Table of Contents
About This Issue
COVID-19 has had dramatic implications for the health and well-being of children from early 2020 to the present. Since the start of the pandemic, the COVID-19 topics relevant to the care of children have changed considerably. This issue reviews the presentation, evaluation, and management of pediatric patients with COVID-19, MIS-C, and long COVID. Additionally, the current literature supporting public health measures as well as COVID-19 vaccinations and their complications are discussed. In this issue, you will learn:
Differences between immunologic responses to SARS-CoV-2 in children and adults
Guidance for prehospital care of children with COVID-19 and those with MIS-C
When laboratory studies are indicated, and which patients should have additional workup
Recommendations for treatment, including respiratory and hemodynamic support measures, antiviral medications, and immunomodulation
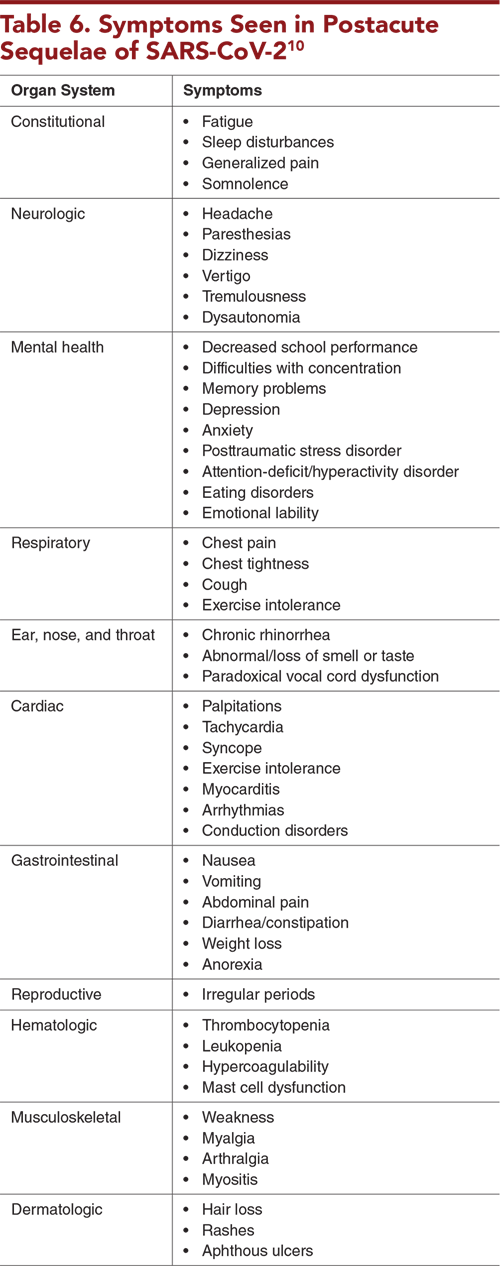
Special considerations for vulnerable populations; infection mitigation strategies; COVID-19 complications, long COVID, and postacute sequelae of SARS-CoV-2; and vaccine complications
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- COVID-19
- Etiology and Pathophysiology
- Differential Diagnosis
- Viral Infections
- Sepsis
- Bacterial Pneumonia
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Treatment
- Respiratory Support
- Medications
- Nirmatrelvir/Ritonavir
- Remdesivir
- Disposition
- Multisystem Inflammatory Syndrome in Children
- Etiology and Pathophysiology
- Differential Diagnosis
- Kawasaki Disease
- Toxic Shock Syndrome
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Other Diagnostic Studies
- Treatment
- Respiratory and Hemodynamic Support
- Immunomodulation
- Additional Considerations
- Disposition
- Special Considerations
- Vulnerable Populations
- Demographic Disparities
- Immunocompromised Patients
- Pregnant and/or Lactating Patients
- Neonates
- Risk to the Infant if the Mother is COVID-19–Positive
- COVID-19 and MIS-C in Neonates
- Infection Mitigation Strategies
- COVID-19 Complications, Long COVID, and Postacute Sequelae of SARS-CoV-2
- Vaccines
- Vaccine Impact on COVID-19
- Vaccine Impact on MIS-C
- Vaccine-Related Complications
- Vaccine-Induced and Viral Myocarditis
- Diagnosing and Treating Vaccine-Induced and Viral Myocarditis
- Controversies and Cutting Edge
- Availability of Data on COVID-19 Infections
- National Wastewater Surveillance System
- Artificial Intelligence Used for COVID-19 Detection on Chest X-ray
- MIS-C During Various COVID-19 Waves
- Summary
- Risk Management Pitfalls for Children With COVID-19 or MIS-C
- 5 Things That Will Change Your Practice
- Time- and Cost-Effective Strategies
- Case Conclusions
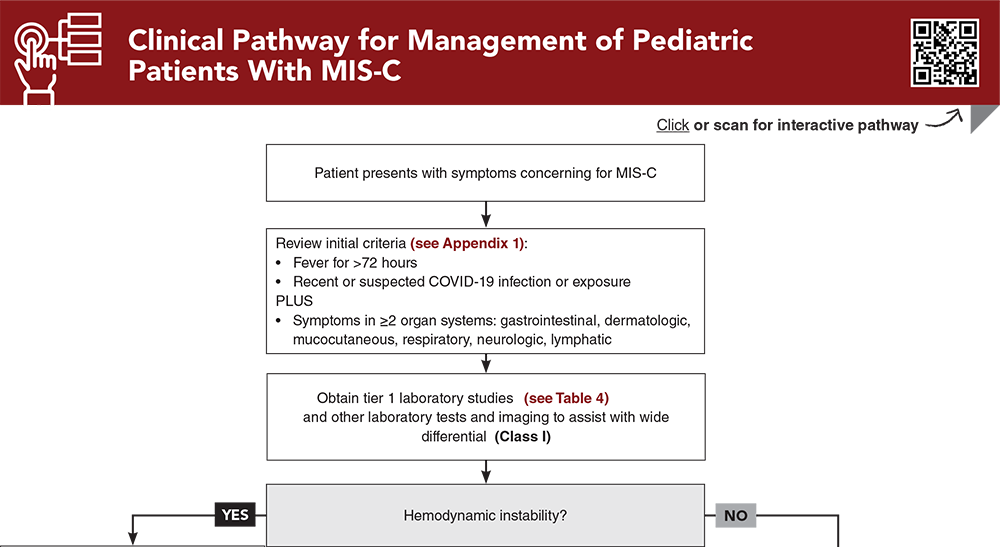
- Clinical Pathway for Management of Pediatric Patients With MIS-C
- Tables, Figures, and Appendix
- References
Abstract
COVID-19, the disease caused by SARS-CoV-2, has been disruptive worldwide. It was primarily a respiratory disease that affected many of the medically vulnerable, but the true impact of postacute sequelae of SARS-CoV-2 (PASC), which has been demonstrated to involve all organ systems, is now coming to light. In addition, a new disease entity emerged, multisystem inflammatory syndrome in children (MIS-C), which has had significant morbidity and mortality associated with it. This issue reviews the presentation, evaluation, and management of patients with COVID-19, MIS-C, and PASC. Additionally, the current literature supporting public health measures, as well as COVID-19 vaccinations and their complications are discussed.
