

Diverticular disease encompasses a spectrum of gastrointestinal conditions (but primarily diverticulosis and diverticulitis), which together affect a large proportion of the adult population, particularly people aged >40 years. Effective diagnosis and management of diverticular disease are crucial to minimizing complications and improving patient outcomes. Advancements in diagnostic imaging and the development of more refined treatment strategies have made it possible to manage diverticulitis more effectively. This issue reviews colonic diverticular disease, exploring the etiology, pathophysiology, and clinical management in the urgent care setting. Emphasis is placed on evidence-based approaches, emerging trends in treatment, and the critical role of early intervention in preventing serious complications.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
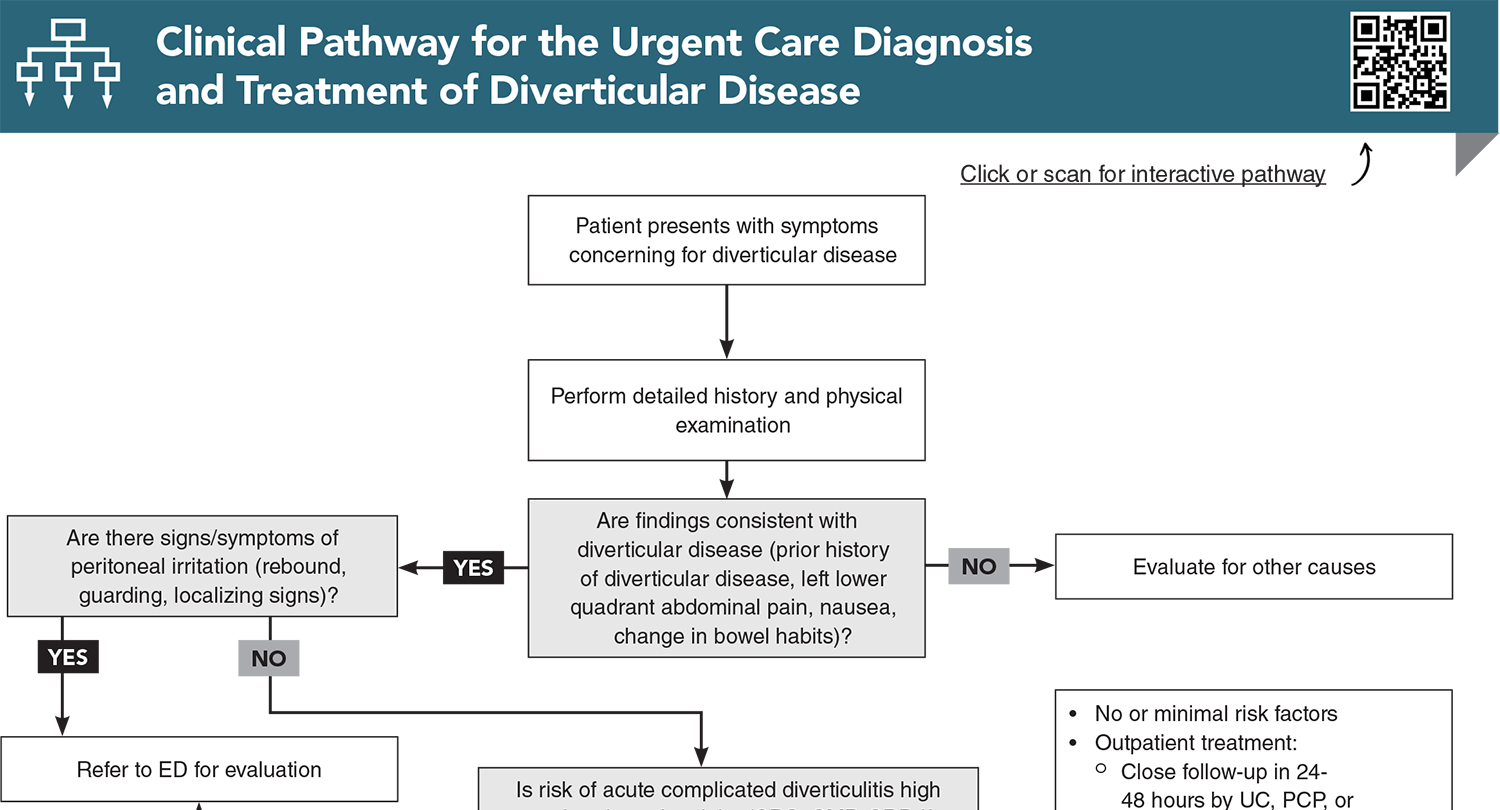
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
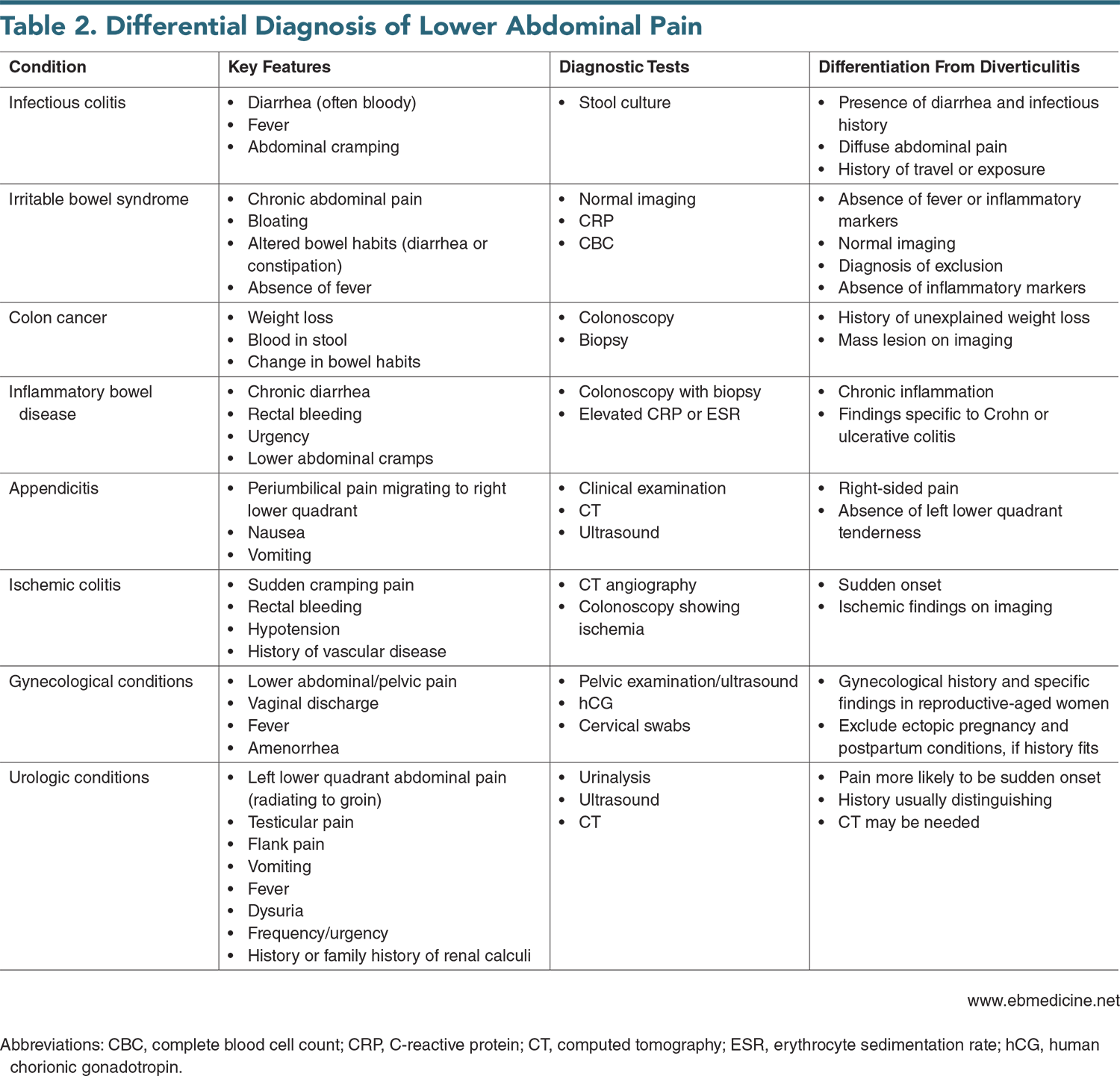
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
1. * Tursi A. Diverticulosis today: unfashionable and still under-researched. Therap Adv Gastroenterol. 2016;9(2):213-228. (Review) DOI: 10.1177/1756283X15621228
2. * Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management of diverticulosis and diverticular disease of the colon. Aliment Pharmacol Ther. 2015;42(6):664-684. (Review) DOI: 10.1111/apt.13322
