Table of Contents
About This Issue
Most neonatal rashes are benign and self-limited, but certain neonatal skin conditions require prompt identification and targeted treatment to prevent severe morbidity and mortality. The ability to differentiate characteristics of high-risk skin conditions from more benign neonatal rashes can be life-saving. This issue offers a strategic approach to the evaluation of neonatal rashes and offers guidance for differentiating benign findings from those that should raise concern and lead to further evaluation and management. In this issue, you will learn:
Descriptions of pertinent skin findings that are essential for diagnosis
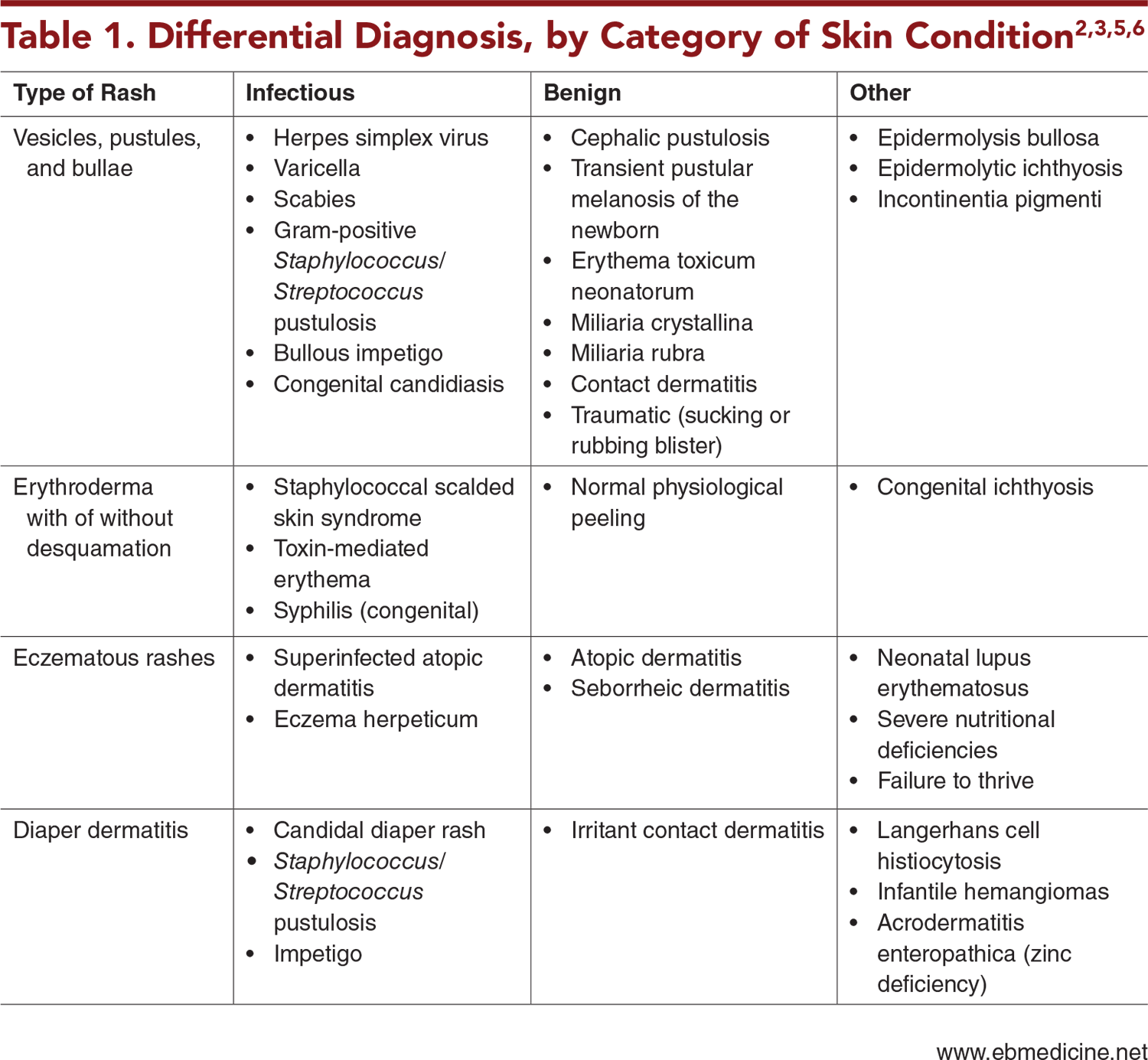
Four common categories of neonatal skin conditions that include diagnoses with the potential for serious outcomes: (1) vesicles, pustules, and bullae; (2) erythroderma with or without desquamation; (3) eczematous rashes; and (4) diaper dermatitis
Conditions in the broad differential diagnosis of neonatal rashes
Key aspects of the history that must be obtained, including maternal history, birth history, developmental history from birth up until the time of presentation, and a thorough family history
Physical examination findings that can narrow the diagnosis
General management considerations, as well as recommendations for management based on the skin findings and presentation
Guidance for disposition, including which neonates should be admitted and which can be discharged home with return precautions and close follow-up
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Emergency Department Evaluation
- Referral to an Emergency Department for Neonatal Skin Rashes
- Initial Stabilization
- History
- Physical Examination
- Diagnostic Studies
- Presenting Features and Management, Based on Skin Findings
- General Management