Case Presentations
- A diffuse maculopapular rash started 2 days ago, and bilateral eye redness started today. The boy is reporting weakness and looks mildly dehydrated.
- The boy’s vital signs are: temperature, 38.6°C; heart rate, 134 beats/min; blood pressure, 100/45 mm Hg; respiratory rate, 20 breaths/min; and pulse oximetry, 98%. He has not traveled out of the country. He reports a diagnosis of COVID-19 3.5 weeks ago, along with other members of his family.
- What is your initial management of this patient? Is the COVID-19 history relevant?
- The girl had a maximum temperature of 39.4°C. The mother says she is concerned about the possibility of COVID-19. They live in a multigenerational home, and 2 grandparents are currently hospitalized with COVID-19. The mother thinks tests should be performed to assure she “will not get intubated like her grandparents.”
- The patient’s vital signs are temperature, 39.1°C; heart rate, 128 beats/min; blood pressure, 90/52 mm Hg; respiratory rate, 26 breaths/min; and pulse oximetry, 97%. A physical examination reveals a well-appearing, well-hydrated child in no respiratory distress. You note nasal congestion, a coarse cough, and clear lung sounds.
- Does her exposure to COVID-19 change your management plan? What are the risk factors for severe COVID-19 that you should be considering?
- The mother is recovering from COVID-19 that was diagnosed 1 day before an uncomplicated vaginal delivery. Her only symptom was a scratchy throat. The Apgar scores were 8 at 1 minute and 9 at 5 minutes. The baby stayed with the mother in her room and was discharged <2 days later. The baby’s birth weight was 7 lbs 2 oz, and he currently weighs 7 lbs 5 oz.
- The boy’s vital signs are: temperature, 38.9°C; heart rate 168 beats/min; blood pressure, 72/46 mm Hg; respiratory rate, 50 breaths/min; and pulse oximetry, 96%. The physical examination reveals a crying but consolable child with clear rhinorrhea, nasal congestion, and intermittent coughing, but is otherwise normal. The mother is tearful and very nervous about the possible effects of COVID-19 on her baby.
- Does the patient's age affect your decision-making? What are the concerns with COVID-19 infection in a newborn? What are the outcomes for neonatal COVID-19 infections?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Pediatric Patients With MIS-C
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables, Figures, and Appendix
Subscribe for full access to all Tables, Figures, and Appendix.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
10. * Rao S, Gross RS, Mohandas S, et al. Postacute sequelae of SARS-CoV-2 in children. Pediatrics. 2024;153(3):e2023062570. (Review) DOI: 10.1542/peds.2023-062570
17. * Leibowitz J, Krief W, Barone S, et al. Comparison of clinical and epidemiologic characteristics of young febrile infants with and without severe acute respiratory syndrome coronavirus-2 infection. J Pediatr. 2021;229:41-47. (Retrospective; 124 patients) DOI: 10.1016/j.jpeds.2020.10.002
35. * Harwood R, Allin B, Jones CE, et al. A national consensus management pathway for paediatric inflammatory multisystem syndrome temporally associated with COVID-19 (PIMS-TS): results of a national Delphi process. Lancet Child Adolesc Health. 2021;5(2):133-141. (Consensus guideline) DOI: 10.1016/S2352-4642(20)30304-7
39. * Ouldali N, Toubiana J, Antona D, et al. Association of intravenous immunoglobulins plus methylprednisolone vs immunoglobulins alone with course of fever in multisystem inflammatory syndrome in children. JAMA. 2021;325(9):855-864. (Retrospective cohort; 111 patients) DOI: 10.1001/jama.2021.0694
57. * Du Y, Chen L, Shi Y. Safety, immunogenicity, and efficacy of COVID-19 vaccines in adolescents, children, and infants: a systematic review and meta-analysis. Front Public Health. 2022;10:829176. (Systematic review and meta-analysis; 6 studies, 9912 patients) DOI: 10.3389/fpubh.2022.829176
Subscribe to get the full list of 78 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: coronavirus disease 2019, COVID-19, COVID, pediatric COVID, coronavirus, SARS-CoV-2, multisystem inflammatory syndrome in children, MIS-C, COVID testing, mRNA vaccine, COVID vaccination complications, long COVID, postacute sequelae of SARS-CoV-2, PASC, vaccine-induced myocarditis