Table of Contents
About This Issue
Acute mesenteric ischemia (AMI) is a potentially catastrophic cause of abdominal pain that is likely underdiagnosed in ED patients due to its sometimes vague and variable symptoms. AMI is commonly due to atherosclerotic occlusive disease, and its underlying etiology is thromboembolic. In most cases, urgent referral will be required, although managing only a patient’s cardiac comorbidities may mask their dangerous mesenteric ischemia. In this issue you will learn:
The 4 types and causes of AMI and their changing prevalence
How abdominal pain in AMI can be differentiated from other presentations on the differential
How to determine whether the mesenteric ischemia is subacute, acute, chronic, or acute-on-chronic
The risk factors in patients with AMI: thromboembolic disease, atrial fibrillation, low-flow states, valvular heart disease, volume depletion, and use of vasoconstrictive agents
The value of laboratory testing for patients with suspected AMI
The imaging recommendations for prompt diagnosis
The “11 As of AMI”
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Mesenteric Artery Embolism
- Mesenteric Artery Thrombosis
- Mesenteric Venous Thrombosis
- Nonocclusive Mesenteric Ischemia
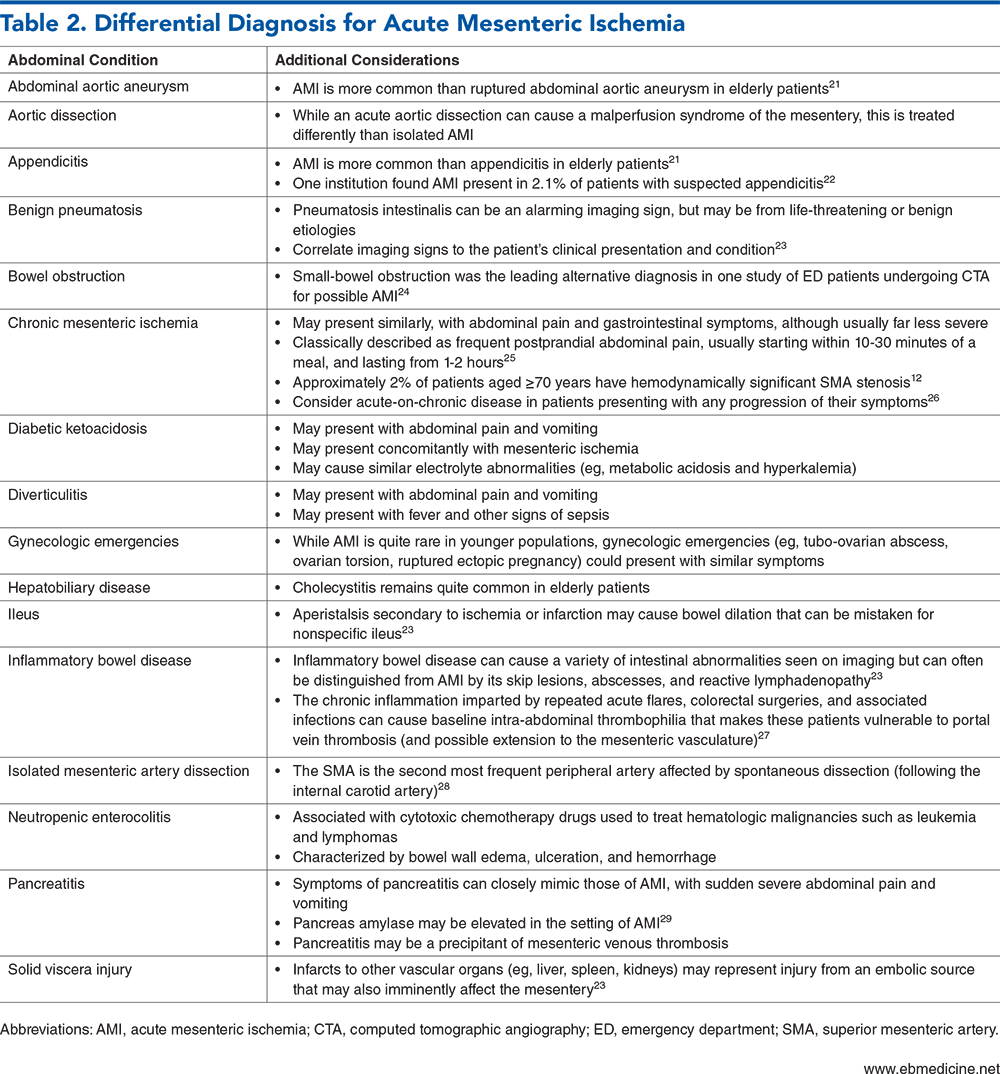
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Mesenteric Artery Embolism
- Mesenteric Artery Thrombosis
- Mesenteric Venous Thrombosis
- Nonocclusive Mesenteric Ischemia
- Physical Examination
- Pitfalls During Evaluation
- Diagnostic Studies
- Laboratory Testing
- White Blood Cell Count
- Metabolic Panel
- Lactate
- D-Dimer
- Other Laboratory Studies
- Imaging Studies
- Computed Tomography
- Arterial Thromboembolic Events on Computed Tomography
- Mesenteric Venous Thrombosis on Computed Tomography
