

Each year, over 1.3 million patients visit the emergency department for constipation. Most cases are benign, but serious complications, such as fecal impaction and stercoral colitis, must be ruled out. Evidence to guide the evaluation and treatment of constipation in the emergency department is limited, and many of the decades-old treatments have not been studied in modern, rigorous, controlled trials. In the emergency department, constipation is a clinical diagnosis, and ideal management includes excluding dangerous mimics or complications and, for most patients, discharging the patient with a bowel regimen tailored to the likely cause of their constipation, with appropriate referral to primary or specialty care. This review evaluates consensus guidelines on management of constipation as well as the early data on the newer prescription medications for chronic and opioid-induced constipation.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
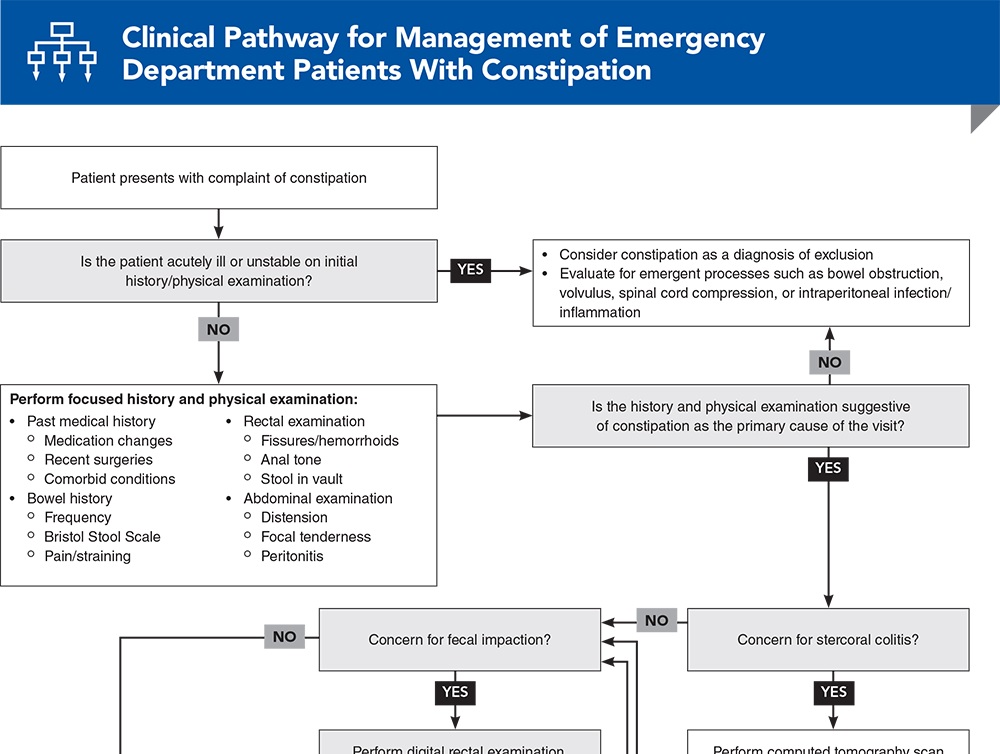
Subscribe to access the complete flowchart to guide your clinical decision making.
