Table of Contents
About This Issue
Abdominal pain is one of the most common presentations in the ED, and 2 common causes are appendicitis and diverticulitis. These intra-abdominal infections present challenges in diagnosis and management for emergency clinicians, and choices and evidence for treatment with antibiotics and/or surgery can be conflicting. In this issue you will learn:
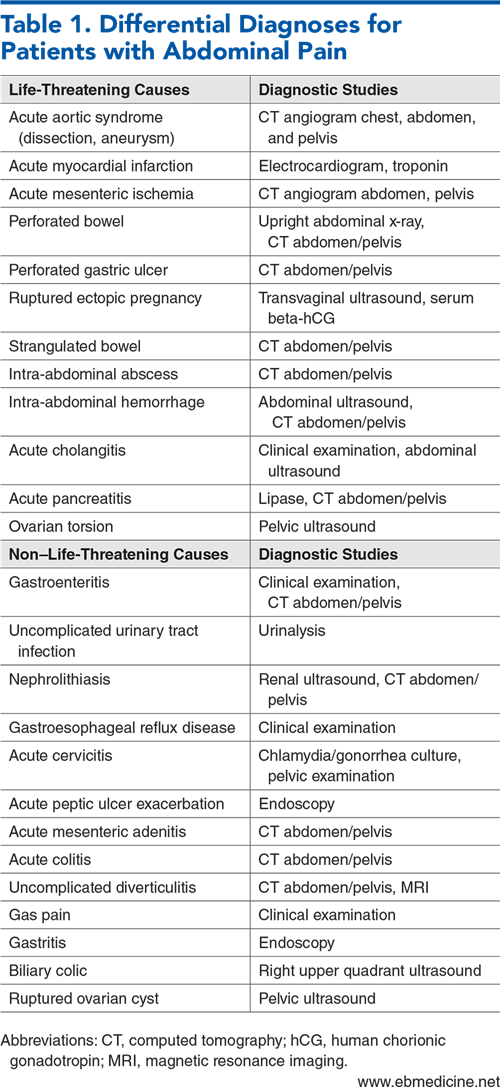
The life-threatening and non-life-threatening causes on the differential for abdominal pain
What the recommended laboratory studies are for appendicitis that have the highest levels of diagnostic value
Which appendicitis scoring system has the highest sensitivity and specificity: AIR, Alvarado, RIPASA, or AAS
Ultrasound, CT, or MRI: when each is called for when there is suspicion for intra-abdominal infection
Antibiotics-only approach for appendicitis: what is the evidence, and when can it be appropriate?
Determining whether diverticulitis is complicated or uncomplicated and staging the disease to dictate treatment strategies
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Appendicitis
- Diverticular Disease
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Likelihood Ratios for Signs and Symptoms
- Physical Examination
- Diagnostic Studies for Appendicitis
- Laboratory Studies for Acute Appendicitis
- Scoring Systems for Diagnosis of Acute Appendicitis
- Imaging Studies for Acute Appendicitis
- Abdominal Ultrasound
- Computed Tomography
- Magnetic Resonance Imaging
- Diagnostic Studies for Diverticulitis
- Laboratory Studies for Acute Diverticulitis
- Imaging Studies for Diverticulitis
- Computed Tomography
- Ultrasound
- Magnetic Resonance Imaging
- Treatment
- Appendicitis Treatment
- Medical Management
- Surgical Management
- Diverticulitis Treatment
- Uncomplicated Diverticulitis
- Complicated Diverticulitis
- Special Populations
- Elderly Patients
- Acute Appendicitis in Elderly Patients
- Diverticulitis in Elderly Patients
- Pregnant Patients
- Acute Appendicitis In Pregnant Patients
- Diverticulitis in Pregnant Patients
- Imaging for Diverticulitis in Pregnant Patients
- Antibiotic Use in Pregnant Patients
- Pediatric Patients
- Appendicitis in Pediatric Patients
- Diverticulitis in Pediatric Patients
- Controversies and Cutting Edge
- Antibiotics-Only Approach for Treatment of Acute Appendicitis
- Antibiotics in Acute Uncomplicated Diverticulitis
- Disposition
- Acute Appendicitis
- Acute Diverticulitis
- Summary
- Time- and Cost-Effective Strategies
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Management of Suspected Intra-Abdominal Infections
- Case Conclusions
- Clinical Pathways
- World Society of Emergency Surgery Clinical Pathway for Management of Patients With Suspected Acute Appendicitis
- Clinical Pathway for Emergency Department Management of Pregnant Patients With Suspected Acute Appendicitis
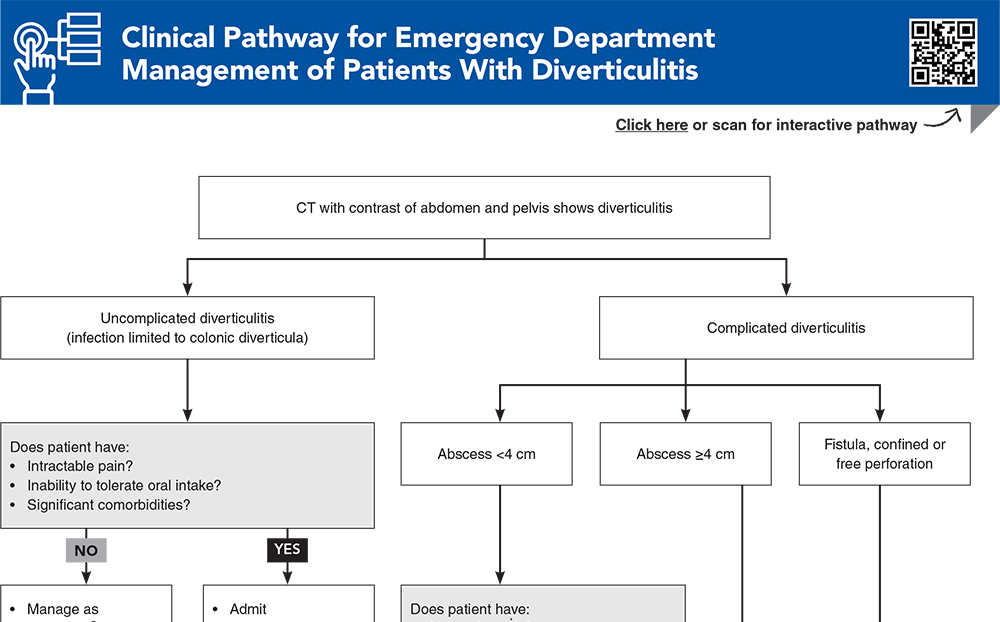
- Clinical Pathway for Emergency Department Management of Patients With Diverticulitis
- Tables and Figures
- References
Abstract
Abdominal pain is one of the most common presenting complaints to the emergency department, and appendicitis and diverticulitis are common causes. Intra-abdominal infections have historically been managed with admission to the hospital, antibiotics, and surgical interventions, and best-practice pathways are an important part of quality programs. Advances in diagnostics and management, supported with outcome data, are impacting care pathways. This review provides an update on best practices related to the management of appendicitis and diverticulitis, with the goal of improving patient care, minimizing risk, and maximizing the patient experience.