- Nonocclusive Mesenteric Ischemia on Computed Tomographic Imaging
- Use of Intravenous Contrast
- Contrast-Enhanced Computed Tomographic Imaging
- Plain Film Radiography
- Ultrasound
- Magnetic Resonance Imaging
- Treatment
- Aggressive Fluid Administration
- Address Metabolic Derangements
- Antibiotics
- Anticoagulation
- Analgesia
- Avoidance of Vasopressors
- Alleviate Stomach
- Avoid Supraphysiologic Oxygenation
- Advance Directives
- Abdominal Compartment Syndrome
- “All the Help”
- Transmural Ischemia
- Mesenteric Venous Thrombosis
- Nonocclusive Mesenteric Ischemia
- Special Circumstances/Populations
- Pediatric Patients
- Pregnant Patients
- Older Adults
- Controversies and Cutting Edge
- Disposition
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Management of Acute Mesenteric Ischemia
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
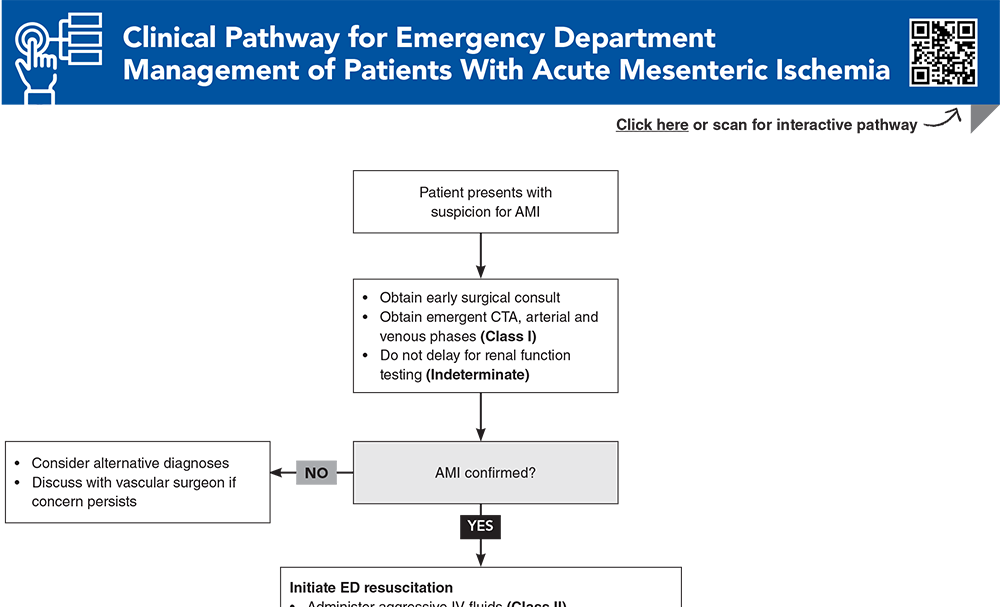
- Clinical Pathway for Emergency Department Management of Patients With Acute Mesenteric Ischemia
- Tables and Figures
- References
Abstract
Acute mesenteric ischemia is a rare but potentially catastrophic condition, and survival is highly dependent on timely diagnosis in the emergency department. Symptoms can be both variable and subtle. Laboratory studies may be misleading and may provide either false reassurance or misdirection. This review includes evidence-based recommendations on the recognition of the 4 separate types of acute mesenteric ischemia, current guidelines on the diagnostic approach, and essential resuscitative steps that should be initiated in the emergency department.
Case Presentations
- The patient states that she was previously diagnosed with atrial fibrillation, but she never established care due to concerns about the cost of anticoagulation medication.
