Table of Contents
About This Issue
Constipation is a common, and distressing, presentation in urgent care. While it is usually benign and can be managed in the urgent care setting, occasionally constipation can indicate or lead to serious, life-threatening conditions such as fecal impaction and stercoral colitis. This issue of Evidence-Based Urgent Care emphasizes that constipation is a diagnosis of exclusion based on a focused history and physical examination to rule out emergent conditions and identify red-flag symptoms. The Bristol Stool Form Scale, clinical criteria, and digital rectal examination may play a key diagnostic role. Management should be tailored to the likely etiology of constipation, with most stable patients safely discharged on a bowel regimen and appropriate follow-up. In this issue, you will learn:
How to evaluate a presentation of constipation, including how to recognize dangerous etiologies and complications and how to perform a digital rectal examination;
Which treatments for constipation are appropriate for various underlying etiologies, comorbid medical conditions, and in concert with other medications; and
When and how to identify patients who may benefit from specialist or emergency department referral for consideration of advanced diagnostic and therapeutic options.
- About This Issue
- *Acknowledgement
- Abstract
- Case Presentations
- Introduction
- Etiology and Pathophysiology
- Differential Diagnosis
- Fecal Impaction
- Stercoral Colitis
- Other Potentially Dangerous Causes of Constipation
- Urgent Care Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Abdominal Radiographs
- Advanced Testing
- Treatment
- Treatment of Fecal Impaction
- Treatment of Stercoral Colitis
- Enemas
- Osmotic Laxatives
- Polyethylene Glycol
- Lactulose
- Magnesium
- Stimulant Laxatives
- Fiber Supplementation
- Disposition
- Special Populations
- Pregnant and Lactating Patients
- Patients on Hospice or at End of Life
- Patients Taking Glucagon-like Peptide-1 Receptor Agonists
- Controversies and Cutting Edge
- Intestinal Secretagogues
- Treatment of Opioid-Induced Constipation
- Relationship of the Gut Microbiome to Constipation
- Summary
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Managing Urgent Care Patients With Constipation
- Critical Appraisal of the Literature
- KidBits: Functional Constipation in Children
- Urgent Care Evaluation
- Treatment
- Conclusion
- References
- Case Conclusions
- Coding & Charting: What You Need to Know
- Coding Challenge: Presentation of Constipation in Urgent Care
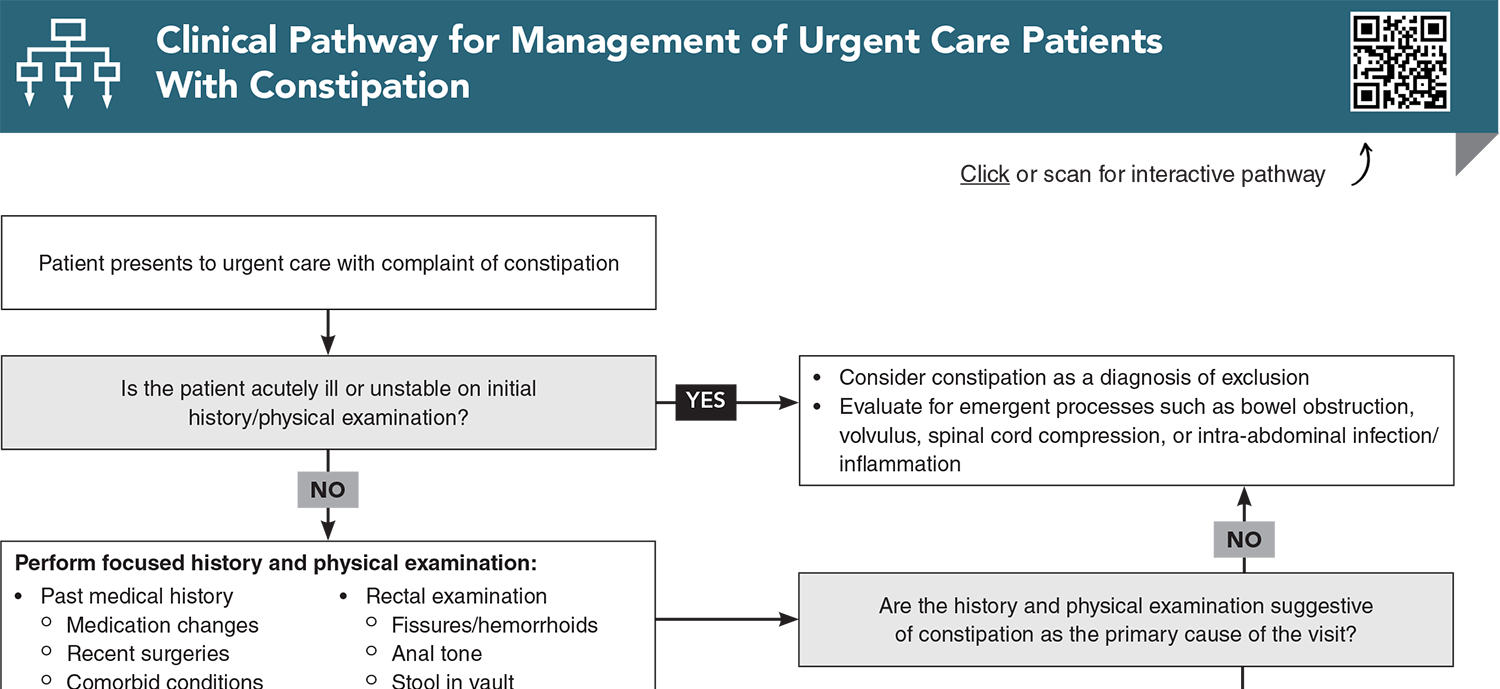
- Clinical Pathway for Management of Urgent Care Patients With Constipation
- References
*Acknowledgement
Portions of this content were previously published in: Richardson C. Emergency department evaluation and management of constipation. Emerg Med Pract. 2024;26(3):1-24. Used with permission of EB Medicine.
