Table of Contents
About This Issue
Increasing evidence suggests that the sole surrogate ECG marker, ST-segment elevation, may have insufficient sensitivity for identifying high-risk patients with coronary occlusion who may benefit from emergent revascularization. This issue examines the evidence for considering STEMI equivalents in identifying patients with acute coronary occlusion who may not meet traditional STEMI criteria. In this issue, you will learn:
How the occlusion/nonocclusion myocardial infarction (OMI/NOMI) paradigm can work with the STEMI/NSTEMI paradigm to help guide decisions on pharmacotherapies and reperfusion.
How the STEMI criteria are measured
How the STEMI equivalents of left bundle branch block and ventricular-paced rhythms, hyperacute T waves, posterior STEMI, and the de Winter sign can help identify patients with life-threatening coronary occlusions
How to use the Sgarbossa and the Smith-modified Sgarbossa criteria to assess ischemia
When posterior myocardial infarction might be present, and how to test for it
Recognizing acute or subacute ischemia, reciprocal ST-segment depression, and inferior myocardial infarction
When transthoracic echocardiography should be ordered
Recommendations for analgesia and pharmacotherapy
Reperfusion therapies: when fibrinolytics are appropriate, and when transfer for PCI is required
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Pathophysiology and Nomenclature
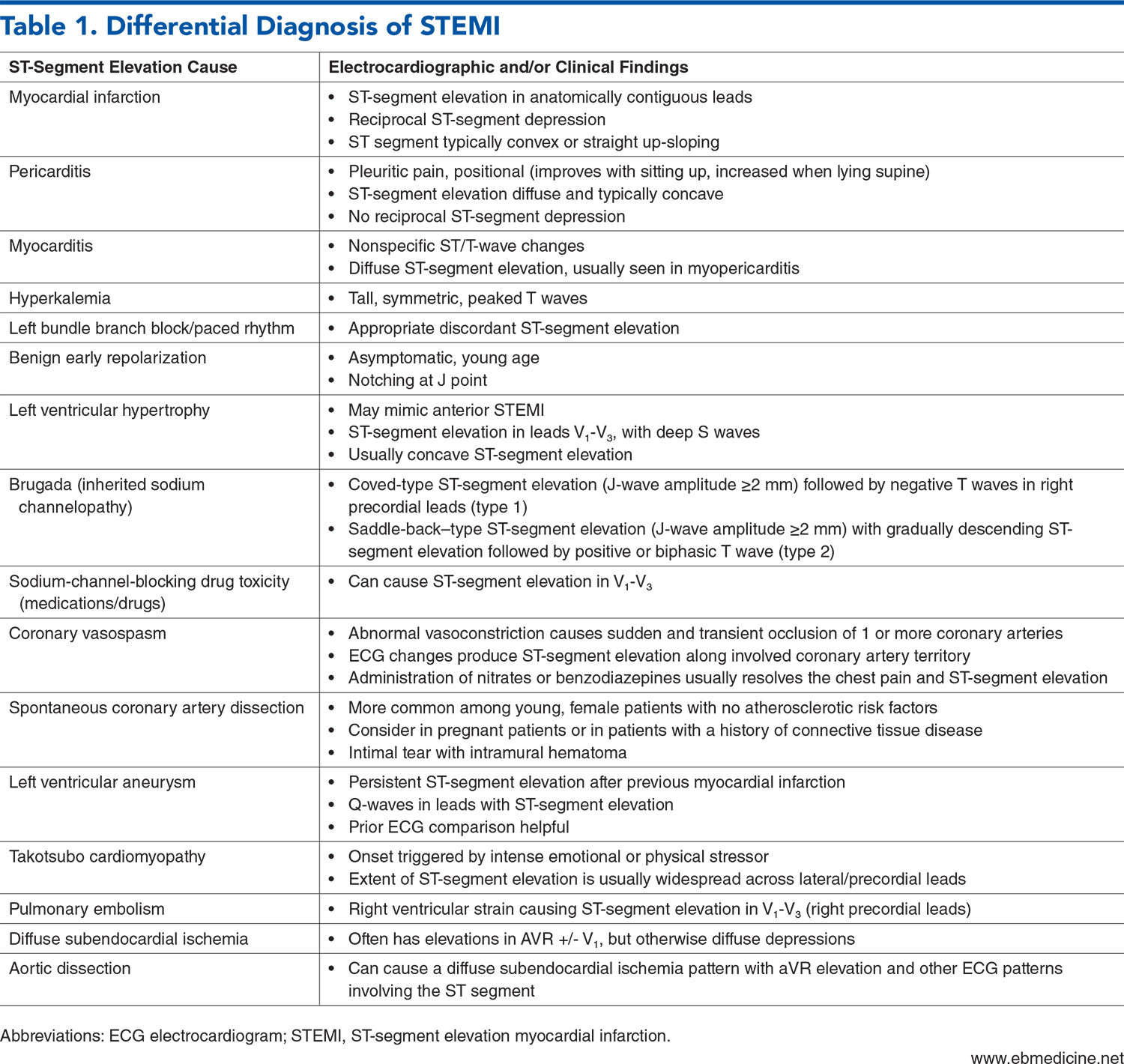
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Diagnostic Studies
- Electrocardiogram
- STEMI Criteria
- STEMI Equivalents
- Left Bundle Branch Block and Ventricular-Paced Rhythms With Sgarbossa Criteria and/or Smith-Modified Sgarbossa Criteria
- Smith-Modified Sgarbossa Criteria
- Hyperacute T Waves
- Posterior Myocardial Infarction
