Table of Contents
About This Issue
Depending on the stage of disease, syphilis can present as a single chancre in an apparently well patient (primary syphilis), all the way to cardiac disease, meningitis, general paresis, stroke, seizures, and mental health symptoms of tertiary syphilis. Because syphilis can present in so many different ways, with latent periods, and symptoms that mimic many benign conditions, it is imperative to identify and properly treat patients to halt its devastating consequences, including congenital syphilis. In this issue, you will learn:
The most common symptoms of each stage of the disease: primary, secondary, tertiary, latent, and congenital syphilis.
How other sexually transmitted infections and HIV can increase the likelihood of syphilis infection – and vice versa.
What the most relevant details of the history can tell you about the likelihood of syphilis and the need for testing.
RPR/VDRL/treponemal/nontreponemal/TP-PA testing: what the testing regimens are and when they should be used, including the reverse-testing protocol.
The first-line treatment regimen (penicillin G benzathine) and the alternative drug regimens that can be used when this drug is in short supply.
The critical needs of pregnant patients who present without prenatal care or are in high-risk groups, to prevent life-threatening congenital syphilis.
When patients can be discharged home and when they need to be admitted for treatment.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Epidemiology
- Etiology and Pathophysiology
- Primary Syphilis
- Secondary Syphilis
- Tertiary Syphilis
- Latent Syphilis
- Neurosyphilis
- Congenital Syphilis
- Ocular Syphilis
- Otosyphilis
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Primary Syphilis on Examination
- Secondary Syphilis on Examination
- Tertiary Syphilis on Examination
- Diagnostic Studies
- Reverse-Testing Protocol
- Nontreponemal Testing
- Testing for Patients With Previous Infections
- Treponemal Testing
- Point-of-Care Testing
- Dark-Field Microscopy
- Testing for Neurosyphilis, Ocular Syphilis, and Otosyphilis
- Treatment
- Treatment Development
- Current Treatment
- First-Line Regimens
- Second-Line Regimens
- Treatment of Sex Partners
- Jarisch-Herxheimer Reaction
- Prevention and Counseling
- Controversies
- The Tuskegee Study
- Cutting Edge
- Alternative Treatment Regimens Under Study
- Postexposure Prophylaxis
- Vaccine Development
- Disposition
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Diagnosing and Treating Emergency Department Patients With Syphilis
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
- Clinical Pathways
- Clinical Pathway for Emergency Department Triage and Testing for Syphilis
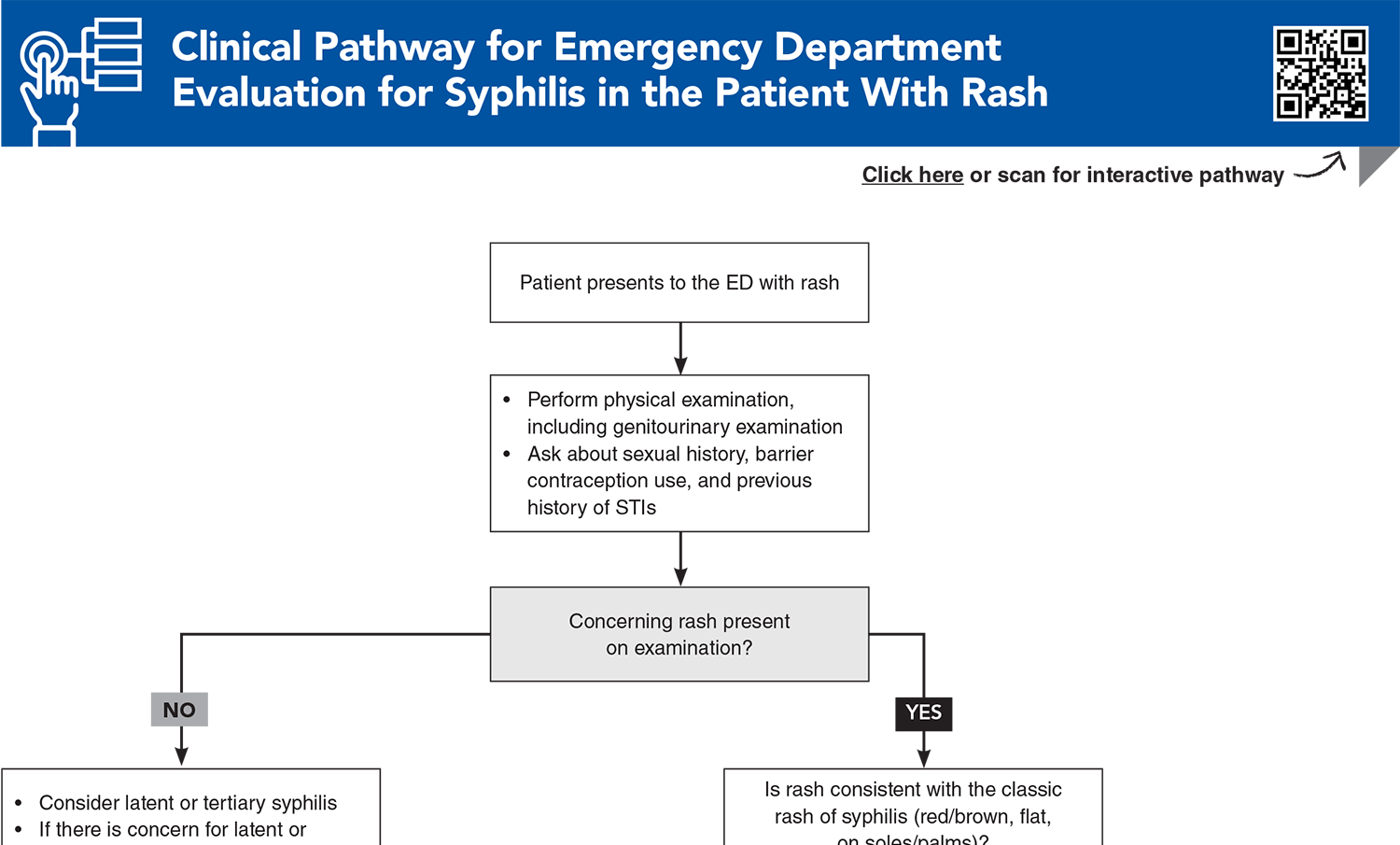
- Clinical Pathway for Emergency Department Evaluation for Syphilis in the Patient With Rash
- Tables and Figures
- References
Abstract
Syphilis is a sexually transmitted infection known as the “great imitator” due to its large variety of presentations, depending on the stage of the disease. Because of its prevalence and the possibility of severe outcomes, emergency clinicians must remain vigilant when evaluating patients, especially those in high-risk groups. Clinicians should be familiar with the treatment recommendations for the various stages of syphilis, including alternative regimens, when national drug shortages limit the availability of first-line treatments. This review discusses the various presentations, diagnostic options, and potential complications for syphilis, as well as current and emerging treatment recommendations.