- Vesicles, Pustules, and Bullae
- Transient Neonatal Pustular Melanosis
- Erythema Toxicum Neonatorum
- Neonatal Cephalic Pustulosis
- Miliaria Crystallina and Miliaria Rubra
- Herpes Simplex Virus Infection
- Other Serious Conditions
- Erythroderma With or Without Desquamation
- Staphylococcal Scalded Skin Syndrome
- Congenital Syphilis
- Eczematous Rashes
- Neonatal Lupus Erythematosus
- Atopic Dermatitis
- Superinfection
- Diaper Dermatitis
- Candidal Infections
- Seborrheic Dermatitis
- Infantile Hemangiomas
- Other Conditions
- Special Populations
- Controversies and Cutting Edge
- Disposition
- Summary
- Risk Management Pitfalls for Neonates With Rashes in the Emergency Department
- Time- and Cost-Effective Strategies
- Case Conclusions
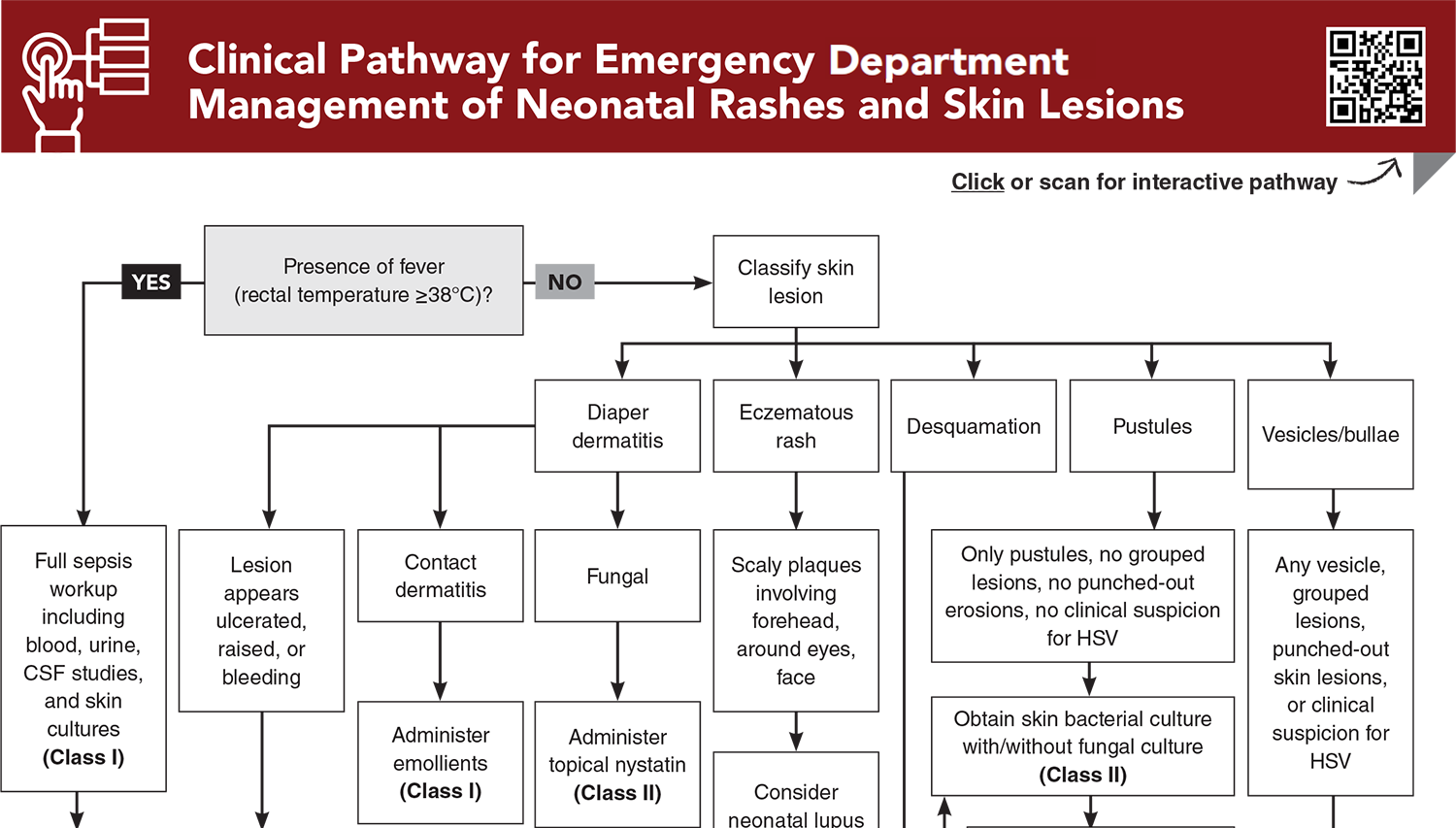
- Clinical Pathway for Emergency Department Management of Neonatal Rashes and Skin Lesions
- Tables, Figures, and Appendix
- References
Abstract
While most cases of neonatal rashes are benign and self-limited, certain neonatal skin conditions require prompt diagnosis and targeted treatment to prevent severe morbidity and mortality. Recognition of high-risk neonatal rashes and early intervention can significantly improve patient outcomes. Categorizing the rash can help delineate a differential diagnosis and determine whether the presentation and physical examination have features of a high-risk rash. This issue offers a strategic approach to the evaluation of neonatal skin conditions and offers guidance for differentiating benign findings from those that should raise concern and lead to further evaluation and management.
Case Presentations
