Table of Contents
About This Issue
Most causes of scrotal pain are benign, but testicular torsion is a true urologic emergency that must be considered in all cases. Delays in time to detorsion are common, leading to suboptimal outcomes. Systems should be implemented to avoid delays in evaluation, ultrasound confirmation of the diagnosis, and coordination of emergent surgical intervention. This issue reviews common causes of acute scrotal pain in pediatric patients. The literature is reviewed, and recommendations are provided to guide the emergency clinician in appropriate management and disposition of boys with acute scrotal pain. In this issue, you will learn:
The pathophysiology of various types of testicular torsion, including deformities that increase the risk for testicular torsion
Sequelae of testicular torsion
Conditions in the differential diagnosis of acute scrotal pain in pediatric patient
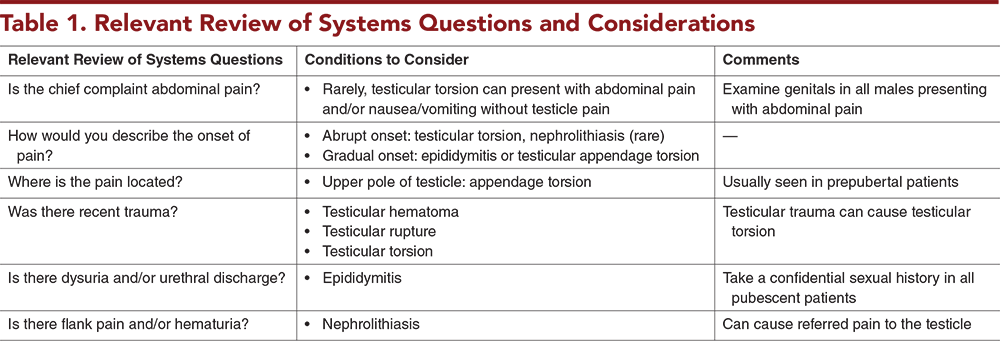
Relevant review of systems questions that should be asked while taking the history
Key aspects of the physical examination that will help determine the cause of pain
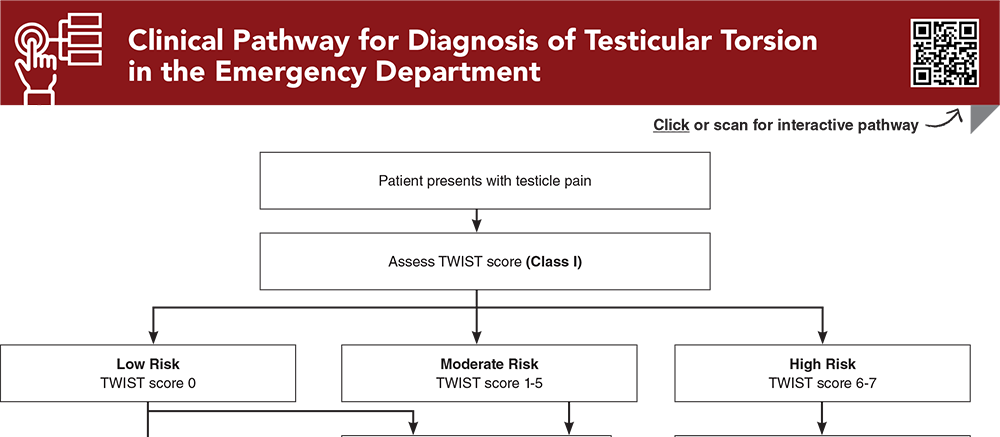
How to use the TWIST score to assess the likelihood of testicular torsion in patients with scrotal pain
Pearls and pitfalls of point-of-care ultrasound for the evaluation of acute scrotal pain
Recommendations for manual detorsion in the emergency department
Considerations for special populations including children with cryptorchidism and those with cerebral palsy
Recommendations for disposition of patients for whom testicular torsion has been ruled out, those who have undergone surgical exploration, and those with confirmed cases of torsion on ultrasound
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Epidemiology and Pathophysiology
- Epidemiology
- Pathophysiology
- Intravaginal Torsion
- Extravaginal Torsion
- Timing and Hypoxia
- Sequelae of Testicular Torsion
- Endocrine Function
- Fertility
- Differential Diagnosis
- Testicular Appendage Torsion
- Acute Epididymitis
- Inguinal Hernia
- Varicoceles
- Hydroceles
- Extra-Testicular Causes
- Less-Common Causes
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Testicular Workup for Ischemia and Suspected Torsion (TWIST) Score
- Ultrasound
- Technique and General Considerations
- Point-of-Care Ultrasound
- Color Doppler Ultrasound
- The Whirlpool Sign
- Treatment
- Manual Detorsion in the Emergency Department
- Operative Management
- Special Populations
- Children With Cryptorchidism
- Children With Cerebral Palsy
- Controversies and Cutting Edge
- Disposition
- Summary
- Risk Management Pitfalls for Management of Patients With Acute Scrotal Pain
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- Case Conclusions
- Clinical Pathway for Diagnosis of Testicular Torsion in the Emergency Department
- Tables and Figures
- References
Abstract
Testicular torsion is a urologic emergency, accounting for up to 15% of cases of acute scrotal pain. Rapid recognition and management are essential to ensure viability of the testis. Doppler ultrasound can be used to confirm the diagnosis of testicular torsion; however, recent studies suggest that a more judicious use of ultrasound may be safe, decrease delays in surgical management, and avoid unnecessary utilization of resources. This issue reviews the epidemiology and historical and physical examination findings of testicular torsion and other common causes of acute scrotal pain. The existing literature is reviewed and recommendations are provided to guide the emergency clinician in appropriate management and disposition of boys with acute scrotal pain.