- Her temperature is 37˚C; blood pressure, 156/90 mm Hg; heart rate, 110 beats/min; respiratory rate, 20 breaths/min; and oxygen saturation, 96% on room air.
- On physical examination, you note that despite the patient reporting severe abdominal pain, she does not seem to have any significant tenderness or guarding. Her laboratory test results are notable for mild acute kidney injury but no leukocytosis or lactic acidosis.
- You wonder whether these laboratory tests have sufficiently ruled out acute mesenteric ischemia. If not, is it still reasonable to move forward with CT imaging?
- The family informs you that he has been experiencing abdominal pain and losing weight for at least the past 6 months, although it seems to have worsened over the past few days, and he has simultaneously become quite ill.
- His temperature is 38.5˚C; blood pressure, 84/52 mm Hg; heart rate, 100 beats/min; respiratory rate, 24 breaths/min; and oxygen saturation, 93% on room air. On examination, he is ill-appearing and oriented to name only. His abdomen appears moderately distended and is tender to palpation.
- You wonder whether this could represent acute mesenteric ischemia, and what treatment you should implement immediately…
- The patient became hypotensive a couple of hours ago, and he was started on peripheral norepinephrine. The patient’s recent lactate measurements have been increasing.
- On examination, you note that he is sedated and unable to provide significant history. His abdomen appears to be mildly distended, with hypoactive bowel sounds and possibly some tenderness.
- You wonder what additional resuscitative measures you could take in the ED, and whether any advanced therapies might benefit this patient…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Patients With Acute Mesenteric Ischemia
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
13. * Bala M, Catena F, Kashuk J, et al. Acute mesenteric ischemia: updated guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2022;17(1):54. (Guideline) DOI: 10.1186/s13017-022-00443-x
36. * Acosta S, Salim S. Management of acute mesenteric venous thrombosis: a systematic review of contemporary studies. Scand J Surg. 2021;110(2):123-129. (Systematic review; 11 studies) DOI: 10.1177/1457496920969084
48. * Cudnik MT, Darbha S, Jones J, et al. The diagnosis of acute mesenteric ischemia: a systematic review and meta-analysis. Acad Emerg Med. 2013;20(11):1087-1100. (Systematic review; 23 studies) DOI: 10.1111/acem.12254
51. * Björck M, Koelemay M, Acosta S, et al. Editor’s choice - management of the diseases of mesenteric arteries and veins: clinical practice guidelines of the European Society of Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2017;53(4):460-510. (Guideline) DOI: 10.1016/j.ejvs.2017.01.010
64. * Tilsed JV, Casamassima A, Kurihara H, et al. ESTES guidelines: acute mesenteric ischaemia. Eur J Trauma Emerg Surg. 2016;42(2):253-270. (Guideline) DOI: 10.1007/s00068-016-0634-0
72. * Ginsburg M, Obara P, Lambert DL, et al. ACR Appropriateness Criteria(®) Imaging of Mesenteric Ischemia. J Am Coll Radiol. 2018;15(11s):S332-S340. (Guideline) DOI: 10.1016/j.jacr.2018.09.018
74. * Lehtimäki TT, Kärkkäinen JM, Saari P, et al. Detecting acute mesenteric ischemia in CT of the acute abdomen is dependent on clinical suspicion: review of 95 consecutive patients. Eur J Radiol. 2015;84(12):2444-2453. (Retrospective; 95 patients) DOI: 10.1016/j.ejrad.2015.09.006
100. *Roussel A, Castier Y, Nuzzo A, et al. Revascularization of acute mesenteric ischemia after creation of a dedicated multidisciplinary center. J Vasc Surg. 2015;62(5):1251-1256. (Prospective observational; 83 patients) DOI: 10.1016/j.jvs.2015.06.204
101. *Brennan CA, Osei-Bonsu P, McClenaghan RE, et al. Vasoactive agents in acute mesenteric ischaemia in critical care. A systematic review. F1000Res. 2021;10:453. (Systematic review; 0 studies) DOI: 10.12688/f1000research.52782.2
115. *Reintam Blaser A, Starkopf J, Björck M, et al. Diagnostic accuracy of biomarkers to detect acute mesenteric ischaemia in adult patients: a systematic review and meta-analysis. World J Emerg Surg. 2023;18(1):44. (Systematic review; 75 studies) DOI: 10.1186/s13017-023-00512-9
Subscribe to get the full list of 120 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: embolism, thrombosis, bowel, infarction, ischemia, aorta, superior, inferior, nonocclusive, pancreatitis, vasoconstrictive, lactate, transmural