

Acute gastroenteritis is a common condition frequently encountered in the urgent care setting. Although most cases are mild and self-limited, an important subgroup of patients will manifest severe disease that necessitates comprehensive diagnostic testing, empiric therapy, and escalation of care. This review provides evidence-based recommendations for the diagnosis, treatment, and disposition of adult patients with acute gastroenteritis. Guidance on management among special patient populations, including immunocompromised patients or patients with recent international travel, are discussed. Emerging issues in the field, such as evolving patterns of antimicrobial resistance and the impact of proton pump inhibitors on acute gastroenteritis, are also reviewed.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
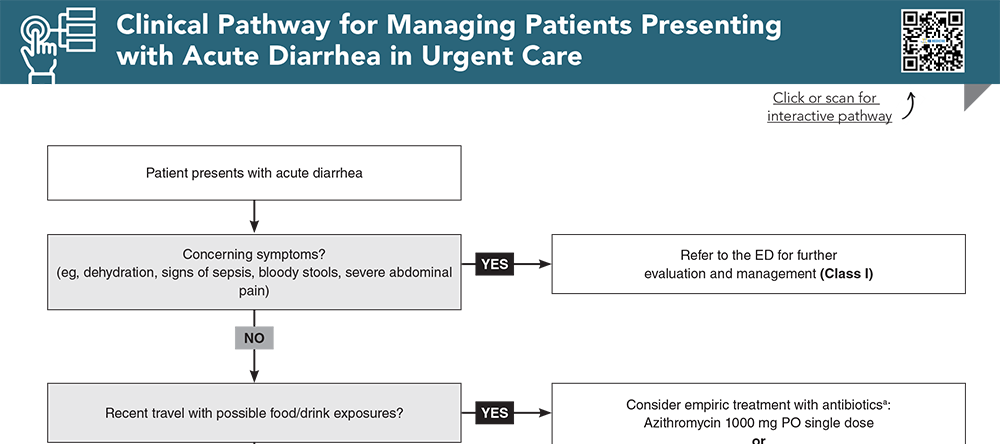
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
2. * Moon RC, Bleak TC, Rosenthal NA, et al. Epidemiology and economic burden of acute infectious gastroenteritis among adults treated in outpatient settings in US health systems. Am J Gastroenterol. 2023;118(6):1069-1079. (Retrospective epidemiological study; 248,896 patients) DOI: 10.14309/ajg.0000000000002186
3. * Riddle MS, DuPont HL, Connor BA. ACG clinical guideline: diagnosis, treatment, and prevention of acute diarrheal infections in adults. Am J Gastroenterol. 2016;111(5):602-622. (Clinical practice guidelines) DOI: 10.1038/ajg.2016.126
4. * Shane AL, Mody RK, Crump JA, et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017;65(12):e45-e80. (Clinical practice guidelines) DOI: 10.1093/cid/cix669
27. * McAuliffe GN, Anderson TP, Stevens M, et al. Systematic application of multiplex PCR enhances the detection of bacteria, parasites, and viruses in stool samples. J Infect. 2013;67(2):122-129. (Prospective comparative study; 1516 patients) DOI: 10.1016/j.jinf.2013.04.009
34. * Krones E, Hogenauer C. Diarrhea in the immunocompromised patient. Gastroenterol Clin North Am. 2012;41(3):677-701. (Review) DOI: 10.1016/j.gtc.2012.06.009
50. * Hartling L, Bellemare S, Wiebe N, et al. Oral versus intravenous rehydration for treating dehydration due to gastroenteritis in children. Cochrane Database Syst Rev. 2006;2006(3):CD004390. (Cochrane review; 17 studies, 1811 patients) DOI: 10.1002/14651858.CD004390.pub2
88. * Riddle MS, Connor BA, Beeching NJ, et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J Travel Med. 2017;24(suppl_1):S57-S74. (Expert guidance) DOI: 10.1093/jtm/tax026
91. * De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea. Cochrane Database Syst Rev. 2000;2000(3):CD002242. (Cochrane review; 20 studies) DOI: 10.1002/14651858.CD002242
98. * Kuschner RA, Trofa AF, Thomas RJ, et al. Use of azithromycin for the treatment of Campylobacter enteritis in travelers to Thailand, an area where ciprofloxacin resistance is prevalent. Clin Infect Dis. 1995;21(3):536-541. (Randomized controlled trial; 42 patients) DOI: 10.1093/clinids/21.3.536
101. *Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis. 2007;44(3):338-346. (Randomized controlled trial; 156 patients) DOI: 10.1086/510589
Subscribe to get the full list of 124 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: gastroenteritis, acute diarrhea, norovirus, traveler’s diarrhea, dehydration, gastrointestinal disorders, diarrhea with nausea and vomiting, dehydration, oral rehydration, rotovirus, bacterial infection
Christina Chien, MD; Peter D. Block, MD, MSc
Lisa M. Campanella-Coppo, MD, FACEP; Benjamin A. Silverberg, MD, MSc, FAAFP, FCUCM
October 1, 2024
October 1, 2027 CME Information
4 AMA PRA Category 1 Credits™. 4 AOA Category 2-B Credits. 4 AAFP Prescribed Credits