Abstract
Most cases of constipation are benign, but serious complications, such as fecal impaction and stercoral colitis, can occur. Data about how often patients present to urgent care with this complaint, as well as evidence to guide the evaluation and treatment of these patients, are limited. Many of the decades-old treatments have not been studied in modern, rigorous, controlled trials. Constipation is a clinical diagnosis, but one of exclusion, and ideal management includes evaluation for dangerous mimics or complications and, for most patients, discharging the patient with a bowel regimen tailored to the likely cause of their constipation, with appropriate referral to primary or specialty care. This review evaluates consensus guidelines on management of constipation as well as the early data on the newer prescription medications for chronic and opioid-induced constipation.
Case Presentations
- The patient has a history of diabetes, stroke, and mild dementia.
- The patient’s son reports that she is usually alert and oriented to person and place, but today she seems weak and confused and is barely talking.
- She hasn’t had a bowel movement in 5 days, even after getting an enema yesterday.
- On examination, she is tachycardic with a nontender but mildly distended abdomen. Her vital signs are: temperature, 37.3°C; heart rate, 114 beats/min; blood pressure, 104/58 mm Hg; and oxygen saturation, 94% on room air.
- You wonder whether an episode of simple constipation could make someone this sick…
- The patient says she has “not had a decent BM” in weeks, and the pain started as she strained, unsuccessfully, to have a bowel movement.
- She notes that she is taking oral iron supplementation for anemia, which got worse with her pregnancy.
- She is slightly tachycardic but afebrile, with otherwise normal vital signs. Her examination shows moderate tenderness in the right mid- and lower abdomen.
- You wonder if this is a simple case of constipation related to iron supplementation or whether the patient requires imaging….
- He has had no fever, nausea, or vomiting. They note that about a year prior, he had similar pain and that an enema given in his pediatrician’s office alleviated the problem, but his pediatrician is not available today.
- His vital signs are normal, and his examination reveals only minimal left lower abdominal tenderness. Genital examination is normal with nontender testes.
- You wonder if an x-ray is needed to confirm the diagnosis and whether an enema is reasonable to give in this case...
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Urgent Care Patients With Constipation
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Chang L, Chey WD, Imdad A, et al. American Gastroenterological Association-American College of Gastroenterology clinical practice guideline: pharmacological management of chronic idiopathic constipation. Am J Gastroenterol. 2023;164(7):1086-1106. (Guidelines) DOI: 10.14309/ajg.0000000000002227
7. * Zhou AZ, Lorenz D, Simon NJ, et al. Emergency department diagnosis and management of constipation in the United States, 2006-2017. Am J Emerg Med. 2022;54:91-96. (Cross-sectional study) DOI: 10.1016/j.ajem.2022.01.065
14. * Bharucha AE, Lacy BE. Mechanisms, evaluation, and management of chronic constipation. Gastroenterology. 2020;158(5):1232-1249. (Review) DOI: 10.1053/j.gastro.2019.12.034
19. * Rao SSC, Brenner DM. Efficacy and safety of over-the-counter therapies for chronic constipation: an updated systematic review. Am J Gastroenterol. 2021;116(6):1156-1181. (Systematic review; 41 studies) DOI: 10.14309/ajg.0000000000001222
26. * Keim AA, Campbell RL, Mullan AF, et al. Stercoral colitis in the emergency department: a retrospective review of presentation, management, and outcomes. Ann Emerg Med. 2023;82(1):37-46. (Retrospective study; 269 patients) DOI: 10.1016/j.annemergmed.2023.02.003
30. * Paquette IM, Varma M, Ternent C, et al. The American Society of Colon and Rectal Surgeons’ clinical practice guideline for the evaluation and management of constipation. Dis Colon Rectum. 2016;59(6):479-492. (Guideline) DOI: 10.1097/DCR.0000000000000599
38. * Peate I. How to perform digital removal of faeces. Nurs Stand. 2016;30(40):36-39. (Review) DOI: 10.7748/ns.30.40.36.s43
64. * Farmer AD, Drewes AM, Chiarioni G, et al. Pathophysiology and management of opioid-induced constipation: European expert consensus statement. United European Gastroenterol J. 2019;7(1):7-20. (Guideline) DOI: 10.1177/2050640618818305
69. * Hanson B, Siddique SM, Scarlett Y, et al. American Gastroenterological Association Institute technical review on the medical management of opioid-induced constipation. Gastroenterology. 2019;156(1):229-253. (Systematic review; 20 studies) DOI: 10.1053/j.gastro.2018.08.018
Subscribe to get the full list of 72 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: constipation, large intestine, stool, feces, gastrointestinal, colonic transit, fecal impaction, stercoral colitis, functional constipation, irritable bowel syndrome with constipation, opioid-induced constipation, occasional constipation, defecatory disorder, abdominal radiograph, digital rectal examination, Bristol Stool Form Scale, Rome Foundation diagnostic criteria, abdominal pain, bowel obstruction, osmotic laxatives, stimulant laxatives, stool softeners, bowel regimen, hemorrhoids, polyethylene glycol (PEG), bisacodyl, senna, enema, digital disimpaction, fiber, psyllium, lactulose, magnesium laxatives, intestinal secretagogues, peripherally acting mu-opioid receptor antagonists