7. * Carabotti M, Annibale B, Severi C, et al. Role of fiber in symptomatic uncomplicated diverticular disease: a systematic review. Nutrients. 2017;9(2). (Systematic review; 12 studies) DOI: 10.3390/nu9020161
8. * Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019;156(5):1282-1298 e1281. (Review) DOI: 10.1053/j.gastro.2018.12.033
11. * Hullar MA, Sandstrom R, Lampe JW, et al. The fecal microbiome differentiates patients with a history of diverticulitis vs those with uncomplicated diverticulosis. Gastroenterology. 2017;152(5):S1. (Cross-sectional analysis; 98 patients) DOI: 10.1016/S0016-5085(17)32217-5
12. * Tursi A, Mastromarino P, Capobianco D, et al. Assessment of fecal microbiota and fecal metabolome in symptomatic uncomplicated diverticular disease of the colon. J Clin Gastroenterol. 2016;50 Suppl 1:S9-S12. (Case-control study; 66 patients) DOI: 10.1097/MCG.0000000000000626
18. * Waugh N, Cummins E, Royle P, et al. Faecal calprotectin testing for differentiating amongst inflammatory and non-inflammatory bowel diseases: systematic review and economic evaluation. Health Technol Assess. 2013;17(55):xv-xix, 1-211. (Systematic review; 19 studies) DOI: 10.3310/hta17550
21. * Tursi A. A critical appraisal of advances in the diagnosis of diverticular disease. Expert Rev Gastroenterol Hepatol. 2018;12(8):791-796. (Critical review) DOI: 10.1080/17474124.2018.1487288
