

Portions of this content were previously published in: Goldberg E. An evidence-based approach to managing asymptomatic elevated blood pressure in the emergency department. Emerg Med Pract. 2015;17(2): 1-24. Used with permission of EB Medicine.
Many patients presenting to urgent care are unaware of their hypertensive status, placing them at substantial risk for cardiovascular, renal, neurological, and ocular complications without appropriate recognition and follow-up. Urgent care clinicians must be prepared to address elevated blood pressure readings while also avoiding unnecessary emergency department referrals for patients who can be safely managed in the outpatient setting. This issue provides evidence-based guidance on the clinical approach to asymptomatic hypertension in adult patients in the urgent care setting, including differentiation of hypertensive emergency from poorly controlled hypertension. Current guidelines on acute care management of high blood pressure are reviewed, along with treatment, disposition, and follow-up recommendations.
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
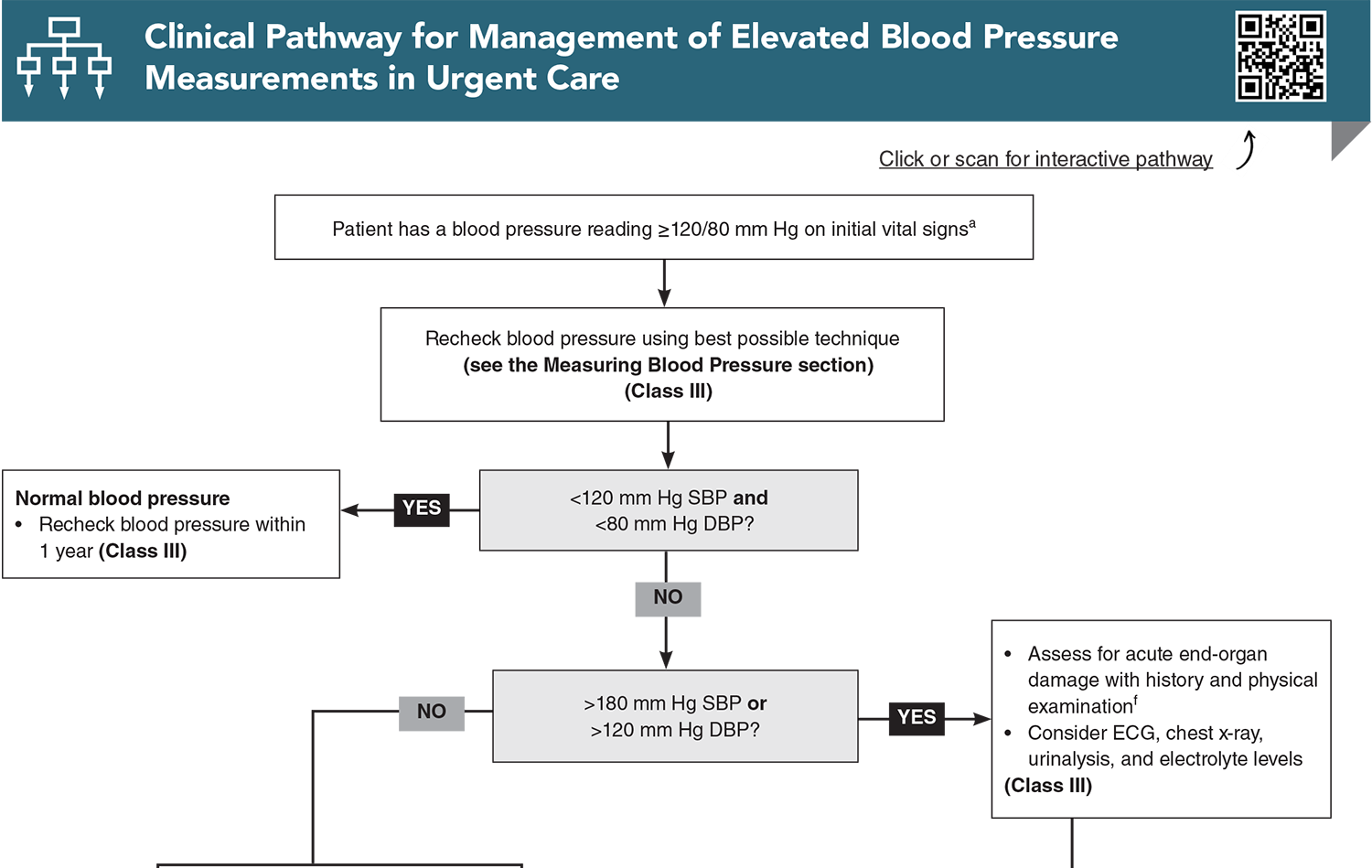
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
Following are the most informative references cited in this paper, as determined by the authors.
1. * Jones DW, Ferdinand KC, Taler SJ, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Hypertension. 2025;82(10):e212-e316. (Clinical practice guideline) DOI: 10.1161/HYP.0000000000000249
2. * Taler SJ. Initial treatment of hypertension. N Engl J Med. 2018;378(7):636-644. (Review) DOI: 10.1056/NEJMcp1613481
3. * Carey RM, Moran AE, Whelton PK. Treatment of hypertension: a review. JAMA. 2022;328(18):1849-1861. (Review)
Wolf SJ, Lo B, Shih RD, et al. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013;62(1):59-68. (Clinical policy statement) DOI: 10.1001/jama.2022.19590
5. * Peixoto AJ. Acute severe hypertension. N Engl J Med. 2019;381(19):1843-1852. (Review) DOI: 10.1056/NEJMcp1901117
6. * Bress AP, Anderson TS, Flack JM. The management of elevated blood pressure in the acute care setting: a scientific statement from the American Heart Association. Hypertension. 2024;81(8):e94-e106. (Scientific statement) DOI: 10.1161/HYP.0000000000000238
7. * Rossi GP, Rossitto G, Maifredini C. Management of hypertensive emergencies: a practical approach. Blood Press. 2021;30(4):208-219. (Systematic review; 18 studies) DOI: 10.1080/08037051.2021.1917983
8. * Gemme S, Meltzer AC, et al; American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Asymptomatic Hypertension. Clinical policy: a critical issue in the outpatient management of adult patients presenting to the emergency department with asymptomatic elevated blood pressure: approved by the ACEP Board of Directors January 22, 2025. Ann Emerg Med. 2025;86(1):e1-e11. (Clinical policy statement) DOI: 10.1016/j.annemergmed.2024.09.016
9. * US Centers for Disease Control and Prevention. Estimated hypertension prevalence, treatment, and control among U.S. adults. Million Hearts. Updated May 12, 2023. Accessed November 15, 2025.(Government statistical data)
32. * Whelton PK, Carey RM, Aronow WS. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College Of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. (Clinical practice guideline) DOI: 10.1161/HYP.0000000000000066
Subscribe to get the full list of 115 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: elevated blood pressure, high blood pressure, hypertension, stage 1 hypertension, stage 2 hypertension, severe hypertension, hypertensive emergency, BARKH, primary hypertension, secondary hypertension, coarctation of the aorta, lifestyle modifications, DASH diet, antihypertensive, thiazide, diuretic, ACEI, ARB, calcium-channel blocker, PREVENT
Melissa Orman, MD
Claude E. Shackelford, MD
December 1, 2025