Table of Contents
About This Issue
Venous thromboembolism (VTE) is often overlooked in children due to overall low incidence. Emergency clinicians who care for pediatric patients may struggle with the balance of avoiding excessive testing versus not missing a VTE. This issue provides an evidence-based review of pediatric VTE, including the epidemiology, presenting clinical signs and symptoms, diagnostic modalities, and treatment options. In this issue, you will learn:
Risk factors for pediatric VTE
The physiology of blood coagulation, including procoagulant and anticoagulant factors in the coagulation cascade
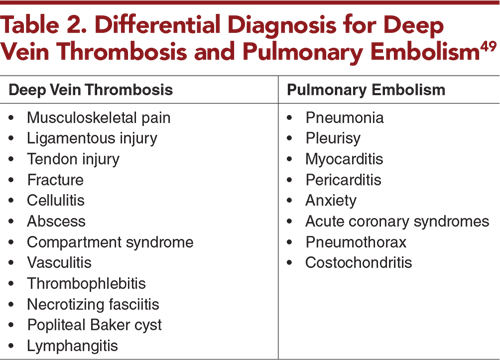
Common diagnoses in the differential for deep vein thrombosis and pulmonary embolism
Recommendations for diagnostic studies that will help identify patients at risk for VTE
Guidance for treatment of VTE, including recommendations for treatment duration, anticoagulation, and thrombolysis
Special considerations for neonates, patients with a central venous catheter-associated thrombus, and patients with heritable thrombophilia
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Etiology
- Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- Deep Vein Thrombosis
- Pulmonary Embolism
- Diagnostic Studies
- Laboratory Studies
- D-dimer
- Other Laboratory Studies
- Low-Risk Clinical Predictive Rules
- Cardiac Studies
- Radiologic Imaging
- Doppler Ultrasound, Computed Tomographic Venography, and Magnetic Resonance Venography
- Computed Tomographic Angiography and Magnetic Resonance Angiography
- Ventilation-Perfusion Lung Scanning
- Imaging After Detection of a Pulmonary Embolism
- Treatment
- Duration of Treatment
- Anticoagulation
- Heparins
- Complications of Heparin
- Vitamin K Antagonists
- Direct Oral Anticoagulants
- Thrombolysis
- Occluded Central Venous Catheter
- Special Populations
- Neonates
- Patients With a CVC-Associated Thrombus
- Patients With Heritable Thrombophilia
- Patients With Postthrombotic Syndrome
- Controversies and Cutting Edge
- Disposition
- Summary
- Risk Management Pitfalls in Management of Venous Thromboembolism in Pediatric Patients
- Time- and Cost-Effective Strategies
- Case Conclusions
- 5 Things That Will Change Your Practice
- Clinical Pathways
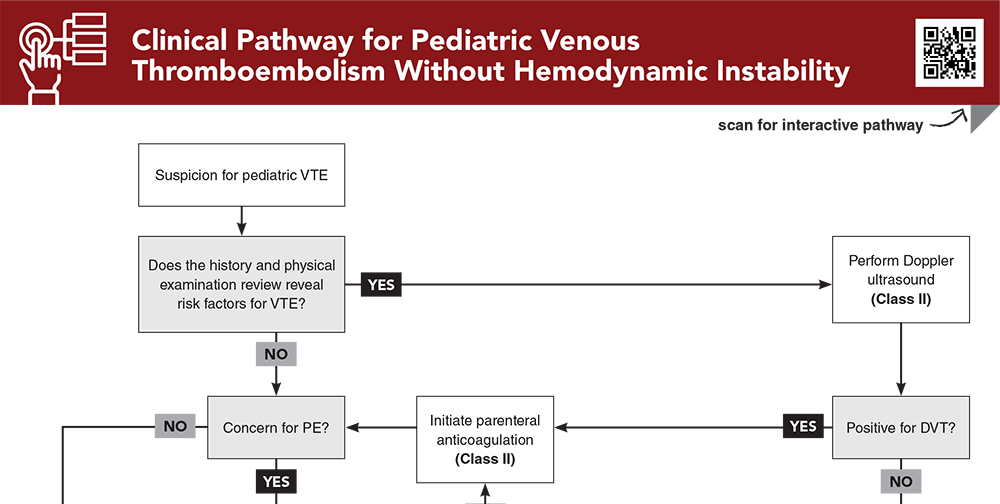
- Clinical Pathway for Pediatric Venous Thromboembolism Without Hemodynamic Instability
- Clinical Pathway for CVC-Associated Thrombosis
- Tables and Figures
- References
Abstract
Although the incidence of pediatric venous thromboembolism is increasing, it is often overlooked in children due to the overall low incidence. This issue reviews the epidemiology of pediatric venous thromboembolism, including the factors that have led to its increasing prevalence, and discusses the physiology of hemostasis and coagulation. Key features of the history and physical examination, as well as identification of risk factors, are reviewed, as these have the most diagnostic value for venous thromboembolism in pediatric patients. Recommendations are also provided for diagnostic testing and management in the emergency department.
