Table of Contents
About This Issue
Injuries to the eye can be very stressful for patients. This issue discusses the mechanisms of common traumatic ocular injuries that may present to an urgent care setting and their evaluation recommendations. Knowledge of the appropriate management and disposition of ocular injuries can help the urgent care clinician provide the best chance for a favorable visual outcome. In this issue, you will learn:
The mechanisms of injury of common ocular injuries;
A systematic approach to the physical examination and diagnostic elements available in the urgent care setting to diagnose traumatic ocular injuries;
The most current treatment recommendations; and
The disposition of traumatic ocular injuries to the globe, including those that require outpatient and emergent referral for further evaluation and treatment.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Etiology and Pathophysiology
- Differential Diagnosis
- Urgent Care Evaluation
- History
- Physical Examination
- Visual Acuity Testing
- Fluorescein Examination
- Indications for pH Testing
- The Multiply Injured Patient
- Proptosis and Retrobulbar Hemorrhage
- Diagnostic Studies
- Laboratory Studies
- Plain Radiography
- Computed Tomography
- Treatment
- Corneal Foreign Body
- Corneal Abrasion
- Corneal Flash Burns
- Open-Globe Injuries
- Traumatic Hyphema
- Traumatic Iritis
- Ocular Chemical Burns
- Retinal Detachment, Posterior Vitreous Detachment, Vitreous Hemorrhage, and Lens Dislocation
- Retrobulbar Hemorrhage
- Disposition
- Corneal Foreign Body or Abrasion
- Traumatic Hyphema
- Ocular Burn
- Retrobulbar Hemorrhage
- Other Injuries
- Special Populations
- Contact Lens Wearers
- Patients Taking Anticoagulants and Antiplatelet Agents
- Controversies and Cutting Edge
- Ultrasound
- Lateral Canthotomy Training
- Topical Anesthetics for Corneal Abrasion
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
- Risk Management Pitfalls in the Urgent Care Evaluation and Management of Ocular Injuries
- KidBits: Pediatric Considerations for Urgent Care Management of Ocular Injuries
- Evaluation and Diagnosis
- Treatment of Common Conditions
- Corneal Abrasion
- Foreign Body
- Subconjunctival Hemorrhage
- Minor Eyelid Injuries and Blunt Trauma
- Summary
- References
- Acknowledgement
- Coding & Charting: What You Need to Know
- Determining the Level of Service
- Problems Addressed
- Complexity of Data
- Risk of Patient Management
- Documentation Tips
- Coding Challenge: Managing Ocular Injuries in Urgent Care
- Acknowledgement
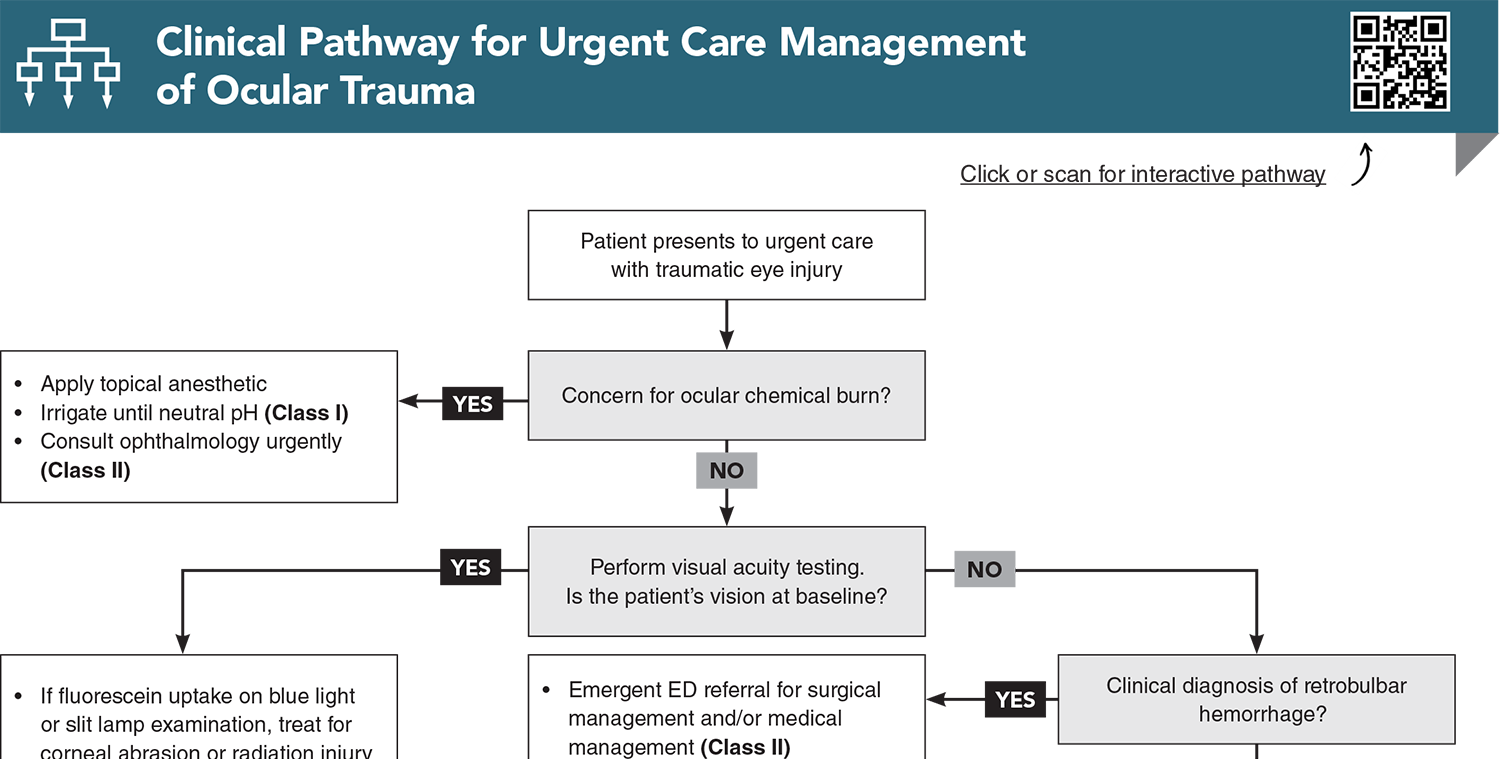
- Clinical Pathway for Urgent Care Management of Ocular Trauma
- References
Abstract
Patients with ocular injuries are commonly seen in the urgent care clinic, and these injuries are the most frequent cause of noncongenital monocular blindness in children and adults. Systematic evaluation and management will ensure that they have the best chance for a favorable final visual outcome. This review provides evidence-based recommendations for the diagnosis, treatment, and disposition of patients with common ocular injuries presenting in the urgent care setting, as well as an overview of more serious injuries that occasionally present to the urgent care that require specialist or emergency department referral.
