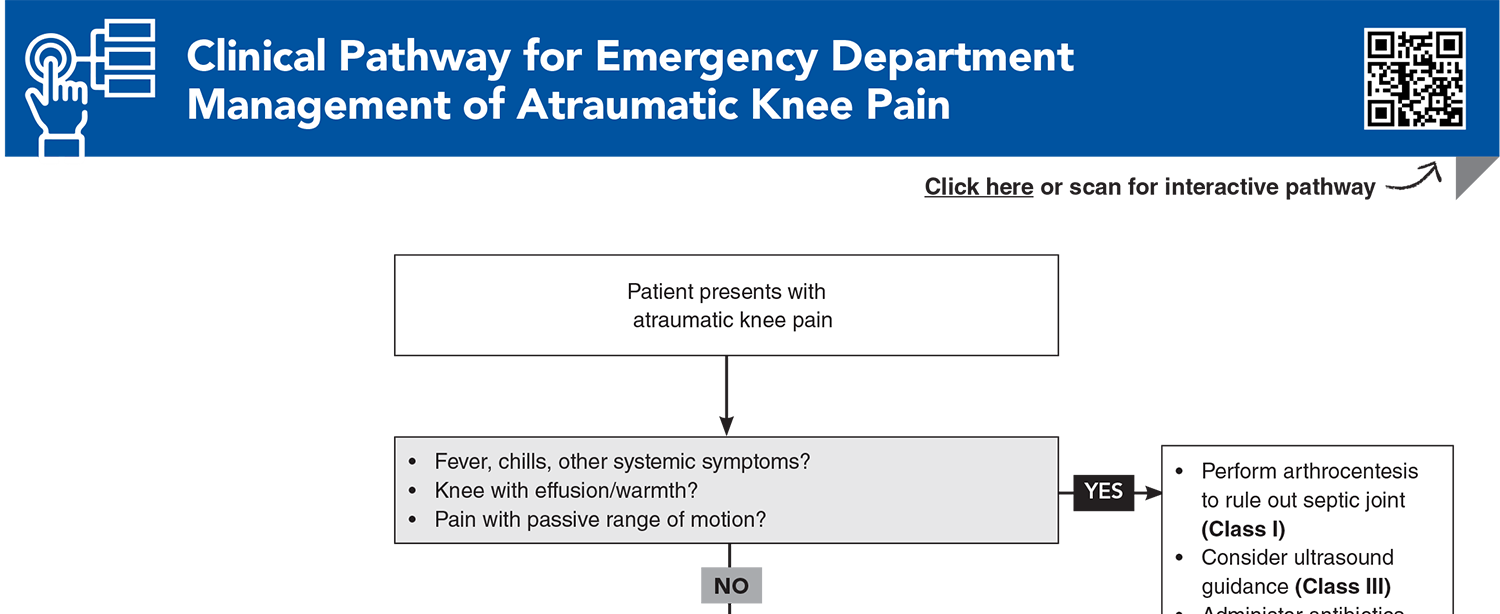
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
5. * Kandemirli GC, Basaran M, Kandemirli S, et al. Assessment of knee osteoarthritis by ultrasonography and its association with knee pain. J Back Musculoskelet Rehabil. 2020;33(4):711-717. (Cross-sectional; 99 patients) DOI: 10.3233/BMR-191504
11. * Helito CP, Teixeira PR, Oliveira PR, et al. Septic arthritis of the knee: clinical and laboratory comparison of groups with different etiologies. Clinics (Sao Paulo). 2016;71(12):715-719. (Retrospective; 105 patients) DOI: 10.6061/clinics/2016(12)07
19. * Kastelein M, Luijsterburg PA, Wagemakers HP, et al. Diagnostic value of history taking and physical examination to assess effusion of the knee in traumatic knee patients in general practice. Arch Phys Med Rehabil. 2009;90(1):82-86. (Prospective, observational cohort studies; 134 patients) DOI: 10.1016/j.apmr.2008.06.027
27. * Sims JI, Chau MT, Davies JR. Diagnostic accuracy of the Ottawa knee rule in adult acute knee injuries: a systematic review and meta-analysis. Eur Radiol. 2020;30(8):4438-4446. (Systematic review and meta-analysis; 8 studies, 7385 patients) DOI: 10.1007/s00330-020-06804-x
29. * Wu TS, Roque PJ, Green J, et al. Bedside ultrasound evaluation of tendon injuries. Am J Emerg Med. 2012;30(8):1617-1621. (Prospective study; 34 patients) DOI: 10.1016/j.ajem.2011.11.004
43. * Sibbitt WL, Jr., Kettwich LG, Band PA, et al. Does ultrasound guidance improve the outcomes of arthrocentesis and corticosteroid injection of the knee? Scand J Rheumatol. 2012;41(1):66-72. (Randomized controlled trial; 64 knees) DOI: 10.3109/03009742.2011.599071
53. * Underwood M, Ashby D, Carnes D, et al. Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study. Health Technol Assess. 2008;12(22):155. (Randomized controlled trial; 585 patients in 26 UK general practices) DOI: 10.3310/hta12220
59. * Toupin April K, Bisaillon J, Welch V, et al. Tramadol for osteoarthritis. Cochrane Database Syst Rev. 2019;5(5):CD005522. (Cochrane review; 22 trials, 6496 patients) DOI: 10.1002/14651858.CD005522.pub3
70. * Chughtai M, Elmallah RD, Mistry JB, et al. Nonpharmacologic pain management and muscle strengthening following total knee arthroplasty. J Knee Surg. 2016;29(3):194-200. (Review) DOI: 10.1055/s-0035-1569147
76. * McAlindon TE, LaValley MP, Harvey WF, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. JAMA. 2017;317(19):1967-1975. (Randomized placebo-controlled double-blind trial; 140 patients) DOI: 10.1001/jama.2017.5283
Subscribe to get the full list of 82 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: arthritis, osteoarthritis, ligament, tendon, patella, meniscus, septic, prosthesis, effusion, dislocation, quadriceps, ROM, Ottawa, ultrasound, arthrocentesis, immobilizer
Vanica Guignard, MD; John Kiel, DO, MPH, FACEP, CAQSM; Diego Riveros, MD
Daniel Eraso, MD, FACEP; Michael P. Jones, MD; John Munyak, MD
March 1, 2025
March 1, 2028 CME Information
4 AMA PRA Category 1 Credits™, 4 ACEP Category I Credits, 4 AAFP Prescribed Credits, 4 AOA Category 2-B Credits.