Table of Contents
About This Issue
Pediatric diabetes and its complications can present significant diagnostic and management challenges. This issue provides an evidence-based guide to identifying and managing the most common pediatric diabetic complications and emergencies. In this issue, you will learn:
Conditions in the differential diagnosis of children with fatigue and vomiting in the emergency department
Recommendations for prehospital care of pediatric patients with a diabetic emergency
Key historical questions that can help diagnose new-onset diabetes, as well as questions that should be asked to help direct care of patients with known diabetes
Biochemical criteria for diagnosis of diabetic ketoacidosis (DKA) and for hyperglycemic hyperosmolar state (HHS)
Which diagnostic studies should be obtained immediately, and which additional laboratory studies should be obtained for patients with hyperglycemia
General treatment recommendations for a 2-bag system, ongoing monitoring during treatment, and addressing complications during treatment
Specific treatment recommendations for mild DKA, moderate to severe DKA, hypoglycemia, and HHS
Guidance for disposition of pediatric patients with diabetic complications
-
About This Issue
-
Abstract
-
Case Presentations
-
Introduction
-
Critical Appraisal of the Literature
-
Etiology and Pathophysiology
-
Differential Diagnosis
-
Prehospital Care
-
Emergency Department Evaluation
-
History
-
Physical Examination
-
Diagnostic Studies
-
Imaging Studies
-
Treatment
-
2-Bag System
-
Diabetic Ketoacidosis
-
Mild Diabetic Ketoacidosis
-
Moderate to Severe Diabetic Ketoacidosis
-
Potassium and Phosphate Supplementation
-
Magnesium and Calcium Supplementation
-
Sodium Bicarbonate
-
General Fluid and Electrolyte Management Recommendations
-
Hypoglycemia
-
Hypoglycemia of Unknown Etiology
-
Hyperglycemic Hyperosmolar State
-
Monitoring During Treatment
-
Complications During Treatment
-
Cerebral Edema
-
Intubation
-
Additional Complications
-
Special Circumstances
-
Managing Patients With Diabetes in the Emergency Department
-
Insulin Pumps
-
Controversies and Cutting Edge
-
Cerebral Edema
-
1-Bag Versus 2-Bag Systems
-
Disposition
-
5 Things That Will Change Your Practice
-
Risk Management Pitfalls for Pediatric Patients With Diabetic Complications and Emergencies
-
Summary
-
Time- and Cost-Effective Strategies
-
Case Conclusions
-
Clinical Pathway for Management of Pediatric Diabetic Ketoacidosis in the Emergency Department
-
Tables and Figures
-
References
Abstract
Children with diabetes mellitus are at high risk for acute life-threatening complications of their chronic disease. Identification and management of these emergencies can be complex and challenging. This issue provides guidance for recognizing pediatric patients with new-onset diabetes as well as diabetic crises in established patients. The most recent literature is reviewed and an approach to managing emergent diabetic complications in the pediatric patient is provided, with a focus on initial stabilization and management. Key features in treating pediatric patients with hyperglycemic emergencies are discussed, including rapid fluid resuscitation when indicated, initiation of insulin, and addressing complicating comorbidities.
Case Presentations
-
The girl’s parents tell you she has had increased thirst and appetite over the last 6 weeks but has lost 2 kg since her last check-up.
-
She developed a runny nose and cough yesterday and a fever of 101°F, which has resolved. Today, she began vomiting and became fatigued.
-
Upon arrival to the ED, the girl is alert, but given her pale and fatigued appearance in triage, she was immediately taken to a room. Her vital signs are: temperature, 37°C; heart rate, 132 beats/min; blood pressure, 70/40 mm Hg; respiratory rate, 31 breaths/min; and oxygen saturation, 100% on room air. Her examination is notable for pallor and ill appearance. She has dry and cracked lips and is breathing fast, with clear lungs. She has epigastric tenderness, but otherwise her abdominal examination is normal.
-
You can tell this patient is ill, and her history is concerning. What treatment will you initiate to immediately address her shock?
-
The boy was diagnosed 1 year ago and has been using diet and exercise to manage his diabetes. He has felt a little more tired this week and also says he thinks his vision is a little blurry, but he has not had a recent eye examination.
-
Upon arrival to the ED, he is well-appearing and in no distress. He is eating a bag of spicy chips in the room. His examination is notable for obesity and acanthosis nigricans circumferentially on his neck. His vital signs are normal for his age except for a heart rate of 110 beats/min and blood pressure of 131/87 mm Hg.
-
As you assess this patient, you think about his elevated glucose at the pediatrician’s office. You are surprised he is so well-appearing, but you are worried about progression of his illness. How should you manage this patient?
