Table of Contents
About This Issue
Patients with juvenile idiopathic arthritis (JIA) may come to the emergency department (ED) with an initial presentation or with related flares of disease. Differentiating JIA from emergent causes of joint pain can be challenging. Prompt recognition of JIA and related complications can avoid unnecessary testing and incorrect treatments. This issue reviews the clinical presentation of JIA, provides guidance for differentiating JIA from conditions with similar presentations, and offers recommendations for management of JIA and JIA-related complications in the ED. In this issue, you will learn:
Subclassifications of JIA including: (1) oligoarticular JIA; (2) polyarticular JIA; (3) psoriatic arthritis; (4) enthesitis-related arthritis; (5) systemic-onset JIA; and (6) undifferentiated arthritis
Complications of JIA such as riziform bodies, temporomandibular arthritis, macrophage activating syndrome, uveitis, and vulnerability to infections
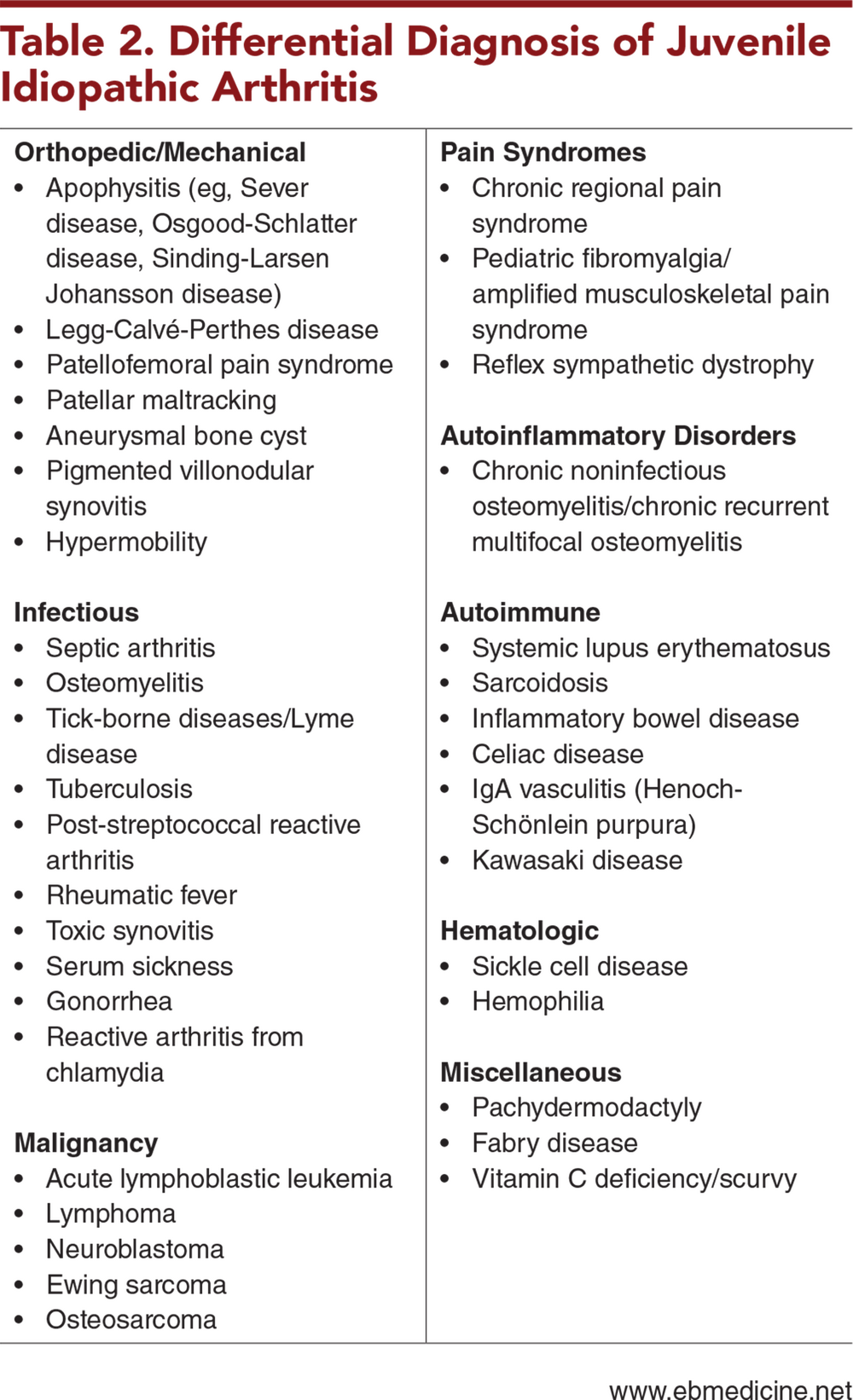
Common causes of joint pain including mechanical etiologies, infectious etiologies, malignancies, chronic pain syndromes, and autoimmune diseases
Historical findings that can aid in diagnosing JIA and key aspects of the physical examination for patients with suspected JIA
Useful laboratory studies to obtain for patients with known or suspected JIA
Which imaging studies can be useful in further characterizing arthritis in patients who may have a difficult joint examination
Recommendations for treatment of JIA flares and management of JIA in cases of infection
Which patients with JIA can be managed in the outpatient setting and which need to be admitted
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Complications of Juvenile Idiopathic Arthritis
- Riziform Bodies
- Temporomandibular Joint Arthritis
- Macrophage Activation Syndrome
- Uveitis
- Vulnerability to Infection
- Differential Diagnosis
- Mechanical Etiologies
- Infectious Etiologies
- Malignancy
- Chronic Pain Syndromes
- Autoimmune Diseases
- Prehospital Care
- Emergency Department Evaluation
- Initial Presentations of Juvenile Idiopathic Arthritis
- History
- Children With Known Juvenile Idiopathic Arthritis
- Systemic-Onset Juvenile Idiopathic Arthritis
- Physical Examination