- On arrival, the infant had a rectal temperature of 37.3°C and a heart rate of 156 beats/min. The nurse reports that he appears well overall. The mother tells you that she has no medical history, the baby was born full-term from a spontaneous vaginal delivery in a hospital setting, and that he was healthy at birth and discharged home shortly after. She tells you they have had many visitors, and she thinks that a cousin, who visited the infant right after delivery, might have had a facial rash.
- A quick examination of the boy’s skin reveals a group of vesicles on his forehead.
- What skin condition are you most worried it could be? For an afebrile, well-appearing neonate with a vesicular skin lesion, what diagnostic tests and treatment are necessary?
- The mother tells you the girl is her third baby who was born vaginally after induction at 36 weeks due to maternal hypertension. The infant spent 1 week in the neonatal intensive care unit for respiratory distress before being discharged.
- The mother says she is concerned because her newborn has had a rash that seems to be spreading. The rash started a week ago and was initially on the chest and now involves parts of the face, back, arms, and upper legs. It does not involve the diaper area. She says she is breastfeeding with some formula supplementation, which she started a couple of weeks ago.
- On examination, the infant’s vital signs are within normal limits, and the baby appears very well but has ill-defined xerotic plaques, most notable on the extensor arms and legs, cheeks, and trunk.
- What is the most probable cause of this rash? What advice would you provide this mother?
- The rash was noted this morning at the boy’s 1-month well-child check. The mother states the rash had been present for the last 1 to 2 days and has been rapidly spreading. The infant was born full-term without any complications and had been doing well until the skin changes were noted. No fevers were documented; however, the mother notes that he has been fussier and feeding less than usual.
