Table of Contents
About This Issue
Urgent care clinics and clinicians are vital to improving the rates of HIV diagnosis, treatment, and prevention in the United States. Clinicians working in urgent care settings should be familiar with the latest guidelines for HIV screening, pre- and postexposure prophylaxis, and treatment. In this issue, you will learn:
The current guidelines for initiating HIV post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP) in the urgent care clinic.
Common adverse effects associated with antiretroviral drugs used to treat HIV.
How to approach the differential diagnosis for patients with HIV who present with new symptoms.
Best practices for screening and diagnosing new HIV infections in the urgent care setting.
Management strategies for patients with suppressed viral loads as well as those with untreated HIV.
The importance of re-engaging and reconnecting out-of-care persons with HIV to proper medical care.
How to handle urgent care cases involving potential HIV exposure, including occupational and nonoccupational scenarios.
CODING & CHARTING: Coding for encounters with patients who have HIV or who have known or suspected exposure to HIV can be complex. Learn more in our monthly coding column.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Epidemiology and Pathophysiology
- The National HIV Epidemic
- The Ending the HIV Epidemic in the United States Initiative
- Special Populations
- Transmission of HIV
- Differential Diagnosis
- Urgent Care Evaluation
- Universal HIV Screening
- History
- New Diagnosis
- Person with HIV with New Complaints
- Physical Examination
- HIV Prevention
- HIV Pre-exposure Prophylaxis
- HIV Postexposure Prophylaxis
- HIV Treatment as Prevention
- Nonpharmacologic HIV Prevention
- Diagnostic Testing
- Laboratory Testing
- Imaging
- Diagnosis of HIV and the Course of Disease
- Treatment
- Current Recommendations for HIV Treatment
- Current Recommendations for HIV Postexposure Prophylaxis
- Current Recommendations for HIV Pre-exposure Prophylaxis
- Adverse Effects of HIV Medications
- Single-Pill Regimens
- Hepatitis B Virus Reactivation
- Drug-Drug Interactions
- Special Circumstances
- Substance Use Disorders and HIV
- New Diagnosis of HIV
- Underinsured or Uninsured Patients
- Cutting Edge
- Risk Management Pitfalls for Managing Patients With HIV in the Urgent Care Setting
- Summary
- 5 Things That Will Change Your Practice
- Case Conclusions
- Coding & Charting: What You Need to Know
- Number and Complexity of Problems Addressed
- Amount and/or Complexity of Data to be Reviewed and Analyzed
- Risk of Complications and/or Morbidity or Mortality of Patient Management
- Coding Challenge
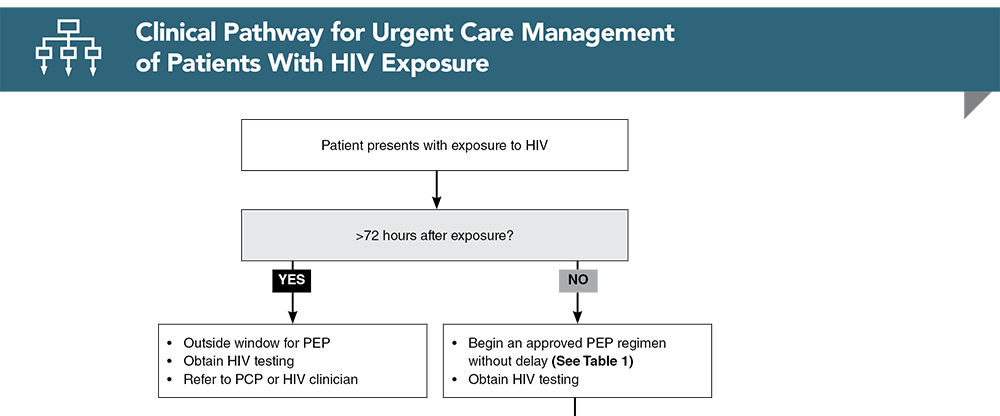
- Clinical Pathway for Urgent Care Management of Patients With HIV Exposure
- References
Abstract
With appropriate care and antiretroviral therapy, persons with HIV can achieve undetectable viral loads, resulting in the virtual elimination of opportunistic infection risk, an improved quality of life, and a normal life expectancy. The optimal urgent care management of persons with HIV includes the diagnosis of new cases, the prevention of HIV acquisition, and the provision of services for re-engagement and reconnection of out-of-care persons with HIV back to the care of an HIV clinician. This issue of Evidence-Based Urgent Care reviews the role of urgent care clinics and clinicians in preventing, screening for, and diagnosing new HIV infections. The urgent care management of persons with HIV is also discussed, including patients who have suppressed viral loads and patients with untreated HIV.
