

Headaches are a common reason for pediatric visits to the emergency department. Emergency clinicians must distinguish between common and dangerous secondary causes of headache and primary headache disorders such as migraine and tension-type headaches. This issue discusses the diagnosis of primary headaches by history and physical examination, the options for first-line treatment of primary headache and for severe or refractory migraines, and procedural interventions that may be considered when other therapies have failed. Guidance is provided for patient and family education regarding triggers, lifestyle modifications, and nutraceutical prophylaxis.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
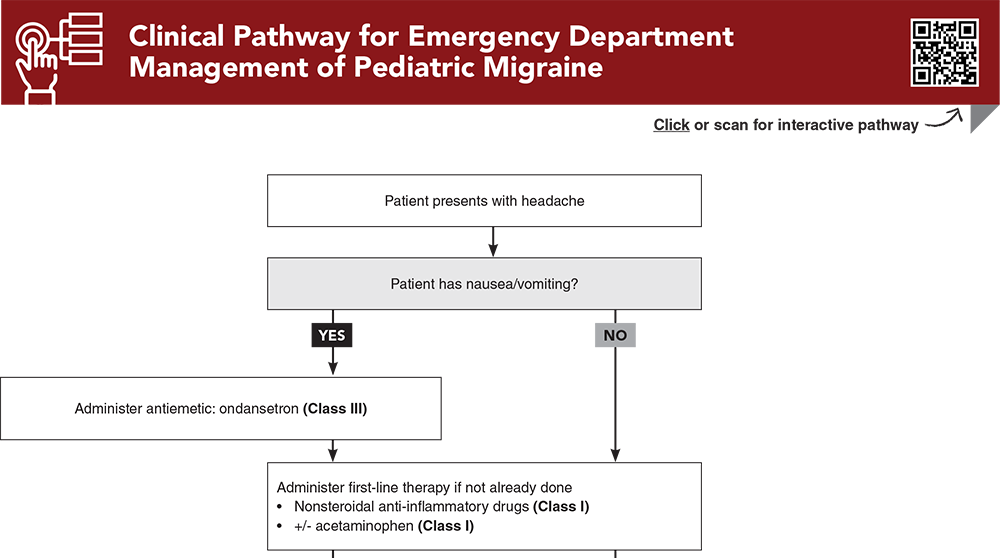
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
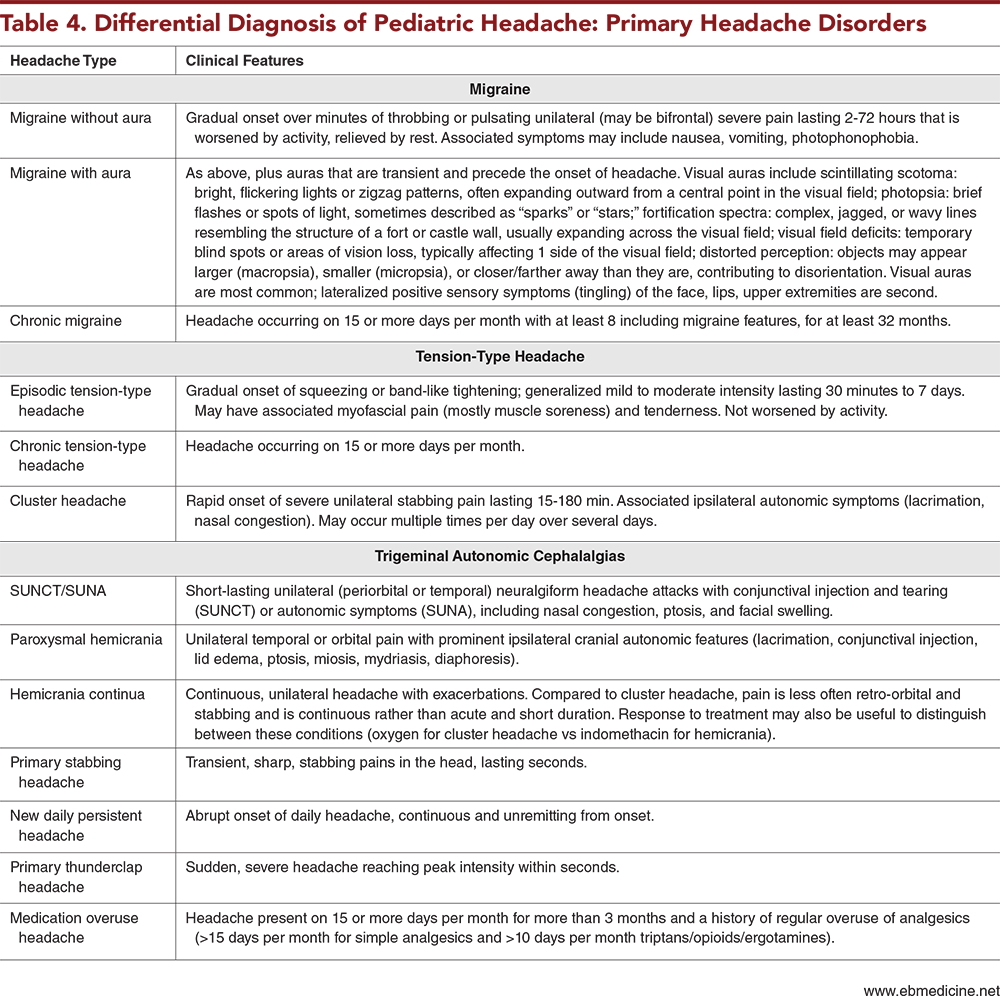
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
3. * Irwin SL, Greene KA, Pavitt SJ, et al. Headache in the pediatric population: focus on migraine. Semin Neurol. 2022;42(4):479-488. (Review) DOI: 10.1055/s-0042-1757927
4. * Raucci U, Della Vecchia N, Ossella C, et al. Management of childhood headache in the emergency department. Review of the literature. Front Neurol. 2019;10:886. (Review) DOI: 10.3389/fneur.2019.00886
6. * Camargo A, Kanekar S. Neuroimaging in pediatric headache. Neurol Clin. 2022;40(3):679-698. (Review) DOI: 10.1016/j.ncl.2022.02.007
14. * Oskoui M, Pringsheim T, Holler-Managan Y, et al. Practice guideline update summary: acute treatment of migraine in children and adolescents: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Headache Society. Headache. 2019;59(8):1158-1173. (Practice guideline) DOI: 10.1111/head.13628
17. * Lewis DW, Ashwal S, Dahl G, et al. Practice parameter: evaluation of children and adolescents with recurrent headaches: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2002;59(4):490-498. (Practice guideline) DOI: 10.1212/wnl.59.4.490