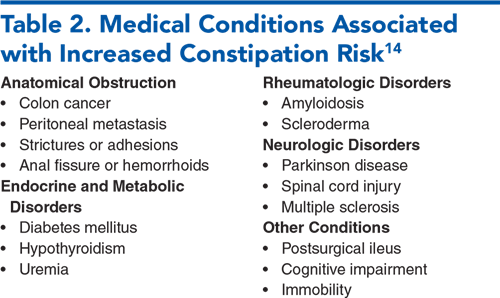
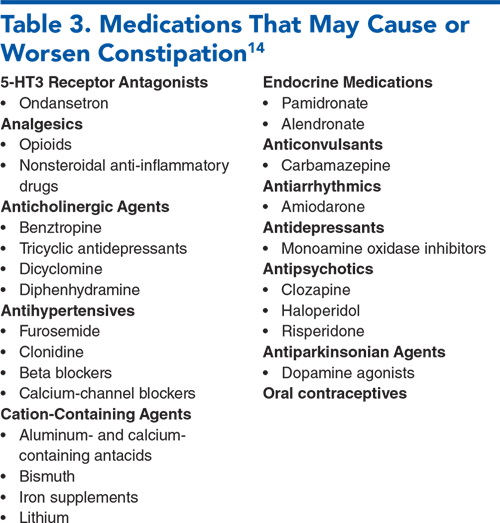
Subscribe for full access to all Tables and Figures.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
1. * Chang L, Chey WD, Imdad A, et al. American Gastroenterological Association-American College of Gastroenterology clinical practice guideline: pharmacological management of chronic idiopathic constipation. Am J Gastroenterol. 2023;164(7):1086-1106. (Guidelines) DOI: 10.1053/j.gastro.2023.03.214
4. * Rao SSC, Lacy BE, Emmanuel A, et al. Recognizing and defining occasional constipation: expert consensus recommendations. Am J Gastroenterol. 2022;117(11):1753-1758. (Review) DOI: 10.14309/ajg.0000000000001945
7. * Zhou AZ, Lorenz D, Simon NJ, et al. Emergency department diagnosis and management of constipation in the United States, 2006-2017. Am J Emerg Med. 2022;54:91-96. (Cross-sectional study) DOI: 10.1016/j.ajem.2022.01.065
13. * Bharucha AE, Lacy BE. Mechanisms, evaluation, and management of chronic constipation. Gastroenterology. 2020;158(5):1232-1249. (Review) DOI: 10.1053/j.gastro.2019.12.034
23. * Keim AA, Campbell RL, Mullan AF, et al. Stercoral colitis in the emergency department: a retrospective review of presentation, management, and outcomes. Ann Emerg Med. 2023;82(1):37-46. (Retrospective study; 269 patients) DOI: 10.1016/j.annemergmed.2023.02.003
27. * Paquette IM, Varma M, Ternent C, et al. The American Society of Colon and Rectal Surgeons’ clinical practice guideline for the evaluation and management of constipation. Dis Colon Rectum. 2016;59(6):479-492. (Guideline) DOI: 10.1097/DCR.0000000000000599
33. Establishment Registration & Device Listing. 2024. Accessed February 10, 2024. (FDA database)
36. * Peate I. How to perform digital removal of faeces. Nurs Stand. 2016;30(40):36-39. (Review) DOI: 10.7748/ns.30.40.36.s43
46. * Rao SSC, Brenner DM. Efficacy and safety of over-the-counter therapies for chronic constipation: an updated systematic review. Am J Gastroenterol. 2021;116(6):1156-1181. (Systematic review; 41 studies) DOI: 10.14309/ajg.0000000000001222
64. * Farmer AD, Drewes AM, Chiarioni G, et al. Pathophysiology and management of opioid-induced constipation: European expert consensus statement. United European Gastroenterol J. 2019;7(1):7-20. (Guideline) DOI: 10.1177/2050640618818305
69. GoodRx. 2023. Accessed February 10, 2024. (Drug price database)
72. * Hanson B, Siddique SM, Scarlett Y, et al. American Gastroenterological Association Institute technical review on the medical management of opioid-induced constipation. Gastroenterology. 2019;156(1):229-253. (Systematic review; 20 studies) DOI: 10.1053/j.gastro.2018.08.018
Subscribe to get the full list of 72 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: constipation, laxative, enema, disimpaction, stercoral colitis, impaction, opioid, IBS
Christopher Richardson, MD
Jessica Palmer, MD; Shawn Wassmuth, MD, FACEP
March 1, 2024
March 1, 2027 CME Information
4 AMA PRA Category 1 Credits™, 4 ACEP Category I Credits, 4 AAFP Prescribed Credits, 4 AOA Category 2-B Credits. Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 0.5 Palliative Care CME credit, subject to your state and institutional approval.