- On examination, the infant’s vital signs are remarkable for an elevated temperature to 37.9°C and a heart rate of 177 beats/min. He is crying, appears uncomfortable, and is difficult to console. Examination of the skin reveals diffuse erythema with accentuation in the neck and axillae. You also make note of some crusting around the eyes and mouth, and focal areas of desquamation on the neck, in addition to noticing a few new developing areas in the skin folds around the diaper area.
- What diagnosis are you most concerned about? What are some options for treatment?
- The mother states the area has become very red and raw and has been worsening over the past 7 days. The baby cries unconsolably whenever she urinates or has a bowel movement. The mother is applying nystatin cream, without any improvement.
- On examination, the infant’s vital signs are within normal range. She is fussy but consolable. You notice a small infantile hemangioma on the chest, which the mother states has been there since 1 week of age and has gotten slightly more red. When examining the infant’s diaper area, you note diffuse erythema of the area extending over her labia majora and over her buttocks. In the center of her left buttock, you notice an annular ulceration about the size of a quarter, with a small amount of bleeding. The mother tells you she did not notice the bleeding beforehand.
- What is the most likely diagnosis and how would you approach initial management?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Depatment Management of Neonatal Rashes and Skin Lesions
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables, Figures, and Appendix
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Siegel M, Lee LW. Neonatal skin emergencies. Pediatr Ann. 2019;48(1):e36-e42. (Review) DOI: 10.3928/19382359-20181210-03
2. * Chadha A, Jahnke M. Common neonatal rashes. Pediatr Ann. 2019;48(1):e16-e22. (Review) DOI: 10.3928/19382359-20181206-01
10. * Pantell RH, Roberts KB, Adams WG, et al. Evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics. 2021;148(2):e2021052228. (Clinical guideline) DOI: 10.1542/peds.2021-052228
12. * Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed: Elsevier; 2017. (Book chapter)
16. * Cruz AT, Nigrovic LE, Xie J, et al. Predictors of invasive herpes simplex virus infection in young infants. Pediatrics. 2021;148(3):e2021050052. (Prospective study; 1367 infants) DOI: 10.1542/peds.2021-050052
19. * Yun S, Cotton C, Faith EF, et al. Management of pustules and vesicles in afebrile infants ≤60 days evaluated by dermatology. Pediatrics. 2024;154(1):e2023064364. (Retrospective study; 248 infants) DOI: 10.1542/peds.2023-064364
23. * Liy-Wong C, Pope E, Weinstein M, et al. Staphylococcal scalded skin syndrome: an epidemiological and clinical review of 84 cases. Pediatr Dermatol. 2021;38(1):149-153. (Retrospective cohort; 84 patients) DOI: 10.1111/pde.14470
24. * Gray L, Olson J, Brintz BJ, et al. Staphylococcal scalded skin syndrome: clinical features, ancillary testing, and patient management. Pediatr Dermatol. 2022;39(6):908-913. (Retrospective cohort; 67 patients) DOI: 10.1111/pde.15102
27. * Stafford IA, Workowski KA, Bachmann LH. Syphilis complicating pregnancy and congenital syphilis. N Engl J Med. 2024;390(3):242-253. (Review) DOI: 10.1056/NEJMra2202762
Subscribe to get the full list of 38 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: neonatal rashes, pediatric dermatology, dermatitis, vesicle, pustule, bullae, erythroderma, desquamation, eczematous rash, diaper dermatitis, diaper rash, bacterial infection, Staphylococcal, Staphylococcus, Streptococcal, Streptococcus, neonatal pustular melanosis, erythema toxicum neonatorum, neonatal cephalic pustulosis, miliaria crystallina, miliaria rubra, herpes simplex virus, HSV, staphylococcal scalded skin syndrome, SSSS, congenital syphilis, neonatal lupus erythematosus, lupus, atopic dermatitis, superinfection, candidal infection, seborrheic dermatitis, infantile hemangioma, hemangioma precursor, Langerhans cell histiocytosis, acrodermatitis enteropathica, scabies