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Treatment
- Flares of Juvenile Idiopathic Arthritis
- Nonsteroidal Anti-Inflammatory Drugs
- Corticosteroids
- Disease-Modifying Anti-Rheumatic Drugs
- Adjunctive Therapies
- Surgical Management
- Management of Juvenile Idiopathic Arthritis in Cases of Infection
- Special Populations
- Controversies and Cutting Edge
- Adult Transitional Care for Patients With Juvenile Idiopathic Arthritis
- Shortage of Pediatric Rheumatologists
- Disposition
- Summary
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Management of Patients With Juvenile Idiopathic Arthritis
- Case Conclusions
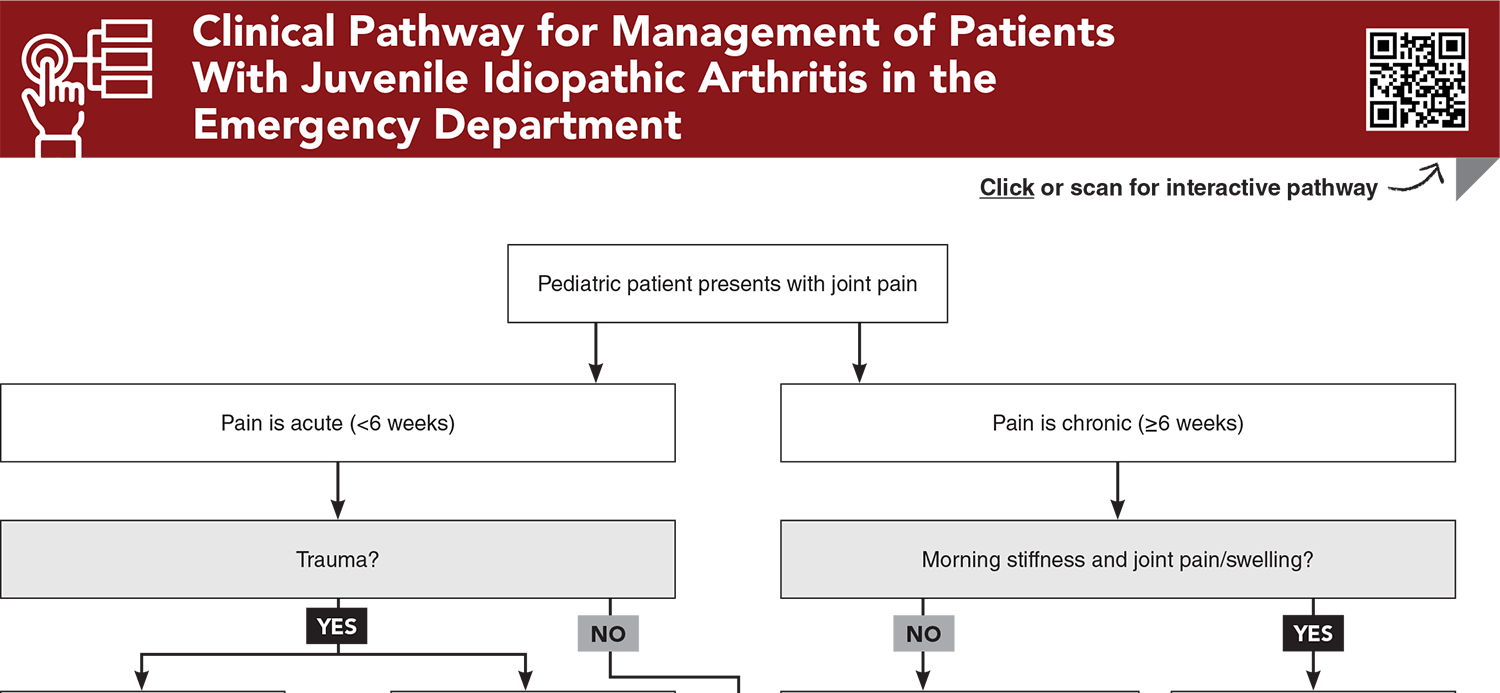
- Clinical Pathway for Management of Patients With Juvenile Idiopathic Arthritis in the Emergency Department
- Tables and Figures
- References
Abstract
Juvenile idiopathic arthritis (JIA) is the most common pediatric rheumatic disease. Children may present to the emergency department during the initial presentation of JIA or due to disease-related complications. Differentiating JIA from emergent causes of joint pain, including severe infections and malignancies, can be challenging. This issue reviews the clinical presentation of JIA, provides guidance for differentiating JIA from conditions with similar presentations, and offers recommendations for management of JIA and JIA-related complications in the emergency department.
Case Presentations
- The mother says that the child has been limping for the past week. The limping is worse when the girl first wakes up and improves as the day progresses. Her mother denies constitutional symptoms.
- On examination, you note bilateral swollen knees and ankles, with an inability to completely flex or extend at these joints. The girl’s vital signs and the rest of her physical examination are normal. Upon further questioning, the mother also tells you the girl has been eating less.
- Laboratory work in the ED reveals mildly elevated inflammatory markers. Imaging with joint ultrasound reveals effusions and synovial hyperemia.
- Should you be concerned for a joint infection? Should you consider other testing such as synovial fluid analysis or magnetic resonance imaging?