33. * Rottier SJ, van Dijk ST, Unlu C, et al. Complicated disease course in initially computed tomography-proven uncomplicated acute diverticulitis. Surg Infect (Larchmt). 2019;20(6):453-459. (Observational study; 1087 patients) DOI: 10.1089/sur.2018.289
47. * van Dijk ST, Daniels L, Unlu C, et al. Long-term effects of omitting antibiotics in uncomplicated acute diverticulitis. Am J Gastroenterol. 2018;113(7):1045-1052. (Randomized controlled trial; 528 patients) DOI: 10.1038/s41395-018-0030-y
52. * Stollman N, Smalley W, Hirano I. American Gastroenterological Association Institute guideline on the management of acute diverticulitis. Gastroenterology. 2015;149(7):1944-1949. (Guideline) DOI: 10.1053/j.gastro.2015.10.003
54. * Peery AF, Shaukat A, Strate LL. AGA clinical practice update on medical management of colonic diverticulitis: expert review. Gastroenterology. 2021;160(3):906-911. (Review) DOI: 10.1053/j.gastro.2020.09.059
Subscribe to get the full list of 63 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: colonic diverticular disease, diverticular disease, diverticula, diverticulitis, diverticulosis, microbiome, gut microbiota, computed tomography, colon, sigmoid colon, symptomatic uncomplicated diverticular disease (SUDD), C-reactive protein, probiotic, gastrointestinal, colonic pressure, dysbiosis, procalcitonin, uncomplicated acute diverticulitis, complicated acute diverticulitis, diverticular hemorrhage, dietary interventions
Andrew Alaya, MD, PhD
Shelley L. Janssen, MD, MBA; Cesar Mora Jaramillo, MD, FAAFP, FCUCM
August 1, 2025