Case Presentations
- The patient says he’s had a slight fever at home. His current vital signs are: temperature, 38.2ºC; heart rate, 108 beats/min; blood pressure, 122/70 mm Hg; and respiratory rate, 14 breaths/min.
- On palpation, his abdomen is soft and not distended, with tenderness to palpation in the periumbilical area and right lower quadrant. Bowel sounds are present.
- You order a urinalysis, complete blood cell (CBC) count, basic metabolic panel (BMP), liver function tests (LFTs), and lipase level, and administer IV morphine, IV crystalloid fluids, and antipyretics.
- You have high suspicion for appendicitis and consider what type of imaging should be ordered. You wonder: do scoring systems really work? And if it is appendicitis, can you send this patient home on oral antibiotics?
- Her vital signs are: temperature, 37.4ºC; heart rate, 93 beats/min; blood pressure, 145/84 mm Hg; and respiratory rate, 16 breaths/min.
- You order a urinalysis, CBC, BMP, LFTs, and lipase level, and give her pain medication and antiemetics.
- Her laboratory results return as normal, and her symptoms improve slightly.
- You consider whether you should order a CT scan to look for complications, or discharge her, without antibiotics, for outpatient follow-up…
- The patient reports subjective fever, chills, nausea, and decreased appetite over the last 3 days.
- Her current vital signs are: temperature, 37.9ºC; heart rate, 112 beats/min; blood pressure, 118/82 mm Hg; and respiratory rate, 18 breaths/min.
- You suspect acute appendicitis, and consider what the best imaging options are. Should you start with ultrasound, or order an MRI? What if she has a contraindication to MRI?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Emergency Department Management of Patients With Diverticulitis
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
6. * Sartelli M, Weber DG, Kluger Y, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15(1):32. (Guidelines) DOI: 10.1186/s13017-020-00313-4
40. * Rud B, Vejborg TS, Rappeport ED, et al. Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database Syst Rev. 2019(11):CD009977. (Cochrane review; 64 studies, 10,280 patients) DOI: 10.1002/14651858.CD009977.pub2
43. * Repplinger MD, Levy JF, Peethumnongsin E, et al. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging. 2016;43(6):1346-1354. (Meta-analysis; 10 studies, 838 patients) DOI: 10.1002/jmri.25115
44. * D’Souza N, Hicks G, Beable R, et al. Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database Syst Rev. 2021(12):CD012028. (Cochrane review; 58 studies, 7462 patients) DOI: 10.1002/14651858.CD012028.pub2
48. * Expert Panel on Gastrointestinal Imaging, Weinstein S, Kim DH, et al. ACR appropriateness criteria® left lower quadrant pain: 2023 update. J Am Coll Radiol. 2023;20(11S):S471-S480. (Guidelines) DOI: 10.1016/j.jacr.2023.08.013
53. * Lameris W, van Randen A, Bipat S, et al. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008;18(11):2498-2511. (Meta-analysis; 14 studies, 1314 patients) DOI: 10.1007/s00330-008-1018-6
64. * Fugazzola P, Ceresoli M, Coccolini F, et al. The WSES/SICG/ACOI/SICUT/ACEMC/SIFIPAC guidelines for diagnosis and treatment of acute left colonic diverticulitis in the elderly. World J Emerg Surg. 2022;17(1):5. (Guidelines) DOI: 10.1186/s13017-022-00408-0
81. * Di Saverio S, Sibilio A, Giorgini E, et al. The NOTA study (Non Operative Treatment for Acute appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg. 2014;260(1):109-117. (Prospective study; 159 patients) DOI: 10.1097/SLA.0000000000000560
86. * Dichman ML, Rosenstock SJ, Shabanzadeh DM. Antibiotics for uncomplicated diverticulitis. Cochrane Database Syst Rev. 2022;6(6):CD009092. (Cochrane review; 5 studies) DOI: 10.1002/14651858.CD009092.pub3
Subscribe to get the full list of 93 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: abdominal, appendicitis, diverticulitis, abscess, peritonitis, AIR, Alvarado, ultrasound, appendicolith, antibiotics