- The boy tells you that his left lower extremity pain is the most severe, and he has difficulty bearing weight. He denies any recent trauma, travel, or infections. He has not had any fevers.
- His vital signs and physical examination are largely unremarkable. The patient refuses examination of his left lower extremity and reports pain to light touch. You also notice some edema in his left lower extremity, with some blue discoloration.
- You order x-rays and laboratory studies, which are negative. The boy is given a dose of ketorolac and a dose of methylprednisolone, but neither medication helps his pain.
- The patient says the pain is severe, and he is requesting stronger pain medications. What is your next step in his management?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Patients With Juvenile Idiopathic Arthritis in the Emergency Department
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * McCurdy D, Parsa MF. Updates in juvenile idiopathic arthritis. Adv Pediatr. 2021;68:143-170. (Review) DOI: 10.1016/j.yapd.2021.05.014
7. * Zaripova LN, Midgley A, Christmas SE, et al. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021;19(1):135. (Review) DOI: 10.1186/s12969-021-00629-8
28. * Sur LM, Gaga R, Duca E, et al. Different chronic disorders that fall within the term juvenile idiopathic arthritis. Life (Basel). 2021;11(5):398. (Case report) DOI:10.3390/life11050398
33. * Dougherty BL, Zelikovsky MA, Miller KS et al. Longitudinal impact of parental catastrophizing on child functional disability in pediatric amplified musculoskeletal pain. J Ped Psych. 2021; 46(4) 476-484 (Prospective study that reviewed archival data; 155 children, 158 parents) DOI: 10.1093/jpepsy/jsaa127
Subscribe to get the full list of 51 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: juvenile idiopathic arthritis, JIA, pediatric arthritis, oligoarticular JIA, polyarticular JIA, macrophage activation syndrome, enthesitis-related arthritis, systemic-onset JIA, undifferentiated arthritis, temporomandibular joint arthritis, TMJ arthritis, micrognathia, rheumatic disease, joint pain, riziform bodies, rice bodies, uveitis, inflammatory arthritis, synovial cyst, synovitis, disease-modifying anti-rheumatic drugs, DMARD, synovectomy, chronic regional pain syndromes, CRPS, amplified musculoskeletal pain syndromes, AMPS, pediatric fibromyalgia, transitional care