Case Presentations
- The patient states that he has well-controlled HIV and says his last CD4 count a few weeks ago was 550 cells/mcL.
- You wonder how to approach diagnosis and treatment for his respiratory infection in the setting of his HIV disease...
- She says she has had up to 3 episodes of diarrhea a day for the past 3 weeks.
- She denies pain, melena, rectal bleeding, and fever. Her laboratory test results are unremarkable.
- You wonder whether additional testing is needed and whether sending her home is appropriate…
- He reports engaging in condomless vaginal intercourse with a partner with unknown HIV status 12 hours earlier.
- In addition to being evaluated for STIs, he wants to make sure he does not contract HIV.
- You wonder if HIV PEP is indicated for this patient…
- She describes having fevers to 101°F, swollen lymph nodes, and diffuse maculopapular rash. Several of her friends are ill with upper respiratory viral infections and she wonders if this is the same illness.
- She is sexually active but denies any known history of STIs.
- You consider the differential and testing options for this patient…
- He reports having unprotected receptive anal intercourse 9 days ago with a partner who has HIV.
- You consider what testing and treatment are indicated…
- He reports having unprotected receptive anal intercourse 2 days ago with a person who he subsequently learned has HIV.
- In addition to HIV and STI testing, you wonder what other care should be offered to this patient...
- He is a housekeeper at a local hotel. He reports that about 1 hour ago, he was removing trash from a guest room and was stuck with a needle that was in the trash receptacle.
- He does not know if the needle had blood on it. The guest who had been staying in the room had already checked out of the hotel when the injury occurred.
- On examination, the wound is deep with active bleeding.
- You consider whether any care is needed in this situation beyond the immediate treatment of the bleeding wound…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Urgent Care Management of Patients With HIV Exposure
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * United States Centers for Disease Control and Prevention. Fast Facts: HIV in the United States. Accessed May 10, 2024. (CDC statistics)
2. * United States Centers for Disease Control and Prevention. About Ending the HIV Epidemic in the US. Updated Match 20, 2024. Accessed May 10, 2024. (CDC initiative)
14. * United States Department of Health & Human Services National Institutes of Health. The science is clear: with HIV, undetectable equals untransmittable. Published January 10, 2019. Accessed May 10, 2024. (News release)
15. * Eisinger RW, Dieffenbach CW, Fauci AS. HIV viral load and transmissibility of HIV infection: undetectable equals untransmittable. JAMA. 2019;321(5):451-452. (Review) DOI: 10.1001/jama.2018.21167
18. * United States Centers for Disease Control and Prevention. Status Neutral HIV Prevention and Care. Last reviewed March 1, 2023. Accessed May 10, 2024. (CDC guidance)
30. * United States Centers for Disease Control and Prevention. Preexposure Prophylaxis for the Prevention of HIV infection in the United States—2021 Update: A Clinical Practice Guideline. Published March 2018. Accessed May 10, 2024. (CDC guidelines)
33. * United States Department of Health & Human Services National Institutes of Health. Post-Exposure Prophylaxis (PEP): Key Points. Updated February 6, 2024. Accessed May 10, 2024. (NIH guidelines)
41. * United States Department of Health and Human Services.Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Updated June 10, 2021. Accessed May 10, 2024. (Guidelines)
Subscribe to get the full list of 51 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: HIV, AIDS, PEP, PREP, pre-exposure, postexposure, prophylaxis, HAART, antiretroviral, CD4, PEP, PrEP, seroconversion, opportunistic infection, HIV testing, HIV screening