- The de Winter Sign
- Electrocardiogram Findings Consistent With Acute or Subacute Ischemia
- aVR ST-Segment Elevation
- Wellens Syndrome
- Reciprocal ST-Segment Depression
- Inferior Myocardial Infarction
- Laboratory Testing
- Imaging Studies
- Chest X-Ray
- Transthoracic Echocardiography
- Treatment
- Supplemental Oxygen
- Analgesia
- Nitrates
- Pharmacotherapies for STEMI
- Antiplatelet Medications
- Aspirin
- P2Y12 Inhibitors
- Agent Selection
- Timing of Administration
- Glycoprotein IIb/IIIa Receptor Inhibitors
- Anticoagulation Therapies
- Reperfusion Therapies
- Percutaneous Coronary Intervention
- Fibrinolytic Therapy
- Considerations for Management in Non–Percutaneous Coronary Intervention-Capable Hospitals
- Special Populations
- Management of STEMI Patients Presenting With Cardiac Arrest
- Controversies and Cutting Edge
- Disposition
- Risk Management Pitfalls in Managing Patients With Suspected Acute Coronary Occlusion
- 5 Things That Will Change Your Practice
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
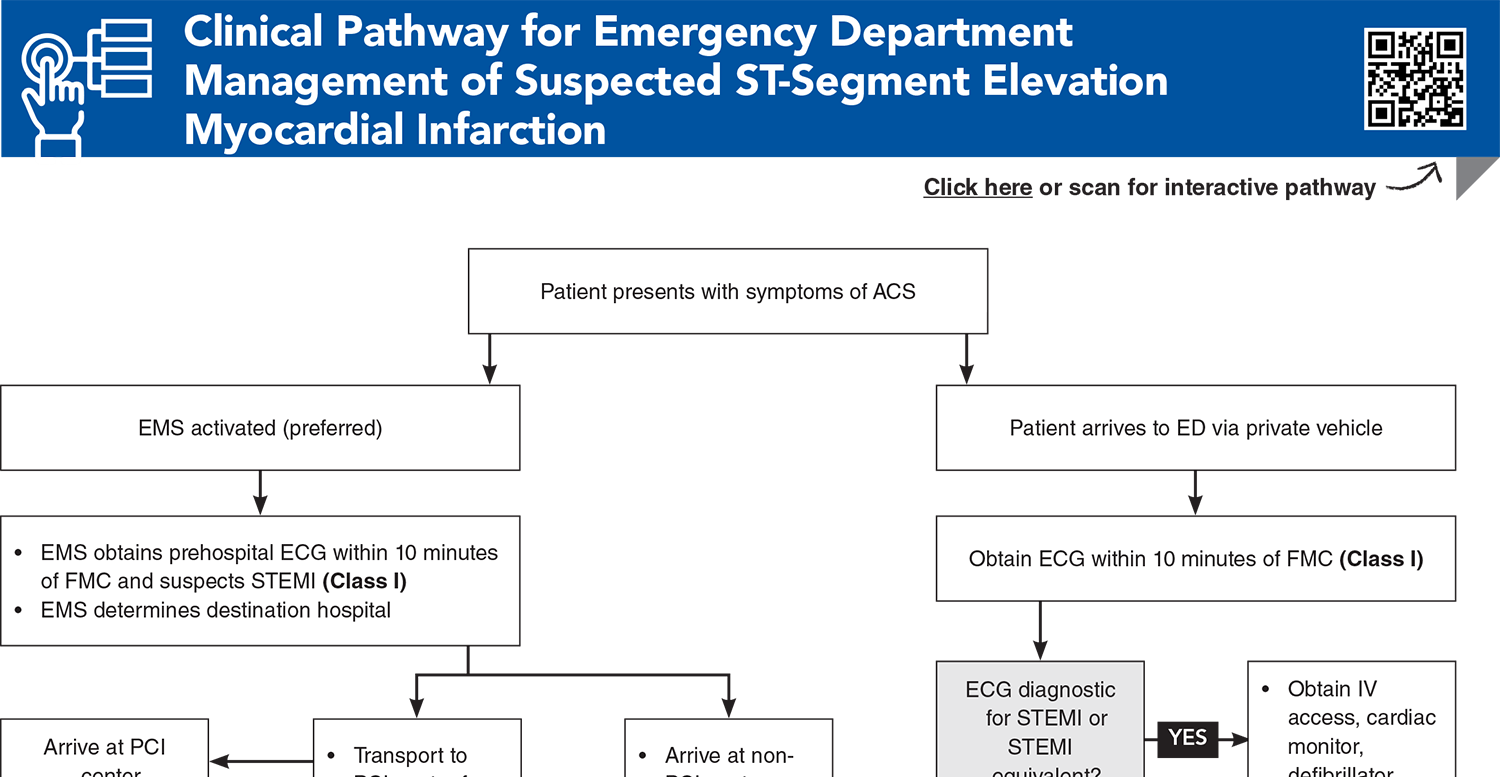
- Clinical Pathway for Emergency Department Management of Suspected ST-Segment Elevation Myocardial Infarction
- Tables and Figures
- References
Abstract
Acute coronary occlusion is a time-sensitive cardiac emergency that requires early, accurate diagnosis and prompt treatment to restore coronary perfusion, usually by percutaneous coronary intervention. Successful management of these patients demands a highly coordinated effort among emergency medical services, the emergency department, and cardiology. This issue highlights the importance of recognizing distinct electrocardiographic patterns that represent acute coronary occlusion, even in the absence of traditional STEMI criteria, and reviews evidence-based management recommendations.
