Table of Contents
About This Issue
Although thyroid disorders are common, decompensated hypothyroidism and thyroid storm represent the rare, life-threatening, extreme ends of the spectrum of thyroid dysfunction. Because laboratory thyroid hormone testing is not reliable for measuring these conditions in their acute stages, diagnosis depends on assessment of the patient’s history and physical manifestations. In this issue you will learn:
Which diseases may precipitate an acute thyroid crisis, and which diseases are caused or exacerbated by thyroid dysfunction.
How the seasons of the year, the patient’s age, and their affect and mood can help diagnose a thyroid crisis.
The strengths and limitations of scoring systems for thyroid storm.
The TSH, free T4, and T3 levels that are suggestive of thyroid disease, and the electrolyte and cardiac abnormalities that can be seen.
The recommended medications for decompensated hypothyroidism and thyroid storm, including the correct timing and sequence for administration.
How to manage a difficult airway in a patient with decompensated hypothyroidism.
The causes and special management requirements for pregnant and pediatric patients with acute thyroid dysfunction.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Etiology
- Hypothyroidism
- Hyperthyroidism
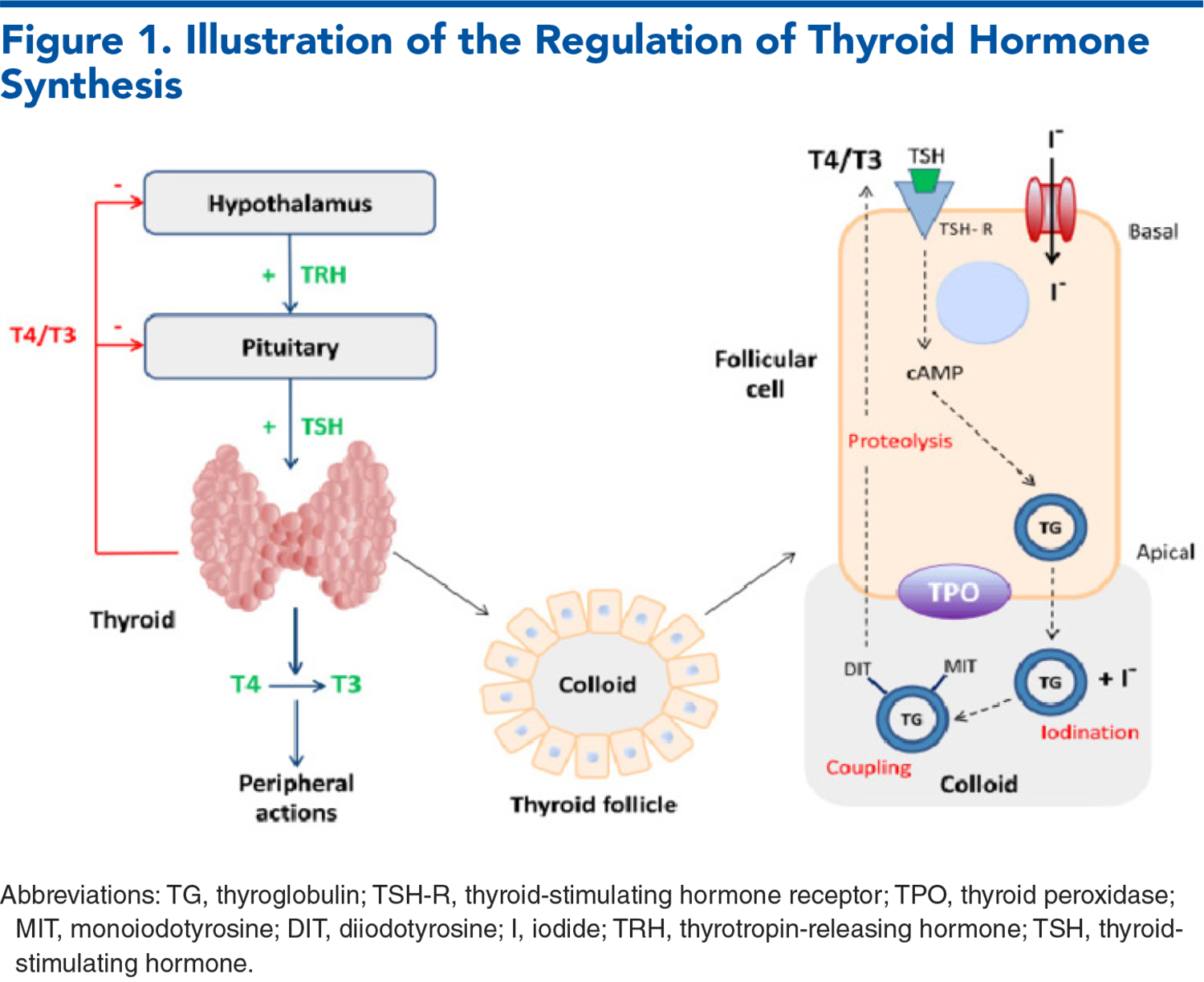
- Pathophysiology
- Differential Diagnosis
- Decompensated Hypothyroidism
- Thyroid Storm
- Prehospital Care
- Emergency Department Evaluation
- Stabilization
- History
- Decompensated Hypothyroidism
- Thyroid Storm
- Physical Examination
- Decompensated Hypothyroidism
- Thyroid Storm
- Diagnostic Studies
- Thyroid Hormone Levels
- Other Diagnostic Tests
- Electrolyte and Glucose Levels
- Cardiac Testing
- Treatment
- Decompensated Hypothyroidism
- Thyroid Storm
- Special Circumstances and Populations
- Airway Considerations
- Pregnant Patients