-
She is here with her mother who found her daughter on the floor in her room after hearing a “thud.” The girl was not responsive to voice, but woke up in a drowsy state when her mother shook her vigorously. She continued to fall asleep and had to be repeatedly stimulated. The mother called 911 and then brought her daughter by private vehicle to the ED, which is only 5 minutes from their house.
-
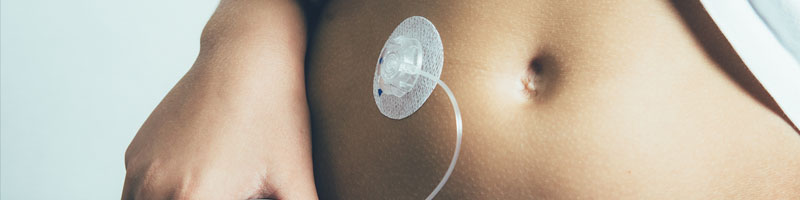
Upon arrival, the patient is minimally responsive, with a Glasgow Coma Scale score of 8. She has no signs of visible trauma, but on rapid examination, you notice that she has an insulin pump. You check a point-of-care glucose level, which is 29 mg/dL. You rapidly administer the adult dose of dextrose.
-
How does the presence of an insulin pump change your initial differential diagnosis prior to obtaining laboratory information? In addition to treating her low glucose, what additional steps are necessary to keep this patient safe?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Pediatric Diabetic Ketoacidosis in the Emergency Department
Subscribe to access the complete flowchart to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
3. * Kuppermann N, Ghetti S, Schunk JE, et al. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. N Engl J Med. 2018;378(24):2275-2287. (Randomized controlled trial; 1255 children) DOI: 10.1056/NEJMoa1716816
10. Laffel L, Svoren B. Epidemiology, presentation, and diagnosis of type 2 diabetes mellitus in children and adolescents. UpToDate. 2023. Accessed October 1, 2023. (Review)
12. * Marcin JP, Glaser N, Kuppermann N. Ventilation in pediatric diabetic ketoacidosis--not too much, but not too little. Pediatr Crit Care Med. 2005;6(4):489-490. (Retrospective cohort; 17 patients) DOI: 10.1097/01.Pcc.0000164636.58381.8f
16. * Glaser N, Fritsch M, Priyambada L, et al. ISPAD Clinical Practice Consensus Guidelines 2022: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2022;23(7):835-856. (Consensus guideline) DOI: 10.1111/pedi.13406
28. Texas Children’s Hospital. Diabetic ketoacidosis (DKA) clinical guideline: evidence-based guideline. 2019. Accessed October 1, 2023. (Consensus guideline)
33. Glaser N. Diabetic ketoacidosis in children: treatment and complications. UpToDate. 2023. Accessed October 1, 2023. (Review)
35. Yu ASL, Stubbs JR. Hypophosphatemia: evaluation and treatment. UpToDate. 2023. Accessed October, 2023. (Review)
36. Glaser N. Diabetic ketoacidosis in children: cerebral injury (cerebral edema). UpToDate. 2023. Accessed October 1, 2023. (Review)
37. * Glaser N, Barnett P, McCaslin I, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med. 2001;344(4):264-269. (Retrospective case-control; 416 children) DOI: 10.1056/nejm200101253440404
41. * Zeitler P, Haqq A, Rosenbloom A, et al. Hyperglycemic hyperosmolar syndrome in children: pathophysiological considerations and suggested guidelines for treatment. J Pediatr. 2011;158(1):9-14. (Review) DOI: 10.1016/j.jpeds.2010.09.048
42. Hirsch IB, Emmett M. Diabetic ketoacidosis and hyperosmolar hyperglycemic state in adults: Treatment. UpToDate 2023. Accessed October 1, 2023. (Review)
56. Levitsky L, Misra M. Insulin therapy for children and adolescents with type 1 diabetes mellitus. UpToDate. 2023. Accessed October 1, 2023. (Review)
59. * Azova S, Rapaport R, Wolfsdorf J. Brain injury in children with diabetic ketoacidosis: review of the literature and a proposed pathophysiologic pathway for the development of cerebral edema. Pediatr Diabetes. 2021;22(2):148-160. (Review) DOI: 10.1111/pedi.13152
Subscribe to get the full list of 59 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: diabetes, diabetic ketoacidosis, DKA, diabetes mellitus, diabetic crisis, hyperglycemic emergency, hyperglycemic hyperosmolar state, HHS, hyperglycemia, hypoglycemia, cerebral edema, insulin, two-bag system, 2-bag system, intubation, hypophosphatemia, phosphate, metabolic acidosis, ketosis, insulin pump