Case Presentations
- Upon arrival, the patient complains of ongoing substernal chest pain. His vital signs are normal.
- EMS reports that the prehospital ECG did not show STEMI. The patient was administered aspirin and sublingual nitroglycerin en route.
- You immediately order a 12-lead ECG, which showed abnormally large T waves by both height and width relative to the QRS size in leads V1 to V3.
- You consider the significance of this and whether to activate the cath lab…
- She is pale, diaphoretic, and in distress, clutching her chest.
- Her vital signs are normal. You obtain an ECG in triage. (See Figure 1.)
- You consider what the most appropriate next step in management would be…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Suspected ST-Segment Elevation Myocardial Infarction
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80(20):1925-1960. (Evidence-based practice guideline) DOI: 10.1016/j.jacc.2022.08.750
4. * O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362-e425. (ACC/AHA evidence-based practice guideline) DOI: 10.1016/j.jacc.2012.11.019
5. * Rao SV, O’Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025;151(13):e771-e862. (ACC/AHA evidence-based practice guideline) DOI: 10.1161/CIR.0000000000001309
6. * Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720-3826. (Evidence-based practice guideline) DOI: 10.1093/ehjacc/zuad107
20. * Smith SW, Dodd KW, Henry TD, et al. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med. 2012;60(6):766-776. (Retrospective; 3 institutions, 162 patients) DOI: 10.1016/j.annemergmed.2012.07.119
Subscribe to get the full list of 66 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: ACO, STEMI, NSTEMI, ACS, ECG, OMI, PCI, myocardial infarction, equivalent, Sgarbossa, posterior, fibrinolytic, reperfusion