- Neonatal Hypothyroidism and Thyrotoxicosis
- Pediatric Patients
- Controversies and Cutting Edge
- Subclinical Hypothyroidism
- Disposition
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Patients With Thyroid Emergencies
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
- Clinical Pathways
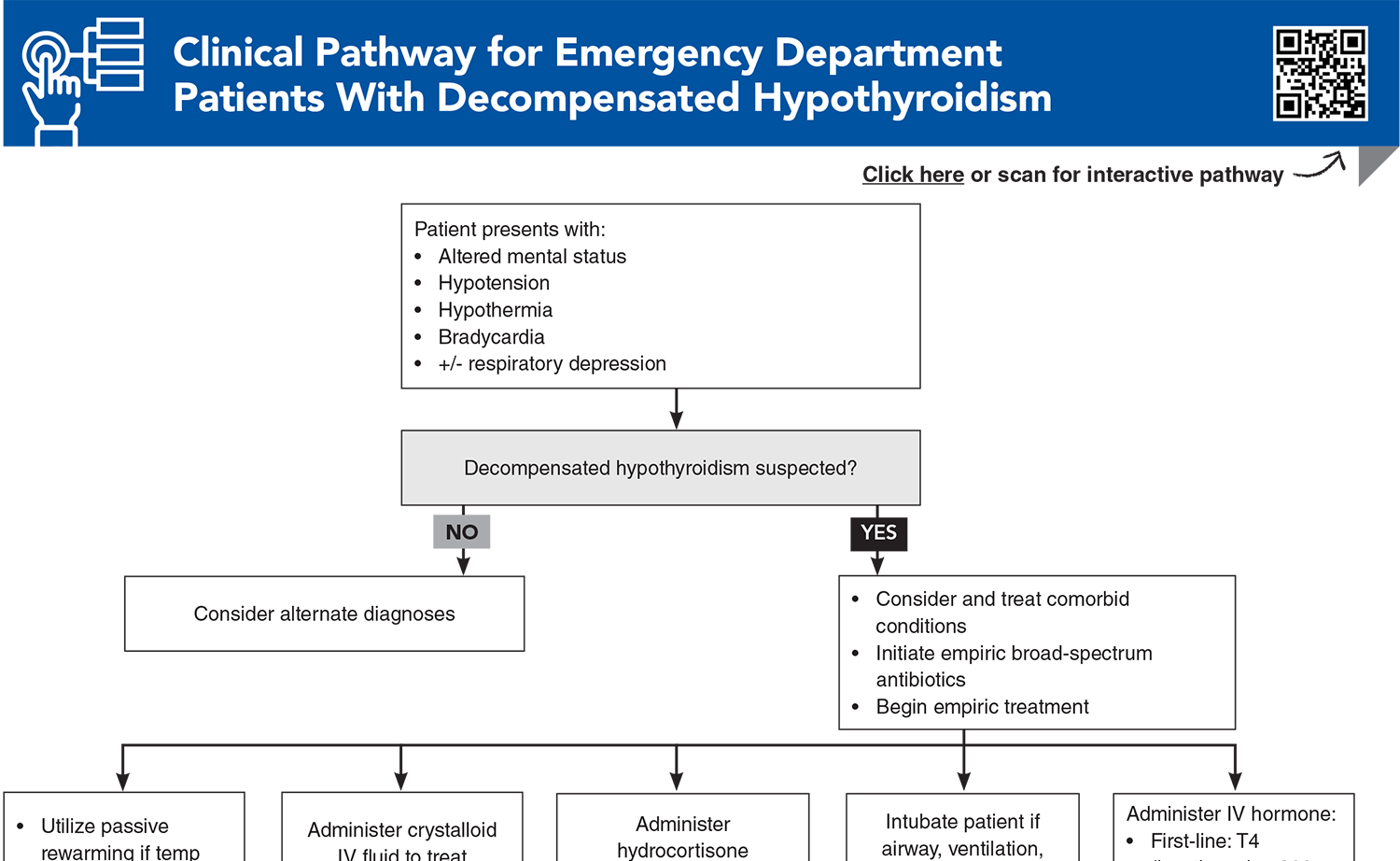
- Clinical Pathway for Emergency Department Patients With Decompensated Hypothyroidism
- Clinical Pathway for Emergency Department Patients With Thyroid Storm
- Tables and Figures
- References
Abstract
Patients experiencing thyroid emergencies can present with a wide array of clinical presentations and comorbid conditions, so a systematic strategy to identify key historical and physical examination features can help guide the emergency clinician in recognizing these infrequent conditions. This issue review the most up-to-date evidence for diagnosing and managing decompensated hypothyroidism and thyroid storm in adult, pediatric, and pregnant patients.
Case Presentations
- According to EMS, a family member found her at home, without heat, with an outdoor ambient temperature of 36°F. She was in a confused mental state.
- On EMS arrival, the patient was noted to be obtunded, with a temperature of 31.6°C, heart rate of 43 beats/min, blood pressure of 78/45 mm Hg, and respiratory rate of 15 breaths/min.
- In the ED, you note the patient to be cold and minimally responsive.
- Review of her medical record shows she currently takes lisinopril, atorvastatin, levothyroxine, and citalopram. Because the differential diagnosis for this patient is so broad, you wonder whether her medication list provides any clues…
- The patient states that her heart palpitations began 2 hours ago, and that for the past 2 weeks, she has felt anxious and has been experiencing nausea and diarrhea.
- Her vital signs are: temperature, 38.3°C; heart rate, 148 beats/min; blood pressure, 157/62 mm Hg; and respiratory rate, 25 breaths/min. Her weight is 52 kg.