26. * Vuralli D, Ozge A, Bolay H. Pediatric headache. In: Togha M, Jafari E, Mohammadianinejad SE, et al, eds. Headache and Migraine in Practice: Academic Press; 2022:239-263. (Book chapter) ISBN: 9780323997294
27. * Ghosh A, Silva E, Burish MJ. Pediatric-onset trigeminal autonomic cephalalgias: a systematic review and meta-analysis. Cephalalgia. 2021;41(13):1382-1395. (Systematic review and meta-analysis; 86 studies) DOI: 10.1177/03331024211027560
30. * Baglioni V, Orecchio S, Esposito D, et al. Tension-type headache in children and adolescents. Life (Basel). 2023;13(3). (Review) DOI: 10.3390/life13030825
38. * Cortel-LeBlanc MA, Orr SL, Dunn M, et al. Managing and preventing migraine in the emergency department: a review. Ann Emerg Med. 2023;82(6):732-751. (Review) DOI: 10.1016/j.annemergmed.2023.05.024
50. * Tsze DS, Ochs JB, Gonzalez AE, et al. Red flag findings in children with headaches: prevalence and association with emergency department neuroimaging. Cephalalgia. 2019;39(2):185-196. (Prospective cohort; 224 patients) DOI: 10.1177/0333102418781814
Subscribe to get the full list of 123 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: primary headache, serious secondary headaches, red-flag symptoms, migraine, migraine with aura, migraine without aura, pediatric migraine, cluster headache, trigeminal autonomic cephalalgias, recurrent headaches, tension-type headache, headache history, headache characteristics, triptans, dopamine antagonists, ergotamine, nerve blocks, trigger point injections, ketamine, calcitonin gene-related peptide-related therapies, CGRP, nutraceuticals
Lujain F. Abul, MD; Aidan McParland, MD, MSc; Garth D. Meckler, MD, MSHS
Sujit Iyer, MD; Emily Rose, MD, FAAP, FAAEM, FACEP
January 1, 2025
January 1, 2028 CME Information
4 AMA PRA Category 1 Credits™, 4 ACEP Category I Credits, 4 AAP Prescribed Credits, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 2 Pain Management credits and 2 Pharmacology CME credits, subject to your state and institutional approval.