Case Presentations
- The boy has no fever, dysuria, or hematuria. He is not sexually active and denies trauma. He has vomited twice.
- On examination, the boy appears uncomfortable and rates his pain as 9/10. His abdomen is soft, with mild lower left quadrant tenderness. A testicular examination is notable for a swollen, erythematous, high-riding left testicle that feels indurated compared to the right testicle. You cannot elicit a cremasteric reflex on either the right or the left.
- You begin to consider your management priorities…
- The boy denies fever, nausea, vomiting, dysuria, or penile discharge. He rates his pain as 8/10, and he looks very uncomfortable.
- You are able to elicit a cremasteric reflex on the left. His left scrotum is swollen, erythematous, and tender to palpation. The testicle is not hard or high-riding. You are very suspicious for testicular torsion and are surprised that there is a cremasteric reflex present.
- You wonder how reliable this reflex is in ruling testicular torsion in or out. You consider the utility of manual detorsion in this patient and whether ultrasound should be obtained first…
- There is no history of trauma. The patient reports his pain is 4/10 and worse with walking. The boy’s mother says he has been walking “funny.” The boy denies nausea or vomiting.
- A cremasteric reflex is positive bilaterally. The right hemiscrotum is normal, with no redness or swelling. The testicle is not hard or high-riding, and there is mild tenderness to palpation. The boy does not appear uncomfortable.
- The TWIST score for this child is 0. You wonder how often testicular torsion occurs in prepubertal boys. You do not have ultrasound staff available at this time of night, and you consider whether an ultrasound is always necessary to rule out torsion, especially when the TWIST score is 0...
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Diagnosis of Testicular Torsion in the Emergency Department
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
6. * Mori T, Ihara T, Nomura O. Diagnostic accuracy of point-of-care ultrasound for paediatric testicular torsion: a systematic review and meta-analysis. Emerg Med J. 2023;40(2):140-146. (Systematic review and meta-analysis; 4 studies, 784 patients) DOI: 10.1136/emermed-2021-212281
12. * Dias Filho AC, Oliveira Rodrigues R, Riccetto CL, et al. Improving organ salvage in testicular torsion: comparative study of patients undergoing vs not undergoing preoperative manual detorsion. J Urol. 2017;197(3 Pt 1):811-817. (Retrospective; 133 patients) DOI: 10.1016/j.juro.2016.09.087
26. * Gielchinsky I, Suraqui E, Hidas G, et al. Pregnancy rates after testicular torsion. J Urol. 2016;196(3):852-855. (Retrospective observational; 63 patients) DOI: 10.1016/j.juro.2016.04.066
29. * Santillanes G, Gausche-Hill M, Lewis RJ. Are antibiotics necessary for pediatric epididymitis? Pediatr Emerg Care. 2011;27(3):174-178. (Retrospective; 160 patients) DOI: 10.1097/PEC.0b013e31820d647a
37. * Sheth KR, Keays M, Grimsby GM, et al. Diagnosing testicular torsion before urological consultation and imaging: validation of the TWIST score. J Urol. 2016;195(6):1870-1876. (Prospective validation; 128 patients) DOI: 10.1016/j.juro.2016.01.101
45. * Frohlich LC, Paydar-Darian N, Cilento BG Jr, et al. Prospective validation of clinical score for males presenting with an acute scrotum. Acad Emerg Med. 2017;24(12):1474-1482. (Prospective cohort; 258 patients) DOI: 10.1111/acem.13295
46. * Barbosa JA, Tiseo BC, Barayan GA, et al. Development and initial validation of a scoring system to diagnose testicular torsion in children. J Urol. 2013;189(5):1859-1864. (Prospective, 338 patients; with retrospective validation, 220 patients) DOI: 10.1016/j.juro.2012.10.056
47. * Qin KR, Qu LG. Diagnosing with a TWIST: systematic review and meta-analysis of a testicular torsion risk score. J Urol. 2022;208(1):62-70. (Systematic review and meta-analysis; 13 studies, 1060 patients) DOI: 10.1097/JU.0000000000002496
56. * Friedman N, Pancer Z, Savic R, et al. Accuracy of point-of-care ultrasound by pediatric emergency physicians for testicular torsion. J Pediatr Urol. 2019;15(6):608.E1-608.E6. (Retrospective; 120 patients) DOI: 10.1016/j.jpurol.2019.07.003
58. * Demirbas A, Demir DO, Ersoy E, et al. Should manual detorsion be a routine part of treatment in testicular torsion? BMC Urol. 2017;17(1):84. (Retrospective; 57 patients) DOI: 10.1186/s12894-017-0276-5
Subscribe to get the full list of 68 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: acute scrotal pain, testicular torsion, groin pain, testicle pain, acute scrotum, testicular ischemia, cremasteric reflex, sequelae of testicular torsion, testicular appendage torsion, intravaginal torsion, extravaginal torsion, bell clapper deformity, acute epididymitis, inguinal hernia, varicoceles, hydroceles, TWIST score, whirlpool sign, manual testicular detorsion, open-book method, trans-scrotal near-infrared spectroscopy, NIRS