- Her physical examination is notable for moderate distress, an irregularly irregular heart rhythm, clear lung sounds, a painless enlarged mass over the neck, and mild suprapubic and left costovertebral angle tenderness. She appears to be very thin for her height.
- You consider whether her anxiety, nausea, diarrhea, and palpitations are being driven by a more complex underlying process…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Patients With Decompensated Hypothyroidism
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Galindo RJ, Hurtado CR, Pasquel FJ, et al. National trends in incidence, mortality, and clinical outcomes of patients hospitalized for thyrotoxicosis with and without thyroid storm in the United States, 2004-2013. Thyroid. 2019;29(1):36-43. (Retrospective longitudinal analysis; 121,384 patients in national database) DOI: 10.1089/thy.2018.0275
3. * Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association Task Force on Thyroid Hormone Replacement. Thyroid. 2014;24(12):1670-1751. (Clinical practice guideline) DOI: 10.1089/thy.2014.0028
4. * Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26(10):1343-1421. (Clinical practice guideline) DOI: 10.1089/thy.2016.0229
5. * Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017;27(3):315-389. (Clinical practice guideline) DOI: 10.1089/thy.2016.0457
8. * Ono Y, Ono S, Yasunaga H, et al. Clinical characteristics and outcomes of myxedema coma: analysis of a national inpatient database in Japan. J Epidemiol. 2017;27(3):117-122. (Observational study; 149 patients) DOI: 10.1016/j.je.2016.04.002
Subscribe to get the full list of 105 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: hyperthyroidism, thyroid storm, myxedema, thyrotoxicosis, hypothyroidism, Graves, goiter, TSH, T3, T4, hypothermia, tachyarrhythmia, hydrocortisone