Case Presentations
- He reports no symptoms at this time, but says he was treated for primary syphilis 2 years ago.
- He is sexually active with both men and women, intermittently uses condoms, and takes pre-exposure prophylaxis (PrEP) for HIV. He presented for testing due to concerns about STI exposure from a sexual partner.
- As the patient asks, “Do I have syphilis again?” you consider whether you should order additional testing or treat him for active infection…
- She said said she just had her pregnancy confirmed at a local women’s clinic and is at 25 weeks’ gestation with her first baby, but she has not yet had any prenatal testing.
- She reports a recent upper respiratory infection, after which she developed a diffuse rash 2 days ago. The rash is on her trunk, arms, legs, and neck. The lesions are small, oval-shaped, and pink in color. There is no involvement of her palms and soles.
- She is sexually active with the baby’s father and does not use condoms.
- She reports a childhood allergy to penicillin but does not know what reaction she had.
- You consider whether you should treat this patient empirically for syphilis, and what antibiotics you would give her…
- Her family reports that she has seemed moody and sometimes agitated.
- She recently retired from her job, has been more irritable with friends and family, and has been complaining of memory problems and “brain fog.”
- On examination, she is alert and oriented to person, place, and time, but is slow to respond to questions. Her vital signs are normal, and she does not have any focal neurological complaints.
- You consider ordering an RPR test, even though she denies being sexually active…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Evaluation for Syphilis in the Patient With Rash
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * New York City Department of Health and Mental Hygiene. The diagnosis, management, and prevention of syphilis: an update and review. 2019. Accessed December 10, 2025. (Review)
3. * Eppes CS, Stafford I, Rac M. Syphilis in pregnancy: an ongoing public health threat. Am J Obstet Gynecol. 2022;227(6):822-838. (Review) DOI: 10.1016/j.ajog.2022.07.041
5. * Hazra A, Collison MW, Davis AM. CDC sexually transmitted infections treatment guidelines, 2021. JAMA. 2022;327(9):870-871. (Guidelines) DOI: 10.1001/jama.2022.1246
9. * Ren M, Dashwood T, Walmsley S. The intersection of HIV and syphilis: update on the key considerations in testing and management. Curr HIV/AIDS Rep. 2021;18(4):280-288. (Review) DOI: 10.1007/s11904-021-00564-z
19. * Thean L, Moore A, Nourse C. New trends in congenital syphilis: epidemiology, testing in pregnancy, and management. Curr Opin Infect Dis. 2022;35(5):452-460. (Review) DOI: 10.1097/QCO.0000000000000875
22. * Wan Z, Zhang H, Xu H, et al. Maternal syphilis treatment and pregnancy outcomes: a retrospective study in Jiangxi Province, China. BMC Pregnancy Childbirth. 2020;20(1):648. (Analysis of Chinese database; 4210 women) DOI: 10.1186/s12884-020-03314-y
24. * Guidance for STD clinical preventive services for persons infected with HIV. Sex Transm Dis. 2001;28(8):460-463. (Committee recommendations) DOI: 10.1097/00007435-200108000-00007
30. * Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2014;312(18):1905-1917. (Systematic review; 102 articles) DOI: 10.1001/jama.2014.13259
Subscribe to get the full list of 43 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: STI, RPR, VDRL, neurosyphilis, congenital, primary, secondary, tertiary, latent, chancre, rash, treponemal, nontreponemal, penicillin, benzathine, benzylpenicillin, PrEP, HIV