Case Presentations
- The girl is tachypneic and mildly tachycardic, with an oxygen saturation of 98% on room air. As you begin the workup, her mother mentions that her daughter underwent pinning of a leg fracture recently and has been immobile for the past 6 days. She says the girl started taking oral contraceptives 3 months ago.
- How should you begin your workup? Does this patient require emergent imaging to rule out a pulmonary embolism?
- The girl is currently undergoing induction-phase treatment for acute lymphoblastic leukemia. They are accompanied by the home nurse who states that there has been difficulty flushing home medications through the girl’s central venous catheter. The girl has otherwise been doing well, without any fevers or other symptoms.
- Your ED team administered a trial of alteplase with no success.
- Should you try alteplase again? What other options should be considered for management of this patient?
- Due to miscommunication between her parents, she has been getting her oral contraceptive medication (prescribed for dysmenorrhea) twice a day instead of once a day. She developed leg pain and swelling 3 days ago, and an ultrasound today confirmed a popliteal vein thrombus.
- The girl is nonverbal. Her parents do not think she has had any difficulty breathing, and she has normal vital signs in the ED.
- Does this patient need to be treated for her deep vein thrombosis? Does she need other imaging or laboratory studies?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Pediatric Venous Thromboembolism Without Hemodynamic Instability
Subscribe to access the complete flowchart to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
4. * Monagle P, Chan AKC, Goldenberg NA, et al. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e737S-e801S. (Practice guidelines) DOI: 10.1378/chest.11-2308
5. * Monagle P, Cuello CA, Augustine C, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2018;2(22):3292-3316. (Society guidelines) DOI: 10.1182/bloodadvances.2018024786
69. * Hennelly KE, Baskin MN, Monuteuax MC, et al. Detection of pulmonary embolism in high-risk children. J Pediatr. 2016;178:214-218. (Retrospective; 561 patients) DOI: 10.1016/j.jpeds.2016.07.046
86. * Male C, Lensing AWA, Palumbo JS, et al. Rivaroxaban compared with standard anticoagulants for the treatment of acute venous thromboembolism in children: a randomised, controlled, phase 3 trial. Lancet Haematol. 2020;7(1):e18-e27. (Multicenter, parallel-group, open-label, randomized study; 520 patients) DOI: 10.1016/S2352-3026(19)30219-4
87. * Goldenberg NA, Kittelson JM, Abshire TC, et al. Effect of anticoagulant therapy for 6 weeks vs 3 months on recurrence and bleeding events in patients younger than 21 years of age with provoked venous thromboembolism: the Kids-DOTT randomized clinical trial. JAMA. 2022;327(2):129-137. (Randomized controlled trial; 417 patients) DOI: 10.1001/jama.2021.23182
98. * Halton J, Brandao LR, Luciani M, et al. Dabigatran etexilate for the treatment of acute venous thromboembolism in children (DIVERSITY): a randomised, controlled, open-label, phase 2b/3, non-inferiority trial. Lancet Haematol. 2021;8(1):e22-e33. (Randomized controlled trial; 267 patients) DOI: 10.1016/S2352-3026(20)30368-9
Subscribe to get the full list of 122 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: deep vein thrombosis, DVT, venous thromboembolism, VTE, pulmonary embolism, PE, thrombus, D-dimer, Wells criteria, PERC rule, coagulation, anticoagulation, heparin, unfractionated heparin, UFH, low-molecular-weight heparin, LMWH, vitamin K antagonist, direct oral anticoagulant, DOAC, thrombolysis, central venous catheter, CVC, occluded central venous catheter, catheter occlusion, thrombophilia, hemodynamic instability, postthrombotic syndrome