Table of Contents
About This Issue
Adrenal insufficiency results when the adrenal cortex cannot supply enough cortisol to meet physiological demands. The condition can have many causes and mechanisms, and its presentation may be vague and overlap with other conditions, such as nausea and vomiting, abdominal pain, altered mental status, or hypotension. Prompt administration of hydrocortisone will prevent life-threatening adrenal crisis. In this issue, you will learn:
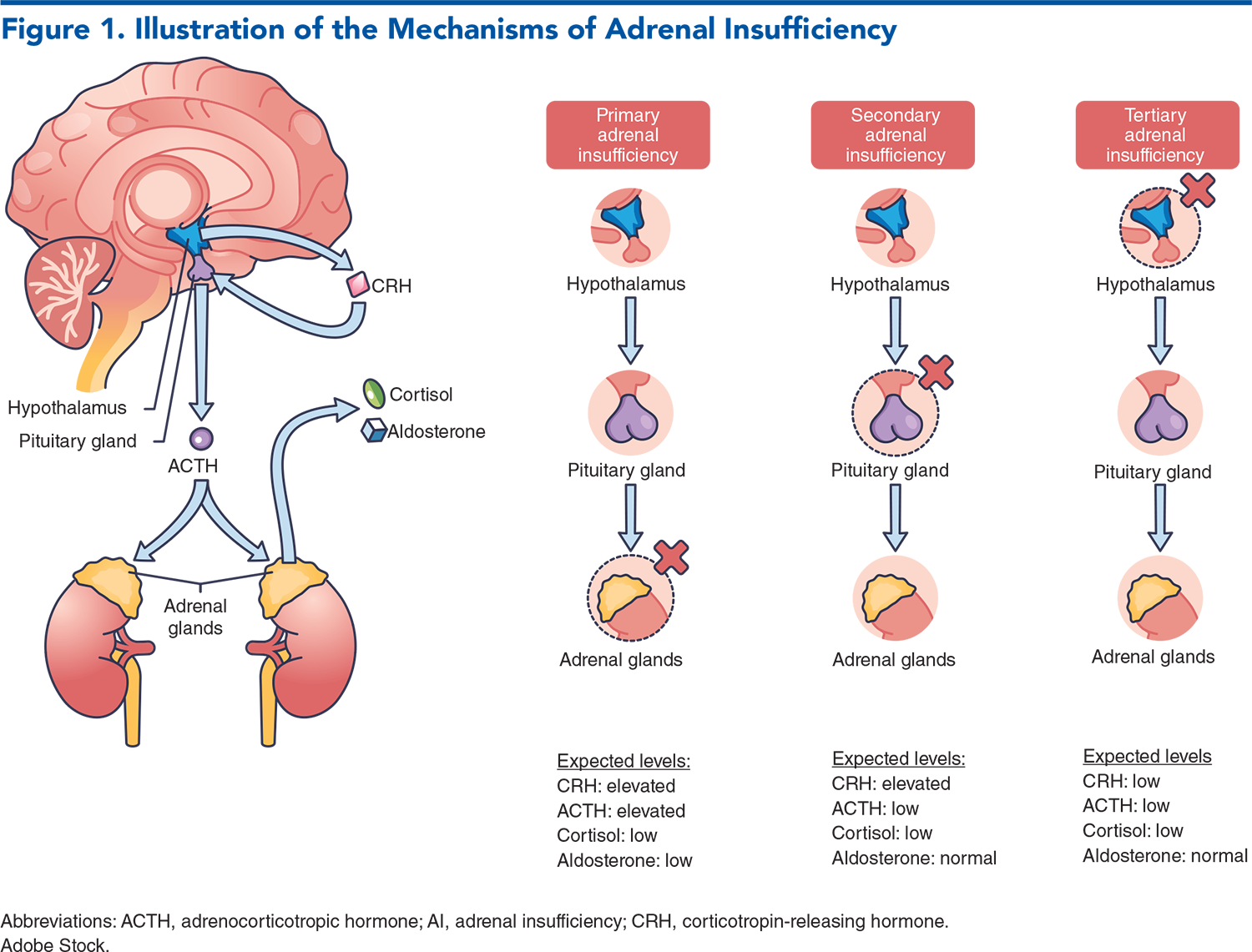
The 3 types of adrenal insufficiency – primary, secondary, and tertiary – their causes, and their management.
What prehospital providers and ED triage personnel need to know about adrenal insufficiency in order to manage these patients expeditiously before they get to the ED.
How the patient’s precipitating events (eg, infection, tumor, exogenous corticosteroid use) will influence signs and symptoms at presentation.
The laboratory studies that should be ordered when adrenal insufficiency is suspected – and what the common findings might be, based on the patient’s type of insufficiency.