Case Presentations
- She immediately began irrigation but continues to complain of pain and decreased vision in the eye.
- After a quick gross examination and pH testing, you administered tetracaine eye drops to the affected eye and initiated immediate irrigation with lactated Ringer’s solution and a commercially available irrigation scleral lens device.
- After 30 minutes of irrigation, the patient feels better. The pH of her eye is 7.4.
- You wonder if you should refer this patient to an ophthalmologist…
- He was wearing eye protection while doing the grinding but did remove his glasses at times and notes that “metal dust was everywhere.”
- He complains of a foreign body sensation and eye irritation.
- He has no significant eye problems and does not wear glasses or contact lenses.
- Gross eye examination shows mild conjunctival injection but is otherwise normal and no abrasion or foreign body is seen. Visual acuity of 20/30 OD, 20/20 OS, and 20/20 OU.
- As you are about to write a prescription for erythromycin eye ointment, the patient asks, "Are you going to put that yellow stuff in my eye like they did last time this happened?”
- She says she feels like something is in her eye and states, "It’s really irritating."
- Her eye is watering, and she feels like her vision is blurry. Symptoms continued even after she removed her contact lenses an hour ago.
- She was not wearing glasses or any eye protection while gardening but did not specifically get the sense that something went into her eye at any time.
- She complains of moderate pain and light sensitivity in addition to the sense of something in her eye.
- You wonder if this is a simple case of foreign body with corneal abrasion...
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Urgent Care Management of Ocular Trauma
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
7. * Scott R. The injured eye. Philos Trans R Soc Lond B Biol Sci. 2011;366(1562):251-260. (Review) DOI: 10.1098/rstb.2010.0234
11. * Khaw PT, Shah P, Elkington AR. Injury to the eye. BMJ. 2004;328(7430):36-38. (Review) DOI: 10.1098/rstb.2010.0234
22. * Brandt MT, Haug RH. Traumatic hyphema: a comprehensive review. J Oral Maxillofac Surg. 2001;59(12):1462-1470. (Review) DOI: 10.1016/j.disamonth.2014.03.004
26. * Perry M, Moutray T. Advanced Trauma Life Support (ATLS) and facial trauma: can one size fit all? Part 4: 'Can the patient see?’ Timely diagnosis, dilemmas and pitfalls in the multiply injured, poorly responsive/unresponsive patient. Int J Oral Maxillofac Surg. 2008;37(6):505-514. (Review) DOI: 10.1016/j.ijom.2007.11.004
38. * Wipperman JL, Dorsch JN. Evaluation and management of corneal abrasions. Am Fam Physician. 2013;87(2):114-120. (Review)
65. * Roque PJ, Hatch N, Barr L, et al. Bedside ocular ultrasound. Crit Care Clin. 2014;30(2):227-241. (Overview) DOI: 10.1016/j.ccc.2013.10.007
74. * Green SM, Tomaszewski C, Valente JH, et al. Use of topical anesthetics in the management of patients with simple corneal abrasions: consensus guidelines from the American College of Emergency Physicians. Ann Emerg Med. 2024;83(5):477-489. (Consensus-based expert guideline) DOI: 10.1016/j.annemergmed.2024.01.004
Subscribe to get the full list of 77 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: eye, ocular, traumatic ocular injuries, corneal foreign body, fluorescein, corneal abrasion, intraocular pressure, tonometry, visual acuity, Snellen chart, retrobulbar hemorrhage, open-globe injury, traumatic hyphema, ocular chemical burn, rust ring, ophthalmology, traumatic iritis, corneal flash burn, subconjunctival hemorrhage, corneal ulcer, irrigation, eye protection, photokeratitis, retinal detachment, vitreous detachment, lens dislocation, proptosis, ecchymosis, eye shield, ocular ultrasound, lateral canthotomy