Table of Contents
About This Issue
Hand and wrist injuries are common in the ED, from strains, sprains, and fractures to lacerations, amputations, and injection and crush injuries. Most emergencies can be managed safely in the ED, although in many cases, prompt referral and follow-up will help avoid serious sequelae, such as stiffness, deformity, amputation, and loss of function. In this issue, you will learn:
How to differentiate between surgical emergencies and injuries that are appropriate for ED management.
How to identify limb-threatening injuries, including compartment syndrome, high-pressure injections, and vascular compromise.
When hand consult is needed – urgent, emergent, or follow-up.
X-ray, ultrasound, CT, or MRI? Indications for each diagnostic strategy.
Recommendations for managing fingertip amputations by zone.
Diagnosing and treating injuries of tendons and ligaments: proper imaging, splinting, and follow-up.
How to manage fractures, dislocations, and dissociations of the wrist and hand to avoid long-term disability.
How to avoid pitfalls in managing patients with neurovascular injuries, high-pressure injection injuries, and acute compartment syndrome.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- Triage and Stabilization
- History
- Physical Examination
- The Hand Examination
- Diagnostic Studies
- Imaging
- Treatment
- Fundamentals of Treatment
- Pain Control
- Hemostasis
- Wound Management
- Splinting
- Skin and Soft Tissue Injuries
- Laceration
- Fight Bite
- Finger Amputation
- Nail Bed Injury
- Tendon Injury
- Diagnosis
- Strain
- Flexor Tendon Injury
- Extensor Tendon Injury
- Ligament Injury
- Sprains
- Carpal Instability
- Perilunate and Lunate Injuries
- Scapholunate Dissociation
- Dislocations
- Carpometacarpal Joint Dislocation
- Metacarpophalangeal Joint Dislocation
- Proximal Interphalangeal Joint Dislocation
- Fractures
- Phalanx Fractures
- Thumb Fractures
- Metacarpal Fractures
- Metacarpal Shaft Fractures
- Metacarpal Base and Head Fractures
- Metacarpal Neck Fractures
- Carpal Fractures
- Scaphoid Fractures
- Non–Scaphoid Carpal Fractures
- Nerve Injuries
- High-Pressure Injection Injuries
- Compartment Syndrome
- Controversies and Cutting Edge
- Management of Open Hand and Finger Fractures
- Disposition
- Summary
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Managing Hand Injuries in the Emergency Department
- Case Conclusions
- Time- and Cost-Effective Strategies
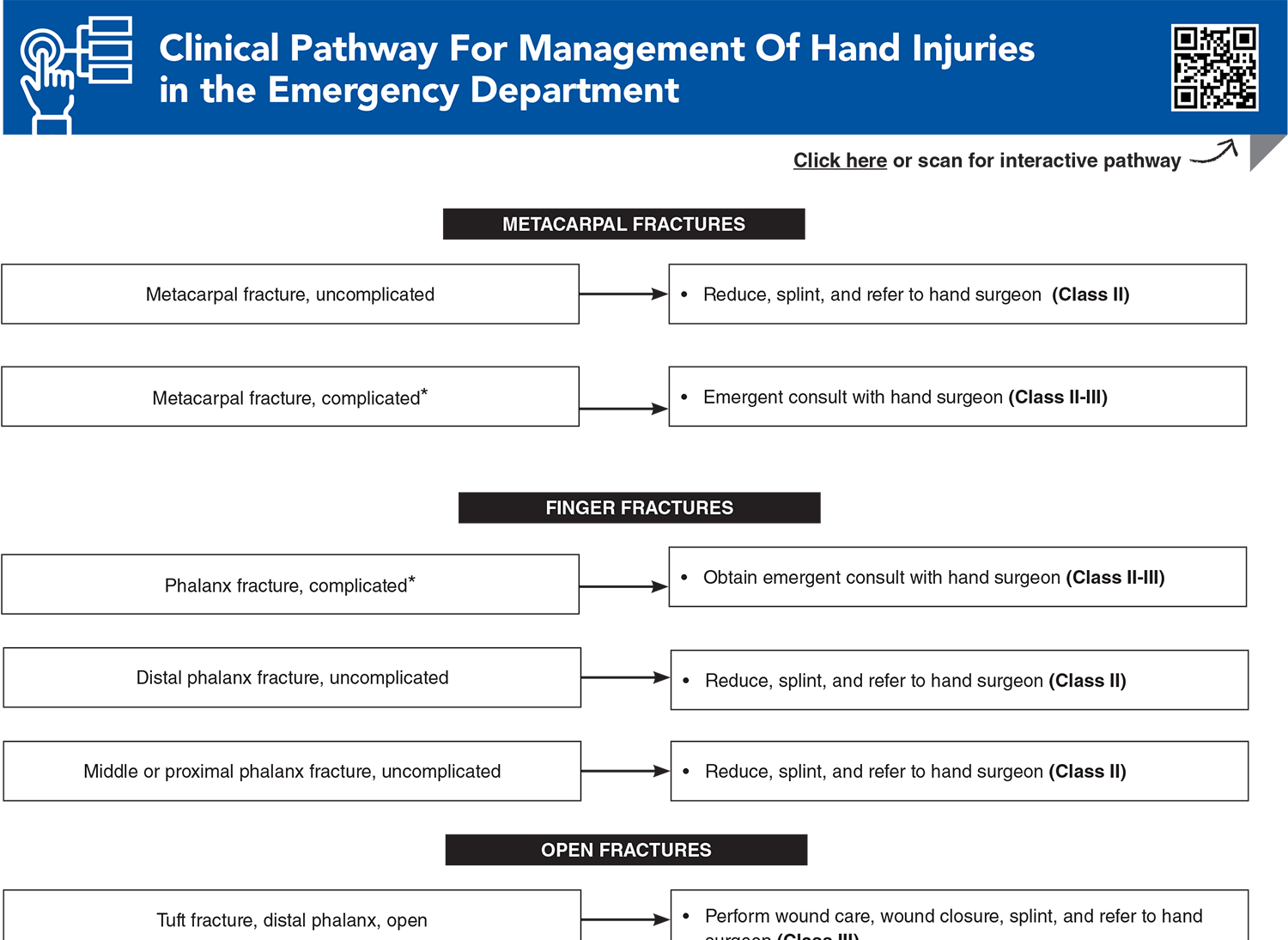
- Clinical Pathway For Management Of Hand Injuries in the Emergency Department
- Tables and Figures
- References
Abstract
Injuries of the hand and wrist are commonly encountered in the emergency department. Though they are rarely life-threatening, there is potential for significant patient pain, morbidity, and long-term functional loss if they are not treated appropriately. A thorough and focused examination and plain radiographs are sufficient to diagnose most hand injuries, with outpatient referral to a hand specialist when indicated. Clinicians must be able to identify the life- or limb-threatening hand injuries that can present, both in treating and facilitating urgent hand consultation. This review provides a best-practice update on the evaluation and treatment of common hand and wrist emergencies.
Case Presentations
- His vital signs are all normal, but he seems to be in some pain. He says he is right-hand dominant.
- Upon examination, the patient’s wrist is tender and swollen but neurovascularly intact. You order x-rays of the right wrist, including a scaphoid view.
- He is asking whether he can play football again next week…
- You note that the patient has a small wound over the volar index finger. He is right-hand dominant.
- His vital signs are normal, but he is in extreme pain. Despite the wound appearing to be very small, he is having difficulty moving the finger.
- Considering the mechanism of injury, you obtain a 3-view x-ray of the hand to determine next steps...
- He says he suffered a table saw injury to the left index finger proximal phalanx approximately 90 minutes ago. The finger is completely amputated. The finger is present in the room, wrapped in saline-soaked gauze, on ice.
- The patient says he has a history of hypertension and a 1-pack-per-day smoking habit. He is right-hand dominant.
- You obtain a 3-view x-ray study of the hand and the amputated part and initiate a consult with the hand service. While awaiting consultation, you consider the indications and contraindications for replantation...
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway For Management Of Hand Injuries in the Emergency Department
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
11. * Wieschhoff GG, Sheehan SE, Wortman JR, et al. Traumatic finger injuries: what the orthopedic surgeon wants to know. Radiographics. 2016;36(4):1106-1128. (Review) DOI: 10.1148/rg.2016150216
32. * Boyd AS, Benjamin HJ, Asplund C. Splints and casts: indications and methods. Am Fam Physician. 2009;80(5):491-499. (Review)
57. * Lutsky KF, Giang EL, Matzon JL. Flexor tendon injury, repair and rehabilitation. Orthop Clin North Am. 2015;46(1):67-76. (Review) DOI: 10.1016/j.ocl.2014.09.004
70. * Miller EA, Friedrich JB. Management of finger joint dislocation and fracture-dislocations in athletes. Clin Sports Med. 2020;39(2):423-442. (Review) DOI: 10.1016/j.csm.2019.10.006
73. * Hawken JB, Giladi AM. Primary management of nail bed and fingertip injuries in the emergency department. Hand Clin. 2021;37(1):1-10. (Review) DOI: 10.1016/j.hcl.2020.09.001
99. * Ketonis C, Dwyer J, Ilyas AM. Timing of debridement and infection rates in open fractures of the hand: a systematic review. Hand (N Y). 2017;12(2):119-126. (Systematic review; 12 articles) DOI: 10.1177/1558944716643294
Subscribe to get the full list of 101 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: fracture, dislocation, dissociation, amputation, injection, nerve, radial, ulnar, compartment, splint, flexor, mallet, sprain, gamekeeper, carpal, lunate, Seymour