Hydrocortisone and intravenous fluids recommendations to prevent or manage adrenal crisis.
What the dosing recommendations are for patients with chronic adrenal insufficiency: maintenance, sick-day, and for medical procedures.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Treatment
- Adrenal Insufficiency
- Adrenal Crisis
- Sick-Day Dosing
- Dosing for Medical Procedures
- Maintenance
- Prevention
- Special Populations
- Pregnant Patients
- Cutting Edge
- Advances in Hydrocortisone Delivery
- Selective Corticotropin-Releasing Factor Type 1 Receptor Antagonists
- Hydrocortisone Use in Septic Shock
- Disposition
- Summary
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Patients With Adrenal Insufficiency
- Dedication
- Case Conclusions
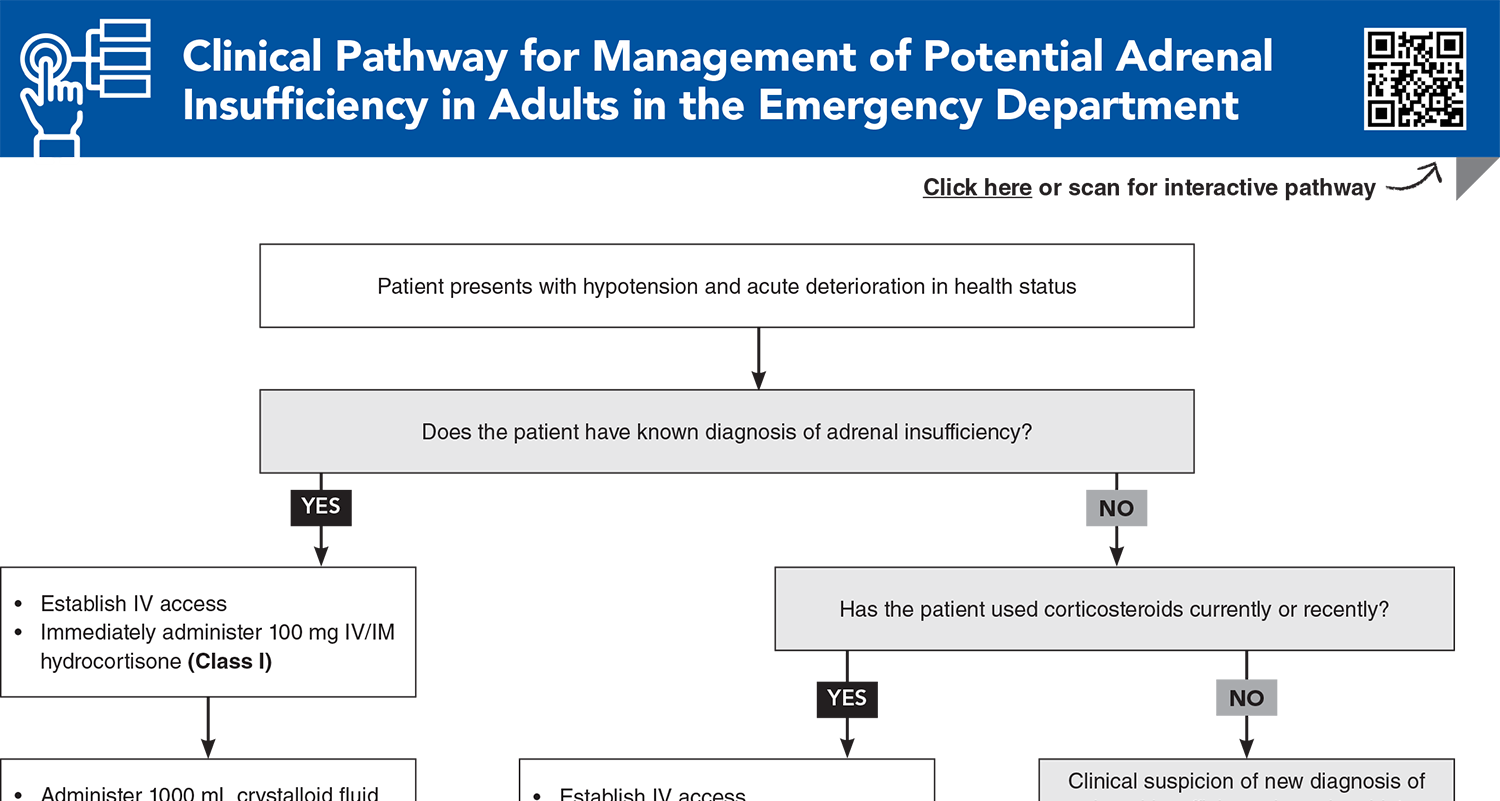
- Clinical Pathway for Management of Potential Adrenal Insufficiency in Adults in the Emergency Department
- Tables and Figures
- References
Abstract
Adrenal insufficiency is a challenging condition to diagnose and manage in the emergency department, and adrenal crisis remains a significant cause of morbidity and potential mortality. Rapid recognition of adrenal insufficiency and adrenal crisis is essential to ensure that life-saving therapy is initiated without delay. This issue provides a review of the etiology and pathophysiology of adrenal insufficiency and focuses on emergency department evaluation and treatment of this condition. The current literature was reviewed to provide an up-to-date guide and the best practices related to management of these diagnoses, as well as strategies for patient education and prevention.
Case Presentations
- The girl’s mother said she started vomiting a few hours ago, twice at home and once during triage. She is well-appearing, with signs of mild dehydration.
- Her vital signs are: temperature, 37°C; heart rate, 132 beats/min; blood pressure, 92/58 mm Hg; and respiratory rate, 24 breatahs/min.
- You have seen 2 other pediatric patients today with similar presentations who did not have congenital adrenal hyperplasia. They both responded well to oral dissolving tablet (ODT) ondansetron and were able to be discharged. Given her medical history, does your patient need additional workup and treatment, or can you proceed with ODT medication and a trial of oral rehydration?
- This patient seems to have the same virus as most of the patients that have been coming in, but chart review shows she has had more than 10 visits over the last 6 months to local EDs, urgent cares, and her primary care provider for vague complaints such as fatigue.
- Her vital signs are: temperature, 37.1°C; heart rate, 86 beats/min; blood pressure, 98/60 mm Hg; and respiratory rate, 18 breaths/min.
- She appears very tanned, and when you inquire, she says she went on vacation 5 months ago, but her tan never went away. She also notes she has been craving salty foods. You review her chart again and note she has had labs drawn a few times in the last 6 months, and she has consistently had low sodium levels, mildly elevated potassium, and glucose levels in the 60s.
- What tests should you order to further evaluate for adrenal insufficiency? What should the disposition be for this patient?
- He appears to be in mild distress. His vital signs reveal a temperature of 39°C, heart rate of 98 beats/min, blood pressure of 91/55 mm Hg, and respiratory rate of 28 breaths/min.
- Examination reveals focal crackles in his right lower lung. Chest x-ray confirms your suspicion for right lower lobe pneumonia. The patient says that he is due for the daily prednisone he takes for polymyalgia rheumatica.
- After administration of IV crystalloid fluids for his hypotension, his blood pressure has not improved. What should you do about the patient’s daily corticosteroid dose?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Managing Patients Presenting with Acute Diarrhea in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
2. * Puar TH, Stikkelbroeck NM, Smans LC, et al. Adrenal crisis: still a deadly event in the 21st century. Am J Med. 2016;129(3):339 e331-e339. (Review) DOI: 10.1016/j.amjmed.2015.08.021
3. * Hahner S, Spinnler C, Fassnacht M, et al. High incidence of adrenal crisis in educated patients with chronic adrenal insufficiency: a prospective study. J Clin Endocrinol Metab. 2015;100(2):407-416. (Prospective survey; 423 patients) DOI: 10.1210/jc.2014-3191
6. * Rushworth RL, Torpy DJ, Falhammar H. Adrenal crises: perspectives and research directions. Endocrine. 2017;55(2):336-345. (Review) DOI: 10.1159/000481660
7. * Hahner S, Hemmelmann N, Quinkler M, et al. Timelines in the management of adrenal crisis - targets, limits and reality. Clin Endocrinol (Oxf). 2015;82(4):497-502. (Prospective survey; 37 patients) DOI: 10.1007/s12020-016-1204-2
8. * Lentz S, Collier KC, Willis G, et al. Diagnosis and management of adrenal insufficiency and adrenal crisis in the emergency department. J Emerg Med. 2022;63(2):212-220. (Review) DOI: 10.1016/j.jemermed.2022.06.005
9. * Rushworth RL, Torpy DJ, Falhammar H. Adrenal crisis. N Engl J Med. 2019;381(9):852-861. (Review) DOI: 10.1056/NEJMra1807486
17. * Burger-Stritt S, Kardonski P, Pulzer A, et al. Management of adrenal emergencies in educated patients with adrenal insufficiency-a prospective study. Clin Endocrinol (Oxf). 2018;89(1):22-29. (Prospective study; 150 patients) DOI: 10.1111/cen.13608
25. * Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(2):364-389. (Clinical guideline) DOI: 10.1210/jc.2015-1710
Subscribe to get the full list of 52 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: Addison, cortisol, primary, crisis, glucocorticoid, hydrocortisone